Abstract
Introduction
Traumatic anterior shoulder dislocation occurs frequently and usually affects young, active male patients. Detachment of the anteroinferior labrum, known as the Bankart lesion, is a common result. However, more extensive entities including bony lesions and disruptions of the labral ring can also be found. The aim of the present work was to analyze all cases of first-time traumatic anterior shoulder dislocation at a level‑1 trauma center with regard to the type of labral lesion. Focus was placed on the frequency and distribution of complex lesions and the extent of the surgical repair.
Patients and methods
The clinical database of a level‑1 trauma center with a specialized shoulder unit was searched to identify all patients with first-time anterior shoulder dislocation treated between 2015 and 2019. Of 224 patients, 110 underwent primary surgical repair after first-time dislocation (mean age 40 years).
Results
A total of 62% of patients had only a soft tissue injury, while 38% (n = 40) showed a bony Bankart lesion/fracture of the glenoid fossa with a mean defect size of 26%. In only 31% of patients (n = 34), a classic Bankart repair was performed, whereas the remaining 69% underwent additional procedures.
Conclusion
In this series of surgically treated first-time traumatic anterior shoulder dislocations, the majority of cases presented with more complex lesions than an isolated classic Bankart lesion. The risk for bony involvement and associated pathologies, such as cuff tears and greater tuberosity fracture, increases with age and requires a more extensive surgical approach. Disruption of the labral ring was frequently found in both soft tissue and bony lesions and directly affected the surgical procedure.
Zusammenfassung
Einleitung
Die traumatische vordere Schulterluxation ist eine häufige Verletzung, die in der Regel junge, aktive männliche Patienten betrifft. Die klassische Bankart-Läsion ist die häufigste Folge. Aber auch ausgedehntere Schäden wie etwa knöcherne Bankart-Läsionen und Risse des labralen Rings kommen vor. Ziel der vorliegenden Arbeit war es, alle Fälle einer traumatischen vorderen Schultererstluxation in einem Level-1-Traumazentrum hinsichtlich des Typs der Labrumläsion zu prüfen. Der Fokus lag dabei auf der Häufigkeit und Verteilung komplexer Läsionen und dem Ausmaß der operativen Wiederherstellung.
Patienten und Methoden
Die klinische Datenbank eines Level-1-Traumazentrums mit dem Bereich Schulterchirurgie wurde durchsucht, um alle zwischen 2015 und 2019 behandelten Patienten mit vorderer Schultererstluxation zu erfassen. Von 224 Patienten wurden 110 einer primären operativen Wiederherstellung nach Erstluxation unterzogen (Durchschnittsalter 40 Jahre).
Ergebnisse
Insgesamt 62 % der Patienten hatten lediglich eine Weichteilverletzung, wohingegen 38 % (n = 40) eine knöcherne Bankart-Läsion/Fraktur der Cavitas glenoidalis mit einer durchschnittlichen Defektgröße von 26 % aufwiesen. Nur 31 % der Patienten (n = 34) wurden einem klassischen Bankart-Repair unterzogen, bei den restlichen 69 % erfolgten weitere Prozeduren.
Schlussfolgerung
In dieser Serie operativ behandelter traumatischer vorderer Schultererstluxationen war die Läsion in der Mehrzahl der Fälle komplexer als eine isolierte klassische Bankart-Läsion. Das Risiko einer Knochenbeteiligung und assoziierter Läsionen wie Rotatorenmanschettenrupturen und Frakturen des Tuberculum majus nimmt mit dem Alter zu und erfordert einen umfassenderen operativen Ansatz. Ein Riss des labralen Rings war bei Weichteil- wie auch Knochenläsionen häufig und wirkte sich direkt auf das operative Vorgehen aus.
