Abstract
Background
The benefit of anatomic (AR) versus parenchyma-sparing resection (PSR) in hepatocarcinoma (HCC) is still debated. The aim of the study was to compare AR vs. PSR in terms of overall survival (OS) and disease-free survival (DFS).
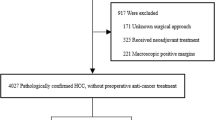
Methods
A systematic review was conducted using Medline and Google Scholar. To reduce intra- and inter-study heterogeneity, only propensity-matched studies and randomized clinical trials (RCT) were evaluated and a generic inverse variance meta-analysis was run. A sub-analysis was performed in case of tumor microvascular invasion (MVI).
Results
Eleven propensity-matched and one RCT were evaluated, with a total of 3445 patients (AR = 1776 and PSR = 1669). Tumor burden and liver function were comparable among studies (I2 < 50%, p > 0.5). OS was similar between AR and PSR (HR 0.93; 95%CI, 0.75–1.15; p = 0.50, I2 = 41%). DFS was improved in AR at 1 year (RR 0.84; 95%CI, 0.72–0.97; p = 0.02; I2 = 36%) and 3 years (RR 0.90; 95%CI, 0.83–0.98; p = 0.02; I2 = 40%) but not at 5 years (RR 0.94; 95%CI, 0.87–1.01; p = 0.07; I2 = 41%). Furthermore, in the presence of MVI, no difference in OS and DFS was observed between AR and PSR.
Conclusion
When liver function and tumor burden are comparable, AR and PSR achieved similar overall survival. AR improved local control in the early period after surgery. Furthermore, in the presence of MVI, the extension of surgery was not associated with better OS and DFS.




Similar content being viewed by others
References
Lafaro KJ, Demirjian AN, Pawlik TