Abstract
Background
Stigma is a barrier to the uptake of buprenorphine to treat opioid use disorder. Harm reduction treatment models intend to minimize this stigma by organizing care around non-judgmental interactions with people who use drugs. There are few examples of implementing buprenorphine treatment using a harm reduction approach in a primary care setting in the USA.
Methods
We conducted a qualitative study by interviewing leadership, staff, and external stakeholders at Respectful, Equitable Access to Compassionate Healthcare (REACH) Medical in Ithaca, NY. REACH is a freestanding medical practice that provides buprenorphine treatment for opioid use disorder since 2018. We conducted semi-structured interviews with 17 participants with the objective of describing REACH’s model of care. We selected participants based on their position at REACH or in the community. Interviews were recorded, transcribed, and analyzed for themes using content analysis, guided by the CDC Evaluation Framework.
Results
REACH provided buprenorphine, primary care, and mental health services in a low-threshold model. We identified three themes related to delivery of buprenorphine treatment. First, an organizational mission to provide equitable and low-stigma healthcare, which was a key to organizational identity. Second, a low-threshold buprenorphine treatment approach that was critical, but caused concern about over-prescribing and presented logistical challenges. Third, creation and retention of a harm reduction-oriented workforce by offering value-based work and by removing administrative barriers providers may face elsewhere to providing buprenorphine treatment.
Conclusions
A harm reduction primary care model can help reduce stigma for people who use drugs and engage in buprenorphine treatment. Further research is needed to evaluate whether this model leads to improved patient outcomes, can overcome community stakeholder concerns, and is sustainable.
Similar content being viewed by others
INTRODUCTION
Buprenorphine is highly effective at reducing opioid-related mortality and can be provided in office settings.1,2 As of 2017, however, nearly half of US counties lacked even one prescriber.3,4 Stigma is a major reason for the suboptimal uptake of buprenorphine, which can be associated with drug use itself and with medication treatment. 5,6 Stigma also discourages people who use drugs (PWUD) from engaging with healthcare and from disclosing their drug use to providers.6 Although buprenorphine is an FDA-approved treatment for opioid addiction, some patients and providers still perceive medication treatment as “trading one addiction for another.”7,8,9 Other provider-level barriers include perception of low reimbursement, obtaining a waiver to prescribe, and fears about buprenorphine diversion.10,11
Low-stigma services for people who use drugs (PWUD) have long been the purview of syringe service programs that espouse a harm reduction approach. “Harm reduction” refers to both a practice and a philosophy. The practice of harm reduction includes (but is not limited to) providing sterile injection equipment, naloxone, education about safe injection and overdose prevention, and testing for bloodborne infection such as HIV and hepatitis C. Here, we primarily refer to harm reduction as the philosophy that underlies these strategies, in which a program’s goal is to reduce the negative consequences of drug use without requiring abstinence.12,13 The harm reduction philosophy, when applied to the healthcare setting, uses multiple approaches that mitigate the stigma that PWUD face in the healthcare system, such as refraining from moral judgment and celebrating incremental positive change.14
“Respectful, Equitable Access to Compassionate Healthcare” (REACH) is an independent, not-for-profit, community-based medical practice serving a predominantly non-urban population in Ithaca, NY. REACH provides office-based buprenorphine treatment and primary care in a harm reduction–informed manner.
This qualitative study was conducted as the first step in a program evaluation of the REACH model of care using the CDC Evaluation Framework.15 The objective of this study is to describe the innovative aspects of this model of care, using data collected from internal and external stakeholders. While there is a growing interest in harm reduction among healthcare organizations, there have been few detailed descriptions of how medical practices operationalize this integration. Existing US models of low-threshold buprenorphine treatment typically take place in academic settings16,17,18, as part of a larger healthcare organization,19,20 or at syringe service programs.21 In contrast, REACH operates as a freestanding medical practice, a model rarely reported in the literature. This qualitative study provides a rich description of this model of practice, incorporating the perspectives of multiple internal and external stakeholders.
