Abstract
Background
The association between pharmaceutical industry promotion and physician opioid prescribing is poorly understood. Whether the influence of industry gifts on prescribing varies by specialty is unknown.
Objective
To examine the relationship between opioid-related gifts to physicians and opioid prescribing in the subsequent year across 7 physician specialties.
Design
Panel study using data from 2014 to 2016.
Participants
236,103 unique Medicare Part D physicians (389,622 physician-years) who received any gifts from pharmaceutical companies measured using Open Payments and prescribed opioids in the subsequent year.
Main Measures
Amounts paid by pharmaceutical companies for opioid-related gifts including meals and lodging; quartile of opioid prescribing as a percent of total prescribing compared with other same-specialty physicians.
Key Results
In 2014–2015, 14.1% of physician received opioid-related gifts from the industry with 2.6% receiving > $100. Gifts varied by specialty and were concentrated among two pharmaceutical companies responsible for 60% of the value of opioid-related gifts. Receiving opioid-related gifts was associated with greater prescribing of opioids compared with same-specialty physicians in the next year. Primary care physicians are nearly 3.5 times as likely to be in the highest quartile of prescribing versus the lower quartiles if they were paid ≥ $100. Psychiatrists and neurologists were 7 to 13 times as likely to be in a higher quartile of opioid prescribing compared with colleagues who were paid $0 in the preceding year.
Conclusions
The value of opioid-related gifts given to physicians varies substantially by provider specialty, as does the relationship between payment amounts and prescriber behavior in the following year.
Similar content being viewed by others
INTRODUCTION
In 2017, there were 58 opioid prescriptions written for every 100 Americans, and 46 people died every day from prescription opioid overdoses.1 Policy efforts to combat the prescription opioid epidemic at both the federal and state levels have included limits on opioid prescribing and redirecting treatment for pain-related conditions to nonopioid interventions.2 Despite these efforts and a decline in overall opioid prescribing since 2012, the morphine milligram equivalents of opioids prescribed per person in the USA are three times what they were in 1999.1
Pharmaceutical industry gifts, such as meals, travel, and educational materials, may be one factor contributing to continued high rates of opioid prescribing in the USA.3, 4 Between 2013 and 2015, the pharmaceutical industry paid providers $46.2 million related to opioid products in the form of gifts.5 While observational and experimental research indicates that providers may perceive themselves to be immune to bias from gift giving,6,7,8,9 even small gifts have been shown to create unconscious bias towards drug prescribing.6,7,8 Recent lawsuits and criminal charges related to promotion of opioid products have increased public scrutiny around these gifts.10,11,12,13
There are multiple gaps in our knowledge about how gifts from pharmaceutical companies may influence prescribing behavior. First, most prior research has examined the marginal influence of each dollar on opioid prescribing, although behavioral economics suggests that there may be a nonlinear relationship between financial incentives and prescribing.14 Second, the volume of opioid prescribing varies by specialty, from as little as 3.6% of a physician’s total prescribing in non-surgical, non-primary care specialties to nearly 50% among pain medicine specialists.15 A provider’s response to pharmaceutical industry gifts might vary by baseline levels of opioid prescribing volume. The objective of this study is to examine the relationship between opioid prescribing by provider specialty and the value of gifts given to physicians by pharmaceutical companies related to promotion of opioid products in the subsequent year. We contribute to the existing literature by (1) measuring differences in the dollar value of opioid manufacturer gifts to physicians across different specialties, and (2) specifying analyses to allow for a nonlinear relationship between gifts and prescribing that may vary by specialty. Thus, our analyses shed light on how opioid manufacturers’ gifts might differentially flow to certain specialties and on how the associated response might vary by specialty.