Similar content being viewed by others
Introduction
Traumatic anterior shoulder dislocation occurs frequently and usually affects young, active male patients. Commonly, a detachment of the anteroinferior labrum results [1]. This lesion is found in approximately 90% of all dislocations [2]. However, more complex entities such as bony avulsions (4–70% of all dislocations), glenoid labral articular disruption (GLAD) lesions, or extensions of the Bankart lesion into the bicpes anchor [superior labrum anterior to posterior lesions (SLAP)] are found [3,4,5,6]. In addition, concomitant injuries (i.e., fractures of the greater tuberosity) may also occur and influence the treatment strategy [7,8,9]. Hence, these injuries may also require more comprehensive surgical management with additional procedures such as screw fixation of glenoid rim fractures or rotator cuff repairs. Whereas patients with a simple capsulolabral injury are frequently operated in an outpatient setting, more complex injuries are often referred to specialized centers that provide the setup for more comprehensive procedures.
The aim of the present work, therefore, was to analyze the cases of first-time traumatic anterior shoulder dislocation that underwent surgical intervention in a level‑1 trauma center with regard to the type of lesion. Attention was paid to exact description of the labral lesion, including the integrity of the labral ring and the presence of additional bony pathologies. It was hypothesized that surgical indications for first-time dislocations are more complex with the majority of surgeries requiring more than a simple Bankart procedure.
Patients and methods
The clinical database of a German level‑1 trauma center with a specialized shoulder unit was searched by International Classification of Diseases (ICD)-10 codes in order to identify all patients with shoulder dislocation that were treated between 2015 and 2019. In total, 224 patients were identified. Of these, 110 underwent primary surgical repair after first-time dislocation, while 54 patients were treated conservatively. The remaining 60 patients had posterior or multidirectional instabilities or were revision cases. Due to the variety and diversity of reasons for the selection of conservative treatment, this has not been further analyzed within the manuscript. The focus was put on patients receiving a surgical intervention after first-time anterior shoulder dislocation. The reasons for a conservative treatment selection included patient age, activity level, absence of complaints, patient choice, or limited structural damage. All patients with first-time anterior shoulder dislocation aged over 18 years with pre-operative radiographs, magnetic resonance imaging and computed tomography scans, as well as intraoperative documentation, were included. Exclusion criteria included prior dislocations, posterior or multidirectional instability, revision cases, and patients that were treated conservatively as intraoperative imaging was required for a valid analysis of structural pathologies. Image evaluation was performed blinded and all names were converted to ID codes for data security reasons. Furthermore, three individual raters analyzed the images separately. In cases of questionable findings, consent of all three raters was achieved by open discussion.
Soft tissue injuries
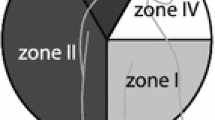
The definitive classification of soft tissue injuries was based on intraoperative imaging (photo and video documentation of all arthroscopic and open procedures) and the surgical reports (i.e. classic Bankart lesions, SLAP lesions, GLAD lesions) analyzed by three individual raters. The extent of the labral lesions was described as the position on a clock displayed for a right shoulder. Intraoperative images and documentation were further assessed to descriptively specify the operative procedure. With regard to the surgical procedure, classic Bankart repair was defined as capsulolabral repair, whereas an extended Bankart repair was defined as Bankart repair with additional SLAP repair or additional fixation of bony fragments.
Additional bony injuries
The CT scans were used for adequate bony assessment. Therefore, all measurements were taken from a two-dimensional slide after multiplanar reconstruction to ensure best possible image position.
Bony Bankart lesions and glenoid rim fractures were defined as solid or multifragmentary, and the localization was also described on a clock face for the right shoulder. The length and width of the fragment were measured in the on-face view. For the length of the fragment, the maximal distance in superior–inferior dimension in line with the glenoid inclination was measured. The largest extension in the anterior–posterior dimension was defined as the width. The approximated defect size in percent was calculated by dividing the width of the fragment by the infraglenoid diameter as previously published (Fig. 1; [10, 11]).
Measurement of the defect size by dividing the width of the fragment by the infraglenoid diameter [10]
The assessment of labral ring continuity
Since it is of importance for the surgical strategy, special attention was paid to the integrity of the labral ring. In the case of a disruption of the labral ring, comparable to a complete radial meniscus tear, the exact location was also tagged on the clock for a right shoulder. The direct impact of surgical technique and surgical time was analyzed.
Statistics
Descriptive statistics were collected with the use of Microsoft excel. Comparisons between groups were performed with the t‑test where applicable.
Ethical approval was not required due to the retrospective study design without patient examinations. However, this chart review study was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Results
A total of 110 patients (89 male, 21 female) with a mean age of 40 years (19–78) were treated operatively. All patients had a capsulolabral lesion. However, in only 62% (n = 68) was a soft tissue injury isolated, whereas the remaining 38% (n = 42) sustained an additional bony Bankart lesion or a fracture of the anterior glenoid rim. Of the 68 patients with only a soft tissue injury, 34 had a “classic” Bankart lesion without extension into the biceps anchor or other soft tissue pathologies. These patients were on average 11 years younger than the overall cohort (29 ± 9.1 vs. 40 ± 14.6 years). SLAP lesions were found in 23 patients (20.9%). A SLAP 5 lesion according to Maffet [12], describing a SLAP lesion that extends into the anterior labrum down to the 6 o’clock position, was the most common type. In 20 of 23 cases, the anterior labrum was repaired in combination with a tenodesis of the long head of biceps. In the remaining three cases, a SLAP repair was performed. GLAD lesions were found in seven cases (6%) and was mostly localized between 2:30 and 4 o’clock. In GLAD lesions, the underlying bone was mircofractured and the labrum was reattached into the defect.
Bony Bankart/anterior glenoid rim fracture
A total of 42 patients (38%) had a bony avulsion/Bankart fracture. The average age of these patients was 44 ±11.2 years (21–64). The mean defect size was 26% ±9.1. Table 1 shows the distribution depending on defect size. In the majority of cases, the bony lesion started at the 2 o’clock position (n = 27) and extended inferiorly to the 6 o’clock position (Fig. 2). Open or arthroscopically assisted direct screw fixation of the fragments was performed in combination with a labral repair (extended labral repair) if fragments were solitary (type 1b according to Scheibel; [4]). These defects were 36% of the glenoid surface on average. Smaller fragments were indirectly fixed by incorporating them into a classic Bankart repair using suture anchors or extended repairs using the bony Bankart bridge technique [13,14,15]. The operation time in cases with bony involvement was approximately twice as long as in isolated soft tissue injuries (77 vs. 133 min; p < 0.005).
Labral ring disruption
The labral ring was disrupted (meaning a complete radial tear) in 20 cases (18%). An anterior glenoid fracture was more frequently associated with labral ring disruption than soft tissue injuries (23% vs. 15%). The disruption was localized between 1 and 3 o’clock in all cases. This had a direct impact on the operative strategy: In cases of labral disruption, the labral ring was closed prior to classic Bankart repair from inferior to superior (Fig. 3). In cases with bony fragments, the labral disruption was always located just superior to the fragment. In cases with bony fragments and an intact labral ring, the labrum can be used to indirectly aid in reducing the bony fragment by closure of the labrum inferior and superior to the fragment (Fig. 4). In cases with labral disruption, reduction of the bony fragments remains more complicated.
A 20-year-old patient with a Bankart lesion and a disrupted labral ring at the 2 o’clock position (a, b). The labral ring is closed (c), resulting in a “classic” Bankart lesion from the 2–6 o’clock position (d) that is subsequently repaired from inferior to superior (e, f) using knotless anchors. L labrum, G glenoid; digits, clocktime
Anterior glenoid rim fracture (a) type 1b according to Scheibel with an intact labral ring. Reconstruction is performed by inferior anchor fixation (b), screw fixation of the solid fragment (c; view from posterior, d; view from anterolateral), and final repair with labral fixation just above the bony fragment (e). Computed tomography scan 4 months after surgery demonstrates anatomic reconstruction of the glenoid (f). G glenoid, aF anterior fragment
Interestingly, the labral ring was torn in four of seven GLAD lesions.
Other associated injuries
Greater tuberosity (GT) fractures were found in 10 patients (9%). This group of patients was on average 49 ± 9.6 years of age (32–63) and therefore older than patients with isolated soft tissue injuries (29 years) and those with a glenoid fracture (42 years; p < 0.005 for both comparisons). GT fractures were equally accompanied by additional soft tissue injuries and glenoid involvement.
Furthermore, in 10 cases (9%), patients required a rotator cuff repair. Patients with cuff tears were on average 62 years old. Isolated subscapularis tears were found in four patients, whereas five presented with posterosuperior cuff lesions and the remaining two had a massive cuff tear involving the subscapularis, supraspinatus, and infraspinatus. All but one patient underwent rotator cuff repair, while one patient was treated with a reverse total shoulder arthroplasty due to preexisting arthritic changes.
Discussion
The present study evaluated surgical cases of traumatic anterior shoulder at a level‑1 trauma center with a specialized shoulder unit. The most notable results were the following:
-
The proportion of cases with bony involvement was comparatively high (38%; n = 42).
-
Only 34 patients (31%) had an isolated “classic Bankart” lesion without involvement of the biceps anchor or other associated injuries.
-
Patients with isolated soft tissue injuries were younger than those with associated lesions.
-
The labral ring was torn in 20 cases (18%), with a higher risk seen in patients with bony involvement.
Anterior shoulder dislocation is a very common injury, mostly resulting in a capsulolabral lesion and a Hill–Sachs defect [16]. While in 1923 Bankart described the avulsion of the labrum as the lesion of necessity, it does not occur in every patient with a first-time traumatic anterior dislocation [1, 2]. It is still a matter of debate as to whether a first-time dislocation should be treated surgically. Since the descriptions by Rowe, the recurrence rate still remains high, particularly in young and active patients [17,18,19,20]. Due to the high risk of recurrence, there is a tendency to recommend primary surgical stabilization in this high-risk population [19].
In the present series, only 34 of 110 (30.9%) surgically treated patients had a “classic” Bankart lesion. In general, the authors recommend surgery after primary anterior shoulder dislocation in young patients under the age of 30 that are either involved in high-level contact or overhead sports or heavy work. Thus, patients with a soft tissue injury were younger than those with associated lesions (29 years, compared to 42 years in bony avulsion and 49 years in greater tuberosity fractures). This is in accordance with other studies [9, 13, 21]. In addition, 23 patients had SLAP lesions, of which the type 5 lesion was the most common [12, 22]. While other SLAP lesions, particularly type 2 lesions, are more frequently the result of compression forces applied to the glenohumeral joint, type 5 lesions are strongly associated with shoulder dislocations, since they represent a Bankart lesion that extends into the biceps anchor. Recently, Brockmeyer et al. suggested a treatment algorithm for SLAP lesions and stated that, in a type 5 lesion, a repair in combination with the anterior labrum reconstruction is widely recommended, at least in patients under 40 years of age [23]. Particularly for type 2 lesions, a strong correlation between the patients’ age and the functional results after SLAP repair is described. A study by Provencher et al. revealed that repairs of type 2 lesions are associated with worse results in patients older than 36 years [24].