METHODS
Research Team
Methods and results are reported according to the COREQ checklist.22 The research team consisted of four university researchers (SNK, BRS, NZ, CNB) and two REACH leaders—the executive director (JW) and the director of research (JG). Three are physicians (SNK, JG, JW) who care for PWUD, and three are researchers (BRS, NZ, CNB) who study healthcare delivery for PWUD. The researchers’ prior beliefs included supporting medication treatment and harm reduction services as being evidence-based.
Design
We conducted semi-structured interviews of 3 participant groups: (1) REACH leadership, (2) REACH staff, and (3) external stakeholders. We identified all existing personnel at REACH (n = 26) and categorized them as leadership (n = 8) or staff (n = 18). For external stakeholders, we identified organizations that would have a perspective on REACH. We identified key informants (n = 22) in those organizations in consultation with the REACH medical director and director of research. We used purposive sampling, selecting potential participants based on job title and expertise to maximize the diversity of participants, including both clinical and non-clinical personnel. University researchers constructed the final list of individuals to contact and maintained confidentiality of that list from REACH collaborators. We approached participants by email and used an oral informed consent script that was approved by the Weill Cornell Medicine Institutional Review Board. Sampling continued until thematic saturation, meaning no new themes emerged when analyzing additional interviews.23
We developed three interview guides, one for each participant group (Supplementary Table 1). We asked all participants about the mission of the organization and the services provided. Additionally, we asked leadership about the organization’s history and factors related to funding and organizational structure. We asked providers and staff about their personal experiences with substance use care. We asked external stakeholders about the local resources for substance use disorder treatment, and to compare REACH to these resources. We approached 21 individuals for interviews; 17 consented and were enrolled. Depending on participants’ preferences and interviewer availability, interviews were conducted either by phone or in person, and lasted 30–90 min (mean 67 min, SD: 22 min). On-site interviews were conducted in a private room with a closed door, either in Ithaca, NY, or at a satellite site in Johnson City, NY. Participants were not compensated for the interviews. Two researchers (SNK, CNB) conducted the interviews, which were audio-recorded and transcribed. REACH team members (JG, JW) did not have access to the interviewee list, transcripts, or recordings.
Analysis
We used content analysis, with analyses conducted iteratively while data collection was ongoing.24 We derived the initial coding structure from the CDC Evaluation framework, categorizing program features into (1) Need, (2) Expected effects, (3) Activities, (4) Resources, (5) Stage of Development, and (6) Context.15 Two researchers (SNK, CNB) coded the first 6 transcripts using the NVivo software to refine the final coding structure; then, one researcher (SNK) coded the remainder of transcripts, and a second investigator reviewed the coded data for omissions and divergent opinions.25 We identified the themes that emerged across these categories by categorizing relating codes into themes, and refined them in discussions with the full research team. In this manuscript, we report findings organized by theme, with the focus on describing the program activities. We reviewed emergent themes with REACH leadership and staff and incorporated their feedback.
RESULTS
Table 1 describes the 17 participants in this study. Of these, 6 were REACH staff (labeled “S” in quote attributions), 4 were leadership (labeled “L”), and 7 were external stakeholders (labeled “E”). Of the 10 REACH leadership and staff, 7 were clinical providers and 5 of these were buprenorphine prescribers. We first describe the clinical activities as reported in the interview data. We then report 3 major themes: (1) an organizational mission to provide equitable and low-stigma healthcare, (2) low-threshold buprenorphine treatment, and (3) the creation and retention of a harm reduction workforce. These themes, with representative quotes, are summarized in Table 2.
Description of REACH Clinical Activities
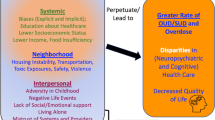
Figure 1 shows clinical and social services that REACH offered at the time of our interviews. The practice relied on a nurse-led model: patients were first evaluated by registered nurses (RNs) who performed history and vital signs, and then conducted a “bio-psychosocial assessment” (S1) which elicited information about treatment goals, current substance use behaviors, and socioeconomic factors. Patients were asked to provide urine for drug screening. Both home and office induction were available. Most prescribers were contracted on an hourly basis, whereas most nurses were employees.
Part-time family medicine and internal medicine providers at REACH offered primary care, including for a small number of patients not on buprenorphine. The initial visit for primary care patients involved a less extensive intake and no urine drug screen. One participant estimated that “40% of our unique patients get primary care here” (L3). At the time of our study, REACH was in the process of developing quality assessment protocols for primary care.
REACH employed one psychiatric nurse practitioner for medication management of people with mental health conditions. Because of high demand, the individual practitioner was “having to see people for quite short visits” (S4). This limited the ability to provide therapeutic counseling as it related to substance use disorder, or to manage more severe mental health conditions. Since the time of the interviews, REACH added additional mental health providers to address this need.
Theme 1: Organizational Mission to Provide Equitable and Low-Stigma Healthcare
Participants were aware of the harm reduction–oriented mission of REACH, and felt that the mission was unique when compared to other substance use treatment providers in the region.
Theme 1.1: Mission of Reducing Stigma as the Key to Organizational Identity
REACH employees and external stakeholders both identified an organizational mission of reducing stigma and advancing health equity: “We knew from day one that …we would provide stigma free, compassionate care at all times. That’s really the foundation of our organization and has always been part of our mission” (L2). Participants emphasized established principles of harm reduction, such as “meeting people where they’re at” to offer individualized support based on a patient’s readiness to change and their current medical and social situation. Staff were motivated to meet patients’ complex social needs without judgment: “REACH is a place that just has the reputation where you will get help. You will get accepted. It’s really remarkable [how] the philosophy—there was always a philosophy—translates through the staff” (E5).
Theme 1.2: Contrast Between REACH and Other Healthcare Providers
Stigma was linked to the inability to access medical care in the area: “We struggle with local primary care providers [not] wanting those with substance use disorders to be there. It’s the stigma of ‘I don’t want these people in my lobby with my other clients’” (E1). Participants were also aware of the contrast between REACH’s approach and the “traditional” substance use disorder treatment model:
They’re mainstream [state-licensed] substance use treatment providers, but I think that those models or those organizations are stuck in a place of using older technology. …There’s really a focus on kind of a 12-step foundation that has a lot to do with group therapy experiences, individual talk therapy experiences, but is very short on some of the things that we can prove work, like medication assisted treatment. (E2)
This was partly attributed to the “traditional abstinence only perspective” (E2) that had been a norm in substance use treatment. Several participants noted that state-licensed substance use treatment providers practice in “a very rigid system” (E2) due to regulation from the state licensing agency. REACH, in contrast “[intentionally] opened as a freestanding medical practice” to be more “nimble” and have the “liberty to [provide care] as the organization chooses, and not be subject to state approval” (L2). Since the time of the interviews, REACH did obtain state-licensing, due to new state policies that allowed them to continue their model of practice.
Theme 2: Low-Threshold Buprenorphine Treatments and Other Clinical and Social Services
The “low-threshold” model of REACH aimed to reduce barriers to initiating patients on buprenorphine and retaining them in treatment. There were differing perspectives among stakeholders and challenges in integrating this treatment into primary care. The hallmarks of this low-threshold model, according to participants, were “being willing to give anybody a shot” (E4), and to “never discharge [patients] if they miss too many appointments” (L2).
Theme 2.1: Differences with Community Buprenorphine Dosing and Treatment Norms
External stakeholders observed tension in the community around prescribing practices at REACH:
[REACH] has received a lot of…public shaming about the doses of Suboxone that [they are] using because…a certain amount of people are on 16 [mg], or 24 [mg]…and the local treatment providers tend to be fairly reluctant to put people on 16 and rarely would ever consider a dose larger than that (E3).