METHODS
Data Sources
We used 2015 and 2016 Medicare National Part D Summary Public Use Files (PUF) to obtain physician prescribing information,16, 17 and identified patient fills of opioid drugs by linking the names of drugs in filled prescriptions to the PUF Drug Summary Tables and a list from the American Society of Addiction Medicine.18,19,20 We used the 2015 and 2016 Medicare Prescriber Summary PUF to obtain additional information about providers, including provider specialty, Part D claim counts, Medicare beneficiary counts, and summaries of Medicare beneficiaries.21, 22
Data on pharmaceutical industry gifts to opioid prescribers was extracted from 2014 and 2015 Complete Year Open Payments data, a database of gifts to clinicians from pharmaceutical and medical device companies compiled by the Centers for Medicaid and Medicaid Services (CMS).23, 24 Federal law mandates that pharmaceutical companies report data about to whom a gift was given, the kind of gift provided, the gift’s dollar value, and any products promoted in association with the gift. Gifts include meals, travel and lodging, education, consulting fees and honoraria, and “compensation for services other than consulting.” Consistent with prior research, we did not include research-related payments as gifts.3,4,5
Because the National Provider Identifier (NPI) used to identify providers in the Medicare data is not published in the Open Payments data, we used a publicly available crosswalk from ProPublica designed specifically to link these two datasets to match providers who appear in both.25 The ProPublica crosswalk matched > 99.7% of the physicians in the Open Payments database with the appropriate NPI using full name and practice location address.26
Study Population
We used the 2015 and 2016 Medicare National Part D prescription fill data to identify providers who had 11 or more fills by 11 or more beneficiaries for any opioid drug in 2015 or 2016 (numbers smaller than 11 are suppressed in the public use file). Fills of opioid medications were identified by matching brand and generic names with drugs flagged as opioids in the lists referenced above. Prescription fills for medications approved for treatment of opioid use disorder by the FDA, including buprenorphine and naloxone, were removed from the list (Appendix Table 3 is the final list of included opioid products).
Using the 2015 and 2016 Medicare Provider Summary data, we removed providers located in US territories from the sample. We also limited the sample to physicians based on providers’ NPPES specialty descriptions. We grouped physicians into one of seven broad specialties: primary care, surgery, psychiatry and neurology, rehabilitative and sports medicine, hematology and oncology, pain medicine and anesthesiology, and other non-surgical specialty (Appendix Table 4 lists the NPPES specialties included in each category).
Data on pharmaceutical industry gifts to opioid prescribers were extracted from Open Payments data. Open Payments records for matched physicians were examined to determine if gifts were related to the promotion of opioid products (as listed in Appendix Table 3).
Outcome Variable
The outcome variable was each physician’s quartile of opioid prescribing as a proportion of total prescribing among Medicare Part D patients. Because opioid prescribing patterns differ based on patient populations within each specialty, quartiles were defined within each of the specialty categories under study.
Exposure Variable
The exposure variable was the value of gifts in a calendar year paid by pharmaceutical companies to physicians related to an opioid medication categorized as follows: $0, more than $0 but under $20, $20 or more but under $100, and more than $100. Previous research has found that receiving a meal worth under $20 is associated with greater frequency of prescribing a drug, but more expensive meals were associated with slightly greater frequency of prescribing.27 The pharmaceutical industry recommends that educational items provided to physicians be $100 in value or less.28 Examining the amount paid nonparametrically allows us to examine whether different paid amounts are related to next-year opioid prescribing in different ways.
Covariate Measures
We calculated the dollar value of gifts paid to each physician by pharmaceutical companies for all drugs in a calendar year. We also calculated what percentage of opioid-related gifts to a physician specialty was paid by each company marketing opioid products. From the Part D Summary data, we calculated, for each specialty, the number of claims for opioids (including refills) and the total number of claims for all drugs including opioids. From the Prescriber Summary data, we extracted the following variables for each provider: number of beneficiaries in the year, average beneficiary age and average beneficiary hierarchical condition category (HCC) risk score, provider gender, and the proportion of prescribers included in the sample in each prescribing year (2015 or 2016).
Statistical Analysis
We used generalized ordinal logistic (GOL) regression models to assess, by specialty, the relationship between the value of gifts related to opioids and subsequent opioid prescribing in the following year.29 GOL models are appropriate because use of an ordered logit model violated the proportional odds assumption; i.e., the odds ratio estimates for the independent variables are different for each quartile of the outcome variable. To simplify the model, variables that were not significantly different between levels were constrained to meet the proportional odds assumption. Standard errors were clustered at the zip code level to account for regional prescribing patterns.
Adjusted models include the covariates listed above. Because different models were used to address each specialty group, we used a Bonferroni correction to identify the p value (p < .007) at which findings were considered statistically significant.30 We also conducted a sensitivity analysis using the same model to predict an outcome of opioid claims per beneficiary.
This research was supported by the National Institute on Drug Abuse (NIDA) under award R01DA045675. The University of Pittsburgh Institutional Review Board approved this study as exempt.
RESULTS
Table 1 shows characteristics of the study population. Our sample included 236,103 unique physicians over 2 years of Medicare prescribing (389,622 physician-years). Nearly half of the physicians were primary care providers (PCPs) (49.0%), 19.0% were surgeons, 2.9% were psychiatrists and neurologists, 2.1% were rehabilitative and sports medicine physicians, 4.5% were hematologists or oncologists, 2.7% were pain medicine and anesthesiology specialists, and 19.8% were other non-surgical specialists. Although on average physicians wrote 13.9% of their Medicare Part D prescriptions for opioids, there was significant variation by specialty; PCPs wrote 4.7% of prescriptions for opioids while pain management and anesthesiology specialists wrote 48.3% of prescriptions for opioids.
In our sample, physicians were given gifts by pharmaceutical companies valued at an average of $4029 in a calendar year (related to all drugs, including opioids). Across all specialties, an average of 1.7% of those gifts was related to opioid products. There was variation by specialty: PCPs received an average of $1076, of which an average of 1.0% ($15) was related to opioid products. Pain medicine and anesthesiology specialists received an average of $4151, of which an average of 18.2% ($1507) was related to opioid products. Surgical specialists received the most money, on average, from the industry, at nearly $11,000; 1.0% ($7) was related to opioid products.
Across all specialties, 14.1% of physician received gifts related to opioids with 2.6% receiving more than $100. This varied by specialty: among pain management and anesthesiology physicians, one-third received no opioid-related gifts, and another third received over $100.
Table 2 shows the proportion of opioid-related gift values that came from each opioid manufacturing company. Insys, which markets Subsys (fentanyl), was responsible for 42.6% of opioid-related gifts to physicians. Purdue, which marketed Hysingla ER (hydrocodone) and Oxycotin (oxycodone), was responsible for an additional 22.0% of opioid-related gifts to physicians. Purdue stopped marketing opioid drugs to physicians in February 2018.31 However, physicians in different specialties were gifted by different companies at different rates. Among surgeons, for example, one-half the value of opioid-related gifts were from Mallinckrodt (makers of Roxicode), which only contributed 6% of opioid-related gifts to physicians overall. Hematology and oncology physicians received nearly all of gifts (84.9%) from Insys (Subsys is marketed for breakthrough cancer pain). Insys provided only 7.6% of the value of gifts given to surgical specialists.
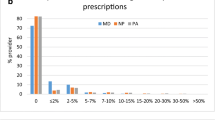
Figure 1 shows the unadjusted temporal relationship between opioid-related gifts to providers and the amount of opioid prescribing by specialty. Physicians who received $100 or more related to opioids are about 3.5 times as likely to be in the highest quartile of prescribing in the following year compared with the lowest quartile of prescribing.
Payments to prescribers related to opioid products by quartile of next-year prescribing and specialty. Quartiles of next-year prescribing by specialty (%): Primary Care (n = 190,900) Q1: 0.04–2.11 | Q2: 2.11–3.57 | Q3: 3.57–5.65 | Q4: 5.65–89.75; Surgical Specialty (n = 73,950) Q1: 0.18–23.30 | Q2: 22.30–36.36 | Q3: 36.36–49.96 | Q4: 50.00–100.00; Psychiatry and Neurology (n = 11,382) Q1: 0.04–1.02 | Q2: 1.02–2.23 | Q3: 2.23–5.05 | Q4: 5.05–83.61; Rehabilitative and Sports Medicine (n = 8093) Q1: 0.06–19.27 | Q2: 19.27–38.15 | Q3: 38.15–52.74 | Q4: 52.74–91.49; Hematology and Oncology (n = 17,322) Q1: 0.10–5.61 | Q2: 5.61–9.46 | Q3: 9.46–14.60 | Q4: 14.60–90.48; Pain Management and Anesthesiology (n = 10,667) Q1: 0.11–38.41 | Q2: 38.42–50.92 | Q3: 50.93–60.35 | Q4: 60.35–93.55; Other Non-surgical Specialty (n = 77,307) Q1: 0.04–1.87 | Q2: 1.87–4.71 | Q3: 4.71–13.89 | Q4: 13.89–94.12.
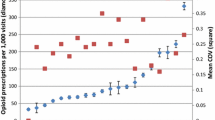
Figure 2 presents the adjusted results from the GOL regression models (full results are found in Appendix Table 5). By comparing the blue, red, and green points with the red line, we can see the likelihood of being in a higher quartile of prescribing if paid $1–$19, $20–$99, and $100+ related to opioids compared with $0, respectively. The temporal relationship between amount paid and next-year prescribing varied by specialty, but in general, receiving gifts related to opioids was associated with greater prescribing of opioids compared with same-specialty physicians in the next year.
Adjusted odds ratio of prescribing in higher versus lower quartiles by specialty and amount paid. Quartiles of next-year prescribing by specialty (%): Primary Care (n = 190,900) Q1: 0.04–2.11 | Q2: 2.11–3.57 | Q3: 3.57–5.65 | Q4: 5.65–89.75; Surgical Specialty (n = 73,950) Q1: 0.18–23.30 | Q2: 22.30–36.36 | Q3: 36.36–49.96 | Q4: 50.00–100.00; Psychiatry and Neurology (n = 11,382) Q1: 0.04–1.02 | Q2: 1.02–2.23 | Q3: 2.23–5.05 | Q4: 5.05–83.61; Rehabilitative and Sports Medicine (n = 8093) Q1: 0.06–19.27 | Q2: 19.27–38.15 | Q3: 38.15–52.74 | Q4: 52.74–91.49; Hematology and Oncology (n = 17,322) Q1: 0.10–5.61 | Q2: 5.61–9.46 | Q3: 9.46–14.60 | Q4: 14.60–90.48; Pain Management and Anesthesiology (n = 10,667) Q1: 0.11–38.41 | Q2: 38.42–50.92 | Q3: 50.93–60.35 | Q4: 60.35–93.55; Other Non-surgical Specialty (n = 77,307) Q1: 0.04–1.87 | Q2: 1.87–4.71 | Q3: 4.71–13.89 | Q4: 13.89–94.12.
Primary care physicians are nearly 3.5 times as likely (aOR 3.40 [CI 2.99–3.86]) to be in the highest quartile of prescribing versus the lower quartiles if they are paid $100 or more, as demonstrated by the green point labeled “Quart. 4 vs Quart. 1-3.” They are at least 60% more likely to be in a higher quartile of prescribing if they are paid between $1 and $19 related to opioids, as demonstrated by the blue points in Figure 2 (quartiles 2–4 vs quartile 1 aOR 1.79 [CI 1.66–1.92], quartiles 3–4 vs quartiles 1–2 aOR 1.65 [CI 1.56–1.75], quartile 4 vs quartiles 1–3 aOR 1.60 [CI 1.51–1.71]).
Psychiatrists and neurologists have a strong relationship between pharmaceutical company gifts and next-year opioid prescribing, especially for larger gifts: physicians in this category who were paid $100 or more were seven to thirteen times as likely to be in a higher quartile of opioid prescribing compared with colleagues paid $0 in the preceding year, as seen by the green points in that specialty’s graph (quartiles 2–4 vs quartile 1 aOR 8.86 [CI 5.13—15.32], quartiles 3–4 vs quartiles 1–2 aOR 7.62 [CI 5.12–11.35], quartile 4 vs quartiles 1–3 aOR 12.59 [CI 8.85–17.92]). Smaller gifts also increased the likelihood of being in higher quartiles of prescribing at least 46% at all levels of prescribing. Among surgeons, the likelihood of being in a higher quartile of prescribing increased by 50% (aOR 1.51 [CI 1.15–1.98]) at all volumes of prescribing for physicians paid $100 versus $0 in opioid-related gifts. For smaller gifts, the relationship weakens as opioid prescribing increases in comparison with other surgeons. Among rehabilitative and sports medicine physicians, receiving between $1 and $19 related to opioids instead of $0 increased the likelihood of being outside the lowest quartile of opioid prescribing by 62% (aOR 1.62 [CI 1.31–2.00]), while receiving $20–$99 more than doubled that likelihood (aOR 2.33 [CI 1.80–3.02]) and receiving $100 or more nearly quintupled it (4.79 [CI 3.45–6.64]). For these specialists, the strength of the relationship between gift values and increasing prescribing decreased at higher levels of prescribing. Oncologists were 50% more likely (aOR 1.46 [CI 1.03–2.07]) to be in the highest quartile of opioid prescribing if they had received $100 or more in gifts related to opioids in the prior year. Gifts of smaller amounts, however, were not related to opioid prescribing.
Among pain management specialists and anesthesiologists, gifts of under $20 were not associated with prescribing. Gifts of $20 or more were related to higher prescribing with the strength of that relationship decreasing at higher levels of prescribing. There appears to be no substantive difference between gifts worth $20–$99 and gifts at $100 or more. The likelihood of being in the highest quartile of prescribing is 38% higher (aOR 1.38 [CI 1.13–1.67]) for physicians in this subgroup who received gifts worth $100 or more and 42% higher (aOR 1.42 [CI 1.16–1.73]) for gifts worth $20–$99. Other non-surgical specialists were over five times as likely to be in the highest quartile of prescribing versus a lower one if they received opioid-related gifts of $100 or more in the previous year (aOR 5.60 [CI 3.45–9.09]). The relationship between small gifts and prescribing decreased as prescribing volumes increased—other non-surgical specialists being paid between $1 and $19 related to opioids, for example, are 2.3 times as likely than those being paid $0 to be outside the lowest quartile, but only 1.2 times as likely to be in the highest quartile (aOR 2.31 [CI 1.87–2.84], aOR 1.23 [CI 0.96–1.57]).
Our sensitivity analysis examined the relationship between amount paid related to opioids and opioid claims per Medicare beneficiary in the following year (as opposed to the primary specification of percent of total prescribing for opioids). Results were consistent in terms of direction and magnitude of the associations between pharmaceutical gifts and opioid prescribing (see Appendix Table 6 for details).
DISCUSSION
Our findings suggest that first, although multiple specialties prescribe opioids, the manufacturers of opioids vary the value of gifts substantially by provider specialty. Second, the relationship between the value of opioid-related gifts and prescribing behavior in the following year also varies substantially. The observed temporal relationship between gifts from pharmaceutical companies and prescribing is consistent with existing research.3, 8, 27, 32,33,34,35 We fill several gaps to better understand real-world behavior of providers and their relationships with pharmaceutical companies.
Our findings shed light on differences in the relationship between the dollar value of opioid-related gifts and prescribing behavior in different medical specialties. Opioid-related gifts to hematologists and oncologists are weakly associated with next-year opioid prescribing, even when these physicians are gifted $100 or more. In contrast, there is a strong association between opioid-related gifts and opioid prescribing among psychiatrists and neurologists, particularly when these physicians are gifted at least $20. Future research should identify why these relationships are so different, considering differences in training, patient populations, and other financial incentives received between specialties.
Second, our findings suggest that the marginal effect of each dollar is likely not identical, and the effect of the gift may have different impacts at different levels of prescribing. For example, among rehabilitative and sports medicine physicians, receiving $100 or more in gifts was not related to being in the top quartile of prescribing versus the bottom three any more than $1–$19 gifts were, but it was strongly related with being outside the bottom quartile of prescribing. While even small gifts are related to increased prescribing in many cases, placing limits on the value of gifts that physicians can receive from pharmaceutical companies related to opioids may reduce pharmaceutical company–influenced opioid prescribing.
Third, our study is the first to characterize patterns of opioid promotion to physicians of different specialties by 19 different companies. Two companies responsible for nearly two-thirds of the value of opioid-related gifts have settled lawsuits for hundreds of millions of dollars related to opioid promotion. CEOs at Insys, the company responsible for 40% of opioid-related gifts to physicians, were recently found guilty of “paying doctors to write prescriptions for a much wider pool of patients than the drug was approved for” between 2012 and 2015.10 Insys recently entered a $225 million global resolution of investigations with the Department of Justice.13 Our data show that, in almost every specialty, physicians receiving gifts related to opioids received at least 25% of the value of those gifts from Insys. Purdue, which paid a $270 million civil settlement in Oklahoma, was responsible for one-fifth of the value of all opioid-related gifts in 2014 and 2015.11, 12 These settlements may have implications for future and ongoing litigation.
Opioid-related gifts have been associated with overdose mortality, with county-level retail opioid prescriptions dispensed as a significant mediating factor.4 OUD is estimated to be a more frequent chronic condition in the Medicare population (the source of our prescribing data) than among those with commercial insurance,36 and high-dose chronic opioid use has increased, particularly among disabled Medicare beneficiaries, in the last decade.37 State-level opioid prescribing restrictions have not been shown to reduce overdose among Medicare beneficiaries,38 and opioid misuse remains high among Medicare beneficiaries.39 Our findings can inform Medicare, health systems, and pharmaceutical firm efforts to identify interventions to reduce opioid overprescribing.
This study has limitations. First, our sample is limited to physicians who prescribe to patients enrolled in Medicare Part D (although fewer than 1% of physicians have formally opted out of Medicare40) who we were able to match to the Open Payments database using the ProPublica crosswalk, and may not be generalizable to other physicians. However, we note that ProPublica has matched over 99.7% of the providers in the Open Payments database.25 Second, physicians are included in the Open Payments database and therefore our sample only if they received gifts from any pharmaceutical companies or medical device manufacturers (for opioids or any other drug) in either 2014 or 2015. The opioid prescribing of physicians who have not received gifts in these years may be different, and the direction of possible bias is unclear. In 2015, approximately half of all US physicians received gifts from pharmaceutical companies and medical device manufacturers, which provides high generalizability for our study.41 Third, we cannot eliminate the possibility of reverse causation (i.e., opioid manufacturers give gifts to physicians who prescribe at high levels). Evidence from social science literature does indicate that giftgiving influences behavior (for example, including a gift in a mailing requesting donations nearly doubled the response rate),42, 43 but there is also evidence that pharmaceutical companies market their products more heavily towards physicians with already high levels of prescribing.44 While we sought to minimize this threat to validity by examining the temporal relationship between gifts and prescribing in the calendar year after gifts were given, we recognize that prescribing patterns in 2016 will likely be highly correlated with 2015 prescribing patterns, thereby not truly eliminating the possibility of reverse causation. We note, however, that if gifts were primarily provided as reinforcement for prior prescribing, we might expect to see a more consistent dose-response relationship, where more prescribing is consistently associated with larger gifts. While true in many cases, it is not always the case; there are several specialties (surgery, hematology and oncology) where $100+ gifts are similar to $1–$19 gifts. As a result, any discussions of causality must be made with appropriate caution until future research is better able to examine this important issue. Finally, we were unable to measure the appropriateness of Part D opioid prescribing, so it is possible that increases in prescribing were related to increases in diagnoses warranting the prescribing of opioids.
Despite these limitations, our findings make an important contribution to our understanding of the association between pharmaceutical gifts and opioid prescribing. While a large majority of physicians who prescribe opioids do not receive gifts from pharmaceutical companies related to opioids, even very small gifts are related to increased prescribing in the subsequent year compared with those who received no gifts, and among some specialties, larger gifts are related to an increased likelihood of increased prescribing compared with those who received smaller gifts. Perhaps with some awareness of this relationship, many hospitals, health systems, and physicians themselves are already limiting their financial relationships with pharmaceutical companies.45, 46 Medical specialty boards may have a role to play in encouraging their members reassess their remaining relationships with pharmaceutical companies, particularly for specialties with strong associations between pharmaceutical gifts and subsequent opioid prescribing. As efforts continue to eliminate prescription opioid overdose deaths by limiting unnecessary opioid prescribing, our findings suggest that the relationships between physicians and pharmaceutical companies warrant greater review
References
2017. Centers for Disease Control Prescription Opioid Data. Accessed at Centers for Disease Control at https://www.cdc.gov/drugoverdose/data/prescribing.html
Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain--United States, 2016. JAMA. 2016;315(15):1624-45.
Hadland SE, Cerda M, Li Y, Krieger MS, Marshall BDL. Association of Pharmaceutical Industry Marketing of Opioid Products to Physicians With Subsequent Opioid Prescribing. JAMA Intern Med 2018;178(6):861-3.