Interestingly, a high number of patients (42) in the present cohort sustained a glenoid rim fracture. As mentioned above, increased age seems to be a risk factor for bony involvement. Throughout the current literature, patients with glenoid rim fractures are older than those with only soft tissue injuries [11, 13, 15, 25]. The mean defect size was 26% in the current study. However, when additional screw fixation was performed, the defect size increased to 36% and most of these fragments were solitary (type 1b according to Scheibel [4]). It is still unclear which glenoid rim fracture needs to be addressed surgically and which can be treated non-operatively. Some authors choose conservative treatment if the humeral head remains centered regardless of the size of the defect [26]. Even in large fragments, successful conservative treatment has been reported [27, 28]. However, Königshausen et al. demonstrated that a displacement and a fracture gap of 5 mm are associated with worse results [27]. Surgical fixation is usually associated with good results and may more sufficiently prevent posttraumatic osteoarthritis by full restoration of the anatomy [25, 29]. However, particularly in bony lesions, the integrity of the labral ring is crucial for the treatment strategy. Most of the techniques described for arthroscopic management of such lesions rely on the principles of “ligamentotaxis” [30]: fixation of the labral ring inferior and superior to the fragment leads to indirect reduction of the fragment, which can then be more easily reduced and fixed anatomically (Fig. 2). In the present study, the authors found the labral ring to be torn in 20 cases, equally distributed to soft tissue and bony injuries. While in soft tissue injuries, the labral ring can be closed prior to the classic Bankart repair (Fig. 3), fractures of the glenoid in combination with a torn labral ring are difficult to reconstruct both arthroscopically and in an open approach, since indirect reduction of the fragment cannot be achieved by traction on the labrum. In some cases, a fragment deep down in the axillary pouch may indicate a torn labral ring, which allows for its displacement (Fig. 5). The surgeon must be prepared for such cases and, in the case of non-reconstructable fractures, be able to perform a Latarjet or other bone-block procedure. Therefore, this situation remains an intraoperative challenge.
Smaller fragments or multifragmentary fractures can be successfully treated by incorporation into the capsulolabral fixation. However, with a conventional suture anchor Bankart repair technique, fragments tend to tilt or displace medially. This risk can be reduced with a “double-row repair” described by Millett as the bony Bankart bridge, in which the bony fragments are attached between a medial and a lateral row of anchors and compressed by a suture mattress [14]. The authors describe good functional results and a stable shoulder joint in 14 of 15 cases after a mean follow-up of 2.7 years. The average bone loss was 29%, which is comparable to those cases in the present study that underwent only soft tissue repair (26%).
Some inherent limitations apply to the present study. First, only surgically treated cases were analyzed. Since a group of conservatively treated patients is not provided, it is not possible to draw conclusions on the indication for either treatment, nor can the reported incidences and distributions be seen as general assumptions. Second, implications for surgical treatment of different types of lesion are described, but since no follow-up examinations were performed, no results with regard to functional outcome can be provided. However, based on the results of this analysis, follow-up studies are mandatory in order to further assess the impact of complete labral ring disruption and to assess what types of rim fractures benefit from surgical treatment.
Conclusion
In this series of surgically treated first-time traumatic anterior shoulder dislocations, the majority of cases presented with more complex lesions than an isolated classic Bankart lesion. The risk for bony involvement and associated pathologies such as cuff tears and greater tuberosity fracture increases with age and requires a more extensive surgical approach. Disruption of the labral ring was frequently found in both soft tissue and bony lesions and directly affects the surgical procedure.
References
Bankart AS, Cantab MC (1993) Recurrent or habitual dislocation of the shoulder-joint. 1923. Clin Orthop Relat Res 291:3–6
Hintermann B, Gachter A (1995) Arthroscopic findings after shoulder dislocation. Am J Sports Med 23(5):545–551
Porcellini G et al (2007) Long-term outcome of acute versus chronic bony Bankart lesions managed arthroscopically. Am J Sports Med 35(12):2067–2072