One participant had been contacted by several pharmacists who “refuse to fill a REACH prescription, saying it was outside of the FDA guidelines for the prescription” (E4). The difference between the maintenance dose of buprenorphine that is recommended in medical training and the dose that patients might need to avoid withdrawal was also noted by one staff member: “You kind of do your training and they’re talking about people on 4 mg and 8 mg and…many of our patients are on 24 mg, which.. I feel comfortable going up to that, but then patients are often like ‘I need a higher dose’” (S4). One participant felt there was a philosophical barrier in the community: “there is a long history in the methadone world of, you know, get people on it, give them as little as possible, and then get them back off as quickly as possible. And that philosophy…carries on into the present and…on the face of it, it’s ridiculous” (E2).
There was disagreement around diversion of medication. Some participants, including one external stakeholder, shared a belief that diverted buprenorphine “means that somebody else doesn’t buy heroin” (L1). However, several participants commented that law enforcement agencies did not view it the same way: “Law enforcement is finding them at drug raids. They’re really upset about this. They’re feeling like it’s adding to the drugs on the street” (E4).
Theme 2.2: Logistical Challenges in Providing Low-Threshold Buprenorphine
One REACH employee commented on the need to balance a “very high no-show rate” and a “lot of walk-ins,” which made the clinical flow variable (L2). Staff performed “morning huddles” to anticipate the potential workflow in each day. Physician providers were largely part time, so walk-in visits and phone calls were often addressed by covering physicians, although nursing staff were usually present to ensure continuity of care. Sometimes this approach presented logistical challenges:
One of the… things that make it a little bit tricky…is that there are so many providers that are working short shifts, and so when these people call needing something we have to reach out to these providers…and then wait for them to get back (S2).
An added complexity was managing each provider’s buprenorphine “slots.” For newly trained providers, the maximum patient load was 30, so “in order to meet the demand, [REACH] had to bring on multiple doctors that are all just doing 30 in their first year” (E1). The practice manager took on the logistics of managing prescriber slots to ensure that all prescribers were within the limits allotted to them, which sometimes involved scheduling patients with other providers who had slots available. This was an important problem but a temporary one, as most providers were able to increase their capacity from 30 to 100 in their second year, and to increase even further after the second year up to 275. Most REACH staff agreed that lack of personnel and physical space presented larger challenges to meeting demand than physician prescribing capacity did.
Theme 2.3: Integration of Primary Care with Buprenorphine Treatment
Integration of primary care and created additional challenges to overcome. For many patients with substance use disorder, other health issues “get shuffled to the back” (S3). One provider expressed a tension between the need to quickly get patients on buprenorphine with the time commitment needed to practice longitudinal primary care:
People will call, they need to get in because they’re desperate to get on [medication assisted therapy (MAT)]…but then they also want primary care….and all of a sudden I’m now their primary care physician and they’re like, diabetic, on insulin, and we never did the groundwork that we needed to do (S4).
Some providers stated they would require additional training in skills such as abscess drainage, whereas others would need training in chronic disease management or in specific areas such as hepatitis C treatment.
Theme 3: Creation and Retention of a Harm Reduction Healthcare Workforce
Participants described the steps needed to train healthcare workers in the harm reduction culture and to maintain that culture over time.
Theme 3.1: Providers’ Previous Experiences in the Healthcare System
REACH needed to attract providers and staff who were willing to practice in a harm reduction model, train them in that model, and sustain their culture as the medical practice expanded. REACH leadership set the goal of being “low threshold for providers,” stating that “it’s under-recognized by patients…that [we] providers are being treated in a corporate medical model and...we’re not delivering the care we want to give” (L4). Providers and staff reinforced this notion: “I’m at the hospital [in my previous job], and I’m there for 12 hours just churning out visits for the sake of volume, and that’s not what I want to do” (S3). Staff also mentioned the appeal of “[working] with more underserved populations” and “doing hands-on, meaningful work in a respectful and compassionate way” (S3).
