Abstract
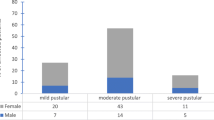
This study aimed to compare the antimicrobial activities of topical agents against Propionibacterium acnes isolated from patients admitted to a hospital in Shanghai, China. The minimal inhibitory concentrations of the cultured P. acnes were determined in accordance with the Clinical and Laboratory Standards Institute. Susceptibilities to clindamycin and erythromycin were compared in terms of gender, age, disease duration, previous treatment, and disease severity. A total of 69 P. acnes strains were isolated from 98 patients (70.41%). The susceptibility to triple antibiotic ointment (neomycin/bacitracin/polymyxin B) and bacitracin was 100%. The susceptibility to fusidic acid was 92.7%. The resistance rates to neomycin sulfate, erythromycin, and clindamycin were 11.7%, 49.3%, and 33.4%, respectively. The high resistance rate to clindamycin and erythromycin was significantly affected by gender, previous treatment, and disease severity rather than by age and disease duration. Topical antibiotics should not be used separately for long-term therapy to avoid multiresistance. The use of topical antibiotics should be determined by clinicians on the basis of clinical conditions.
Similar content being viewed by others
References
Beylot C, Auffret N, Poli F, Claudel JP, Leccia MT, Del Giudice P, Dreno B. Propionibacterium acnes: an update on its role in the pathogenesis of acne. J Eur Acad Dermatol Venereol 2014; 28(3): 271–278
Haider A, Shaw JC. Treatment of acne vulgaris. JAMA 2004; 292(6): 726–735
Ross JI, Snelling AM, Carnegie E, Coates P, Cunliffe WJ, Bettoli V, Tosti G, Katsambas A, Galvan Peréz Del Pulgar JI, Rollman O, Török L, Eady EA, Cove JH. Antibiotic-resistant acne: lessons from Europe. Br J Dermatol 2003; 148(3): 467–478
Gollnick H, Cunliffe W, Berson D, Dreno B, Finlay A, Leyden JJ, Shalita AR, Thiboutot D; Global Alliance to Improve Outcomes in Acne. Management of acne: a report from a Global Alliance to Improve Outcomes in Acne. J Am Acad Dermatol 2003; 49(1 Suppl): S1–S37
Bonomo RA, Van Zile PS, Li Q, Shermock KM, McCormick WG, Kohut B. Topical triple-antibiotic ointment as a novel therapeutic choice in wound management and infection prevention: a practical perspective. Expert Rev Anti Infect Ther 2007; 5(5): 773–782
Cesur S. Topical antibiotics and clinical use. Mikrobiyol Bul 2002; 36(3-4): 353–361
Khorvash F, Abdi F, Kashani H H, Fatemi Naeini F, Khorvash F. Efficacy of mupirocin and rifampin used with standard treatment in the management of acne vulgaris. Iran J Pharm Res 2013; 12(1): 223–227
Ramli R, Malik AS, Hani AF, Jamil A. Acne analysis, grading and computational assessment methods: an overview. Skin Res Technol 2012; 18(1): 1–14
Dreno B, Gollnick HP, Kang S, Thiboutot D, Bettoli V, Torres V, Leyden J. Understanding innate immunity and inflammation in acne: implications for management. J Eur Acad Dermatol Venereol 2015; 29(Suppl 4): 3–11
Rathi SK. Acne vulgaris treatment: the current scenario. Indian J Dermatol 2011; 56(1): 7–13
Del Rosso JQ, Kim GK. Topical antibiotics: therapeutic value or ecologic mischief? Dermatol Ther (Heidelb) 2009; 22(5): 398–406
Tan HH. Antibacterial therapy for acne: a guide to selection and use of systemic agents. Am J Clin Dermatol 2003; 4(5): 307–314
Aubin GG, Portillo ME, Trampuz A, Corvec S. Propionibacterium acnes, an emerging pathogen: from acne to implant-infections, from phylotype to resistance. Med Mal Infect 2014; 44(6): 241–250
Del Rosso J. Emerging topical antimicrobial options for mild-tomoderate acne: a review of the clinical evidence. J Drugs Dermatol 2008; 7(2 Suppl): s2–s7
Tanghetti E. The impact and importance of resistance. Cutis 2007; 80(1 Suppl): 5–9
Yun HJ, Lee SW, Yoon GM, Kim SY, Choi S, Lee YS, Choi EC, Kim S. Prevalence and mechanisms of low- and high-level mupirocin resistance in staphylococci isolated from a Korean hospital. J Antimicrob Chemother 2003; 51(3): 619–623
Bonamonte D, Belloni Fortina A, Neri L, Patrizi A. Fusidic acid in skin infections and infected atopic eczema. G Ital Dermatol Venereol 2014; 149(4): 453–459
Williamson DA, Monecke S, Heffernan H, Ritchie SR, Roberts SA, Upton A, Thomas MG, Fraser JD. High usage of topical fusidic acid and rapid clonal expansion of fusidic acid-resistant Staphylococcus aureus: a cautionary tale. Clin Infect Dis 2014; 59(10): 1451–1454
Author information
Authors and Affiliations
Corresponding author
Additional information
These authors contributed equally to this work.
Rights and permissions
About this article
Cite this article
Ma, Y., Zhang, N., Wu, S. et al. Antimicrobial activity of topical agents against Propionibacterium acnes: an in vitro study of clinical isolates from a hospital in Shanghai, China. Front. Med. 10, 517–521 (2016). https://doi.org/10.1007/s11684-016-0480-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11684-016-0480-9