Scheibel M et al (2009) Anterior glenoid rim defects of the shoulder. Orthopade 38(1):41–8, 50–3
Durban CM et al (2016) Anterior shoulder instability with concomitant superior Labrum from anterior to posterior (SLAP) lesion compared to anterior instability without SLAP lesion. Clin Orthop Surg 8(2):168–174
Neviaser TJ (1993) The GLAD lesion: another cause of anterior shoulder pain. Arthroscopy 9(1):22–23
Dai F et al (2020) Injury mechanism of acute anterior shoulder dislocation associated with Glenoid and greater tuberosity fractures: a study based on fracture morphology. Orthop Surg 12(5):1421–1429
Dimakopoulos P et al (2007) Anterior traumatic shoulder dislocation associated with displaced greater tuberosity fracture: the necessity of operative treatment. J Orthop Trauma 21(2):104–112
Dussing F et al (2018) Anterior shoulder dislocation and concomitant fracture of the greater tuberosity: clinical and radiological results. Obere Extrem 13(3):211–217
Sugaya H (2014) Techniques to evaluate glenoid bone loss. Curr Rev Musculoskelet Med 7(1):1–5
Sugaya H et al (2003) Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am 85(5):878–884
Maffet MW, Gartsman GM, Moseley B (1995) Superior labrum-biceps tendon complex lesions of the shoulder. Am J Sports Med 23(1):93–98
Godin JA et al (2019) Midterm results of the bony Bankart bridge technique for the treatment of bony Bankart lesions. Am J Sports Med 47(1):158–164
Millett PJ, Braun The S (2009) “bony Bankart bridge” procedure: a new arthroscopic technique for reduction and internal fixation of a bony Bankart lesion. Arthroscopy 25(1):102–105
Millett PJ, Horan MP, Martetschlager F (2013) The “bony Bankart bridge” technique for restoration of anterior shoulder stability. Am J Sports Med 41(3):608–614
Hill HA, Sachs MD (1940) The grooved defect of the humeral head. Radiology 35(6):690–700
Hovelius L et al (1996) Primary anterior dislocation of the shoulder in young patients. A ten-year prospective study. J Bone Joint Surg Am 78(11):1677–1684
Hovelius L et al (2008) Nonoperative treatment of primary anterior shoulder dislocation in patients forty years of age and younger. a prospective twenty-five-year follow-up. J Bone Joint Surg Am 90(5):945–952
Hurley ET et al (2020) Arthroscopic Bankart repair versus conservative management for first-time traumatic anterior shoulder instability: a systematic review and meta-analysis. Arthroscopy 36(9):2526–2532
Rowe CR (1963) Anterior dislocations of the shoulder: prognosis and treatment. Surg Clin North Am 43:1609–1614
Muhm M et al (2017) Associated injuries with greater tuberosity fractures : mechanism of injury, diagnostics, treatment. Unfallchirurg 120(10):854–864
Snyder SJ et al (1990) SLAP lesions of the shoulder. Arthroscopy 6(4):274–279
Brockmeyer M et al (2016) SLAP lesions: a treatment algorithm. Knee Surg Sports Traumatol Arthrosc 24(2):447–455
Provencher MT et al (2013) A prospective analysis of 179 type 2 superior labrum anterior and posterior repairs: outcomes and factors associated with success and failure. Am J Sports Med 41(4):880–886
Scheibel M et al (2016) Arthroscopic reduction and fixation of large solitary and multifragmented anterior glenoid rim fractures. J Shoulder Elbow Surg 25(5):781–790
Ernstbrunner L, Jessen M, Wieser K (2020) Anatomic healing after non-operative treatment of a large, displaced anterior glenoid rim fracture after primary traumatic anterior shoulder dislocation—a case report. BMC Musculoskelet Disord 21(1):361
Konigshausen M et al (2016) Results of non-operative treatment of fractures of the glenoid fossa. Bone Joint J 98-B(8):1074–1079
Kraus N et al (2010) Conservative therapy of antero-inferior glenoid fractures. Unfallchirurg 113(6):469–475
Tauber M et al (2008) Arthroscopic screw fixation of large anterior glenoid fractures. Knee Surg Sports Traumatol Arthrosc 16(3):326–332
Corradini A et al (2018) Arthroscopic repair of glenoid rim fractures: a ligamentotaxis surgical technique. Musculoskelet Surg 102(Suppl 1):41–48
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
B. Schliemann, F. Dyrna, V. Kravchenko, M. J. Raschke, and J. C. Katthagen declare that they have no competing interests.
Ethical approval was not required due to retrospective study design without patient examinations. However, this chart review study was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schliemann, B., Dyrna, F., Kravchenko, V. et al. Labral lesions in first-time traumatic anterior shoulder dislocation: it’s more than just Bankart …. Obere Extremität 16, 34–40 (2021). https://doi.org/10.1007/s11678-021-00629-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11678-021-00629-w