Participants acknowledged the difficulties of prescribing buprenorphine in many other office settings:
We’ve had local providers who have been waiver providers for several years and never used their licenses because they didn’t feel like they could do it in their primary care office...[REACH] is offering them an opportunity to do the right thing and making it easy (E3).
One provider recalled “so many structural barriers to providing [buprenorphine] that I didn’t even try to do it at my other jobs,” including lacking other clinical providers who could cover for related issues (L3). Another was also grateful for billing support: “if I were billing for myself, I would be overwhelmed” (S5).
Theme 3.2: “Harm-Reductionizing” New Providers
Multiple participants referred to providers as being “harm-reductionized,” meaning they were provided training and acculturation to the harm reduction environment (S1, L2, L3). REACH covered the cost for providers who needed buprenorphine waiver training. New providers shadowed the director and met with the practice manager to learn the culture of the practice. New hires also received online educational sessions related to harm reduction such as training in motivational interviewing and using stigma-free language. There was an explicit attempt to orient new hires to some of the logistical challenges of the work: “Your patients aren’t gonna show up on time. You’re not gonna get out on time. If [patients] do show up, we’re not gonna turn them away...” (S1). Staff meetings provided an opportunity for ongoing reinforcement of these principles. The importance of acculturation was considered critical for maintaining patient trust: “If any part of that chain falls apart, then we re-traumatize someone and they stop coming for help” (L3).
Theme 3.3: Maintaining a Harm Reduction Culture
There were several challenges to maintaining this culture, especially as the practice grew to include more providers and staff. Some providers were initially less attuned to harm reduction principles, being “deeply rooted in the old model” (L2) and having “one of [the] biggest learning curves [be] tipping my focus and my frame of mind in approaching the population” (S3). Working with the high-need population also came with a risk of emotional burnout:
After about the first three or four months I was definitely feeling emotionally burned out…getting everybody’s hour long story of why they started doing heroin at 13-years-old. So, it was incredibly just draining in that sense that I could just feel all of them and what they've been through... I just felt so bad because I feel helpless with this population at times (S2).
The harm reduction culture also encouraged staff to be more vulnerable and open than in traditional medical environments, which could lead to difficulty in setting professional norms:
[They] know that it’s a safe space and they wind up sharing more with you, and sharing more with the patients, and relating with everybody on this rock-bottom raw, honest level. And so it’s almost more difficult to manage because you’re like, ‘well, I don’t know if it’s appropriate in the workplace, but wait, where do I draw the line?’ (S1).
DISCUSSION
We describe a low-threshold model of buprenorphine treatment in a freestanding primary care practice in upstate New York. We detail the model of care delivery, illustrate the way that a harm reduction philosophy can change provider and clinic culture, and describe the approach to creating and sustaining a harm reduction workforce.
The integration of the harm reduction philosophy and medication treatment for opioid use disorder can be complicated by a “philosophical clash” between two models of care.26 In the traditional healthcare model, the provider and institution are empowered as the holders of knowledge. In contrast, the harm reduction philosophy empowers the patient, with healthcare delivery being determined by the patient’s self-determined needs. Our findings suggest that this traditional philosophy has also been integrated into licensing requirements for substance use treatment programs, which can limit their flexibility to adopt harm reduction approaches. Additionally, we see the application of this philosophical difference when examining REACH’s treatment initiation and retention criteria, and buprenorphine dosing practices.
One application of the harm reduction philosophy employed by REACH is to have flexible criteria for initiation and retention in buprenorphine treatment. In contrast, other practices may implement administrative barriers, such as waiting lists and out-of-pocket costs; or clinical ones, such as treatment initiation criteria and zero tolerance for ongoing drug use.27 These barriers further propagate the stigma associated with engaging in treatment. In one study, 30% of involuntary discharges from buprenorphine treatment within 6 months were due to either attendance policies or urine drug screens.28 Reports from individual practices have described feasibility and patient satisfaction using low-threshold strategies to reduce the barriers to initiating buprenorphine.17,18,19,20,29 A direct comparison with REACH is challenging, however, due to differences in the specific treatment designs and the clinical settings. A unique feature of REACH is that the low-barrier approach has been a foundational philosophy since its inception, rather than a change from a high-barrier one. Additionally, REACH is not part of a larger healthcare system such as a university, in which involvement with the parent organization may still produce stigma.
REACH’s typical buprenorphine doses of 16 or 24 mg/day revealed some tensions, as discussed in theme 2.1. National guidelines are generally consistent with FDA-approved labeling of 24 mg/day as a maximum maintenance dose, but acknowledge potential benefit of higher doses.30,31 Clinical studies have shown poorer treatment outcomes with lower doses compared to higher doses.32,33 Two clinical trials that allowed for escalation beyond the FDA-approved 24-mg daily dose showed no adverse safety signals and modest improvement in retention with higher doses.34,35 Nevertheless, some providers limit their own dosing below that threshold, such as 4 or 8 mg/day, and view higher doses as being outside community norms. Concern from the community and from law enforcement that patients may divert excess buprenorphine also influences perception of acceptable buprenorphine doses. This underscores the difference between the harm reduction philosophy, which prioritizes patients’ self-determination, and a more traditional healthcare philosophy in which the system prioritizes considerations outside of the individual patient’s expressed needs.
The need for increased clinical capacity to provide buprenorphine is well-documented, especially in rural settings.36 Research about barriers faced by providers to providing buprenorphine point to institutional support as a key factor.10,11 Moreover, research on physician satisfaction and burnout has documented that provider job satisfaction is affected by providers’ perceived ability to provide compassionate healthcare, and by minimizing the “professional dissonance” between clinical goals (e.g., improving patient health) and institutional ones (e.g., maximizing revenue).37,38 Nevertheless, our findings in theme 3.3 also reflect that “compassion fatigue” and emotional burnout can be common among service providers who work with people affected by trauma, as is common for PWUD.39,40 In addition to providing the opportunity to do meaningful work treating substance use disorders, organizations may need to develop strategies for providers to address the emotional consequences of that work.
There are several limitations of this study. In keeping with the goal of qualitative research, we aimed to provide a deep understanding of this unique treatment model. Further research should confirm whether similar issues arise in other clinical settings. We conducted interviews less than 1 year after REACH’s opening the medical practice. The factors here represent the issues that might be faced by a similar organization at a similar stage of development, with further work needed to understand how these factors would evolve over time. This study does not report on the direct perspective of patients served at REACH, other substance use treatment providers, or regulatory agencies.
In conclusion, this qualitative study describes a unique model of buprenorphine treatment delivery in a community-based primary care setting. This innovative treatment model addresses healthcare system stigma for people who use drugs. As the US healthcare system attempts to meet the rising demand for opioid use disorder treatment, accessible models that overcome traditional barriers to treatment access are needed. Further research is needed to evaluate whether the model leads to improved patient outcomes, overcomes community stakeholder concerns, and is financially sustainable.
References
Gibson A, Degenhardt L, Mattick RP, Ali R, White J, O'Brien S. Exposure to opioid maintenance treatment reduces long-term mortality. Addiction. 2008;103(3):462–468.
Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev 2014(2):CD002207.
Andrilla CHA, Moore TE, Patterson DG, Larson EH. Geographic Distribution of Providers With a DEA Waiver to Prescribe Buprenorphine for the Treatment of Opioid Use Disorder: A 5-Year Update. J Rural Health 2019;35(1):108–112.