Hadland SE, Rivera-Aguirre A, Marshall BDL, Cerda M. Association of Pharmaceutical Industry Marketing of Opioid Products With Mortality From Opioid-Related Overdoses. JAMA Netw Open 2019;2(1):e186007.
Hadland SE, Krieger MS, Marshall BDL. Industry Payments to Physicians for Opioid Products, 2013-2015. Am J Public Health 2017;107(9):1493-5.
Gibbons RV, Landry FJ, Blouch DL, Jones DL, Williams FK, Lucey CR, et al. A comparison of physicians’ and patients’ attitudes toward pharmaceutical industry gifts. J Gen Intern Med 1998;13(3):151-4.
Caudill TS, Johnson MS, Rich EC, McKinney WP. Physicians, pharmaceutical sales representatives, and the cost of prescribing. Arch Fam Med 1996;5(4):201-6.
Dana J, Loewenstein G. A social science perspective on gifts to physicians from industry. JAMA. 2003;290(2):252-5.
Babcock L, Loewenstein G, Issacharoff S. Creating Convergence: Debiasing Biased Litigants. Law Soc Inq 1997;22(4):913-25.
Emanuel G, Thomas K. Top Executives of Insys, an Opioid Company, Are Found Guilty of Racketeering. The New York Times. New York.
Dolmetsch C. Purdue’s Sackler Family Must Face Opioid Suits in New York. Bloomberg. New York.
Hoffman J. Purdue Pharma and Sacklers Reach $270 Million Settlement in Opioid Lawsuit. The New York Times, New York.
Opioid Manufacturer Insys Therapeutics Agrees to Enter $225 Million Global Resolution of Criminal and Civil Investigations. Company Admits Illegal Conduct Regarding Promotion of Subsys, a Powerful Opioid Painkiller. 19-621 ed: Department of Justice Office of Public Affairs; 2019.
Magnus SA. Physicians’ financial incentives in five dimensions: a conceptual framework for HMO managers. Health Care Manag Rev 1999;24(1):57-72.
Levy B, Paulozzi L, Mack KA, Jones CM. Trends in Opioid Analgesic-Prescribing Rates by Specialty, U.S., 2007-2012 Am J Prev Med 2015;49(3):409-13.
Centers for Medicare & Medicaid Services. Medicare Provider Utilization and Payment Data: Part D Prescriber Summary table, CY2015. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/PartD2015.html.
Centers for Medicare & Medicaid Services. Medicare Provider Utilization and Payment Data: Part D Prescriber Summary table, CY2016. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/PartD2016.html.
Centers for Medicare & Medicaid Services. Medicare Provider Utilization and Payment Data: Part D Drug National Summary table, CY2015. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/PartD2015.html.
Centers for Medicare & Medicaid Services. Medicare Provider Utilization and Payment Data: Part D Drug National Summary table, CY2016. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/PartD2016.html.
Opioids: Brand names, generic names & street names. It Matters Colorado.
Centers for Medicare & Medicaid Services. Medicare Provider Utilization and Payment Data: Part D Prescriber PUF NPI Drug table, CY2015. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/PartD2015.html.
Centers for Medicare & Medicaid Services. Medicare Provider Utilization and Payment Data: Part D Prescriber PUF NPI Drug table, CY2016. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/PartD2016.html.
Centers for Medicare & Medicaid Services. Complete 2014 Program Year Open Payments Dataset. https://www.cms.gov/OpenPayments/Explore-the-Data/Dataset-Downloads.html.
Centers for Medicare & Medicaid Services. Complete 2015 Program Year Open Payments Dataset. https://www.cms.gov/OpenPayments/Explore-the-Data/Dataset-Downloads.html.
Tigas M, Jones RG, Ornstein C, Groeger L. Dollars for Docs NPI/Open Payments Crosswalk.
Jones RG, Ornstein C. Matching Industry Payments to Medicare Prescribing Patterns: An Analysis. ProPublica, Manhattan; 2016.
DeJong C, Aguilar T, Tseng CW, Lin GA, Boscardin WJ, Dudley RA. Pharmaceutical Industry-Sponsored Meals and Physician Prescribing Patterns for Medicare Beneficiaries. JAMA Intern Med 2016;176(8):1114-22.
PhRMA. Code on Interactions with Healthcare Professionals. 2008.
Williams R. Generalized ordered logit/partial proportional odds models for ordinal dependent variables. Stata J 2006;6(1):58-82.
Armstrong RA. When to use the Bonferroni correction. Ophthalmic Physiol Opt 2014;34(5):502-8.
2018. McCausland P, Connor T OxyContin maker Purdue to stop promoting opioids in light of epidemic. Accessed at NBC News at https://www.nbcnews.com/storyline/americas-heroin-epidemic/oxycontin-maker-purdue-stop-promoting-opioids-light-epidemic-n846726 on March 18, 2019.
Fleischman W, Agrawal S, King M, Venkatesh AK, Krumholz HM, McKee D, et al. Association between payments from manufacturers of pharmaceuticals to physicians and regional prescribing: cross sectional ecological study. BMJ 2016;354.
Lo B, Grady D. Payments to Physicians: Does the Amount of Money Make a Difference? JAMA. 2017;317(17).
Wood SF, Podrasky J, McMonagle MA, Raveendran J, Bysshe T, Hogenmiller A, et al. Influence of pharmaceutical marketing on Medicare prescriptions in the District of Columbia. PLoS One 2017;12(10):e0186060.
Yeh JS, Franklin JM, Avorn J, Landon J, Kesselheim AS. Association of Industry Payments to Physicians With the Prescribing of Brand-name Statins in Massachusetts. JAMA Intern Med 2016;176(6):763-8.
Dufour R, Joshi AV, Pasquale MK, Schaaf D, Mardekian J, Andrews GA, et al. The prevalence of diagnosed opioid abuse in commercial and Medicare managed care populations. Pain Pract 2014;14(3):E106-15.
Anderson KK, Hendrick F, McClair V. National Trends in High-dose Chronic Opioid Utilization among Dually Eligible and Medicare-only Beneficiaries (2006-2015). Data Analysis Brief: Center for Medicare and Medicaid Services; 2018.
Meara E, Horwitz JR, Powell W, McClelland L, Zhou W, O’Malley AJ, et al. State Legal Restrictions and Prescription-Opioid Use among Disabled Adults. N Engl J Med 2016;375(1):44-53.
Carey CM, Jena AB, Barnett ML. Patterns of Potential Opioid Misuse and Subsequent Adverse Outcomes in Medicare, 2008 to 2012. Ann Intern Med 2018;168(12):837-45.
Boccuti C, Swoope C, Damico A, Neuman T. Medicare Patients’ Access to Physicians: A Synthesis of the Evidence. Kaiser Family Foundation, San Francisco; 2013.
Tringale KR, Marshall D, Mackey TK, Connor M, Murphy JD, Hattangadi-Gluth JA. Types and Distribution of Payments From Industry to Physicians in 2015. JAMA. 2017;317(17):1774-84.
Cialdini RB. Influence: The Psychology of Persuasion: Harper Business; 1993.
Katz D, Caplan AL, Merz JF. All Gifts Large and Small: Toward an Understanding of the Ethics of Pharmaceutical Industry Gift Giving. Am J Bioeth 2003;3(3):39-46.
Manchanda P, Xie Y, Youn N. The Role of Targeted Communication and Contagion in Product Adoption. Mark Sci 2008;27(6):961-76.
Commercial Access to Physicians: Medical Industry Sales Reps Accessibility to U.S. Physicians. Irvine, CA: SK&A; 2017.
Larkin I, Ang D, Steinhart J, Chao M, Patterson M, Sah S, et al. Association Between Academic Medical Center Pharmaceutical Detailing Policies and Physician Prescribing. JAMA. 2017;317(17):1785-95.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 68.9 kb)
Rights and permissions
About this article
Cite this article
Hollander, M.A.G., Donohue, J.M., Stein, B.D. et al. Association between Opioid Prescribing in Medicare and Pharmaceutical Company Gifts by Physician Specialty. J GEN INTERN MED 35, 2451–2458 (2020). https://doi.org/10.1007/s11606-019-05470-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-019-05470-0