Haffajee RL, Lin LA, Bohnert ASB, Goldstick JE. Characteristics of US Counties With High Opioid Overdose Mortality and Low Capacity to Deliver Medications for Opioid Use Disorder. JAMA Netw Open 2019;2(6):e196373.
van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend 2013;131(1–2):23–35.
Biancarelli DL, Biello KB, Childs E, et al. Strategies used by people who inject drugs to avoid stigma in healthcare settings. Drug Alcohol Depend 2019;198:80–86.
Madden EF. Intervention stigma: How medication-assisted treatment marginalizes patients and providers. Soc Sci Med 2019;232:324–331.
Muthulingam D, Bia J, Madden LM, Farnum SO, Barry DT, Altice FL. Using nominal group technique to identify barriers, facilitators, and preferences among patients seeking treatment for opioid use disorder: A needs assessment for decision making support. J Subst Abus Treat 2019;100:18–28.
Richard EL, Schalkoff CA, Piscalko HM, et al. “You are not clean until you’re not on anything”: Perceptions of medication-assisted treatment in rural Appalachia. Int J Drug Policy 2020:102704.
Andrilla CHA, Coulthard C, Larson EH. Barriers Rural Physicians Face Prescribing Buprenorphine for Opioid Use Disorder. Ann Fam Med 2017;15(4):359–362.
Kermack A, Flannery M, Tofighi B, McNeely J, Lee JD. Buprenorphine prescribing practice trends and attitudes among New York providers. J Subst Abus Treat 2017;74:1–6.
Harm Reduction Coalition. Principles of Harm Reduction. https://harmreduction.org/about-us/principles-of-harm-reduction/. Accessed Aug 15 2020.
Harm Reduction International. What is harm reduction? 2020; https://www.hri.global/what-is-harm-reduction. Accessed Aug 15 2020.
Hawk M, Coulter RWS, Egan JE, et al. Harm reduction principles for healthcare settings. Harm Reduct J 2017;14(1):70.
Framework for program evaluation in public health. MMWR Recomm Rep 1999;48(RR–11):1–40.
Wakeman SE, Rigotti NA, Chang Y, et al. Effect of Integrating Substance Use Disorder Treatment into Primary Care on Inpatient and Emergency Department Utilization. J Gen Intern Med 2019;34(6):871–877.
Payne BE, Klein JW, Simon CB, et al. Effect of lowering initiation thresholds in a primary care-based buprenorphine treatment program. Drug Alcohol Depend 2019;200:71–77.
Snow RL, Simon RE, Jack HE, Oller D, Kehoe L, Wakeman SE. Patient experiences with a transitional, low-threshold clinic for the treatment of substance use disorder: A qualitative study of a bridge clinic. J Subst Abus Treat 2019;107:1–7.
Lee CS, Rosales R, Stein MD, et al. Brief Report: Low-Barrier Buprenorphine Initiation Predicts Treatment Retention Among Latinx and Non-Latinx Primary Care Patients. Am J Addict 2019;28(5):409–412.
Bhatraju EP, Grossman E, Tofighi B, et al. Public sector low threshold office-based buprenorphine treatment: outcomes at year 7. Addict Sci Clin Pract 2017;12(1):7.
Bachhuber MA, Thompson C, Prybylowski A, Benitez JM, Mazzella SM, Barclay D. Description and outcomes of a buprenorphine maintenance treatment program integrated within Prevention Point Philadelphia, an urban syringe exchange program. Subst Abus 2018;39(2):167–172.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19(6):349–357.
Bourgeault IL, Dingwall R, De Vries RG. The SAGE handbook of qualitative methods in health research. Los Angeles: SAGE; 2010.
Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15(9):1277–1288.
NVivo Qualitative Data Analysis Software [computer program]. Version 11: QSR International Pty Ltd.; 2017.
Heller D, McCoy K, Cunningham C. An invisible barrier to integrating HIV primary care with harm reduction services: philosophical clashes between the harm reduction and medical models. Public Health Rep 2004;119(1):32–39.
Kourounis G, Richards BD, Kyprianou E, Symeonidou E, Malliori MM, Samartzis L. Opioid substitution therapy: Lowering the treatment thresholds. Drug Alcohol Depend 2016;161:1–8.
Gryczynski J, Mitchell SG, Jaffe JH, O'Grady KE, Olsen YK, Schwartz RP. Leaving buprenorphine treatment: patients' reasons for cessation of care. J Subst Abus Treat 2014;46(3):356–361.
Jakubowski A, Fox A. Defining Low-threshold Buprenorphine Treatment. J Addict Med 2020;14(2):95–98.
American Society of Addiction Medicine. National Practice Guideline for the Use of Medications in the Treatment of Addiction Involving Opioid Use. Chevy Chase, MD: American Society of Addiction Medicine, 2015.
Substance Abuse and Mental Health Services Administration. Medications for Opioid Use Disorder. Treatment Improvement Protocol (TIP) Series 63, Full document. Rockville, 2018.
Accurso AJ, Rastegar DA. The Effect of a Payer-Mandated Decrease in Buprenorphine Dose on Aberrant Drug Tests and Treatment Retention Among Patients with Opioid Dependence. J Subst Abus Treat 2016;61:74–79.
Kapuganti A, Turner T, Thomas CJ. Evaluation of buprenorphine/naloxone dose and use of sedating supportive medication on treatment outcomes in veterans with opioid use disorder. Mental Health Clin 2017;7(6):271–275.
Hser YI, Saxon AJ, Huang D, et al. Treatment retention among patients randomized to buprenorphine/naloxone compared to methadone in a multi-site trial. Addiction. 2014;109(1):79–87.
Jacobs P, Ang A, Hillhouse MP, et al. Treatment outcomes in opioid dependent patients with different buprenorphine/naloxone induction dosing patterns and trajectories. Am J Addict 2015;24(7):667–675.
Cole ES, DiDomenico E, Cochran G, et al. The Role of Primary Care in Improving Access to Medication-Assisted Treatment for Rural Medicaid Enrollees with Opioid Use Disorder. J Gen Intern Med 2019;34(6):936–943.
Lown BA, Shin A, Jones RN. Can Organizational Leaders Sustain Compassionate, Patient-Centered Care and Mitigate Burnout? J Healthc Manag 2019;64(6):398–412.
Agarwal SD, Pabo E, Rozenblum R, Sherritt KM. Professional Dissonance and Burnout in Primary Care: A Qualitative Study. JAMA Intern Med 2020.
Cosden M, Sanford A, Koch LM, Lepore CE. Vicarious trauma and vicarious posttraumatic growth among substance abuse treatment providers. Subst Abus 2016;37(4):619–624.
Reyre A, Jeannin R, Largueche M, Moro MR, Baubet T, Taieb O. Overcoming professionals’ challenging experiences to promote a trustful therapeutic alliance in addiction treatment: A qualitative study. Drug Alcohol Depend 2017;174:30–38.
Acknowledgments
The authors acknowledge the study participants for sharing their time and experience.
Funding
This work was funded by the Cornell Center for Health Equity, the National Institute on Drug Abuse (P30 DA040500 and K01 DA048172), and the National Institute of Mental Health (T32 MH073553).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Kapadia has received research grants paid to his institution from Gilead Sciences Inc., unrelated to the current study, for research related to hepatitis C. All other authors declare no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 13 kb)
Rights and permissions
About this article
Cite this article
Kapadia, S.N., Griffin, J.L., Waldman, J. et al. A Harm Reduction Approach to Treating Opioid Use Disorder in an Independent Primary Care Practice: a Qualitative Study. J GEN INTERN MED 36, 1898–1905 (2021). https://doi.org/10.1007/s11606-020-06409-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-020-06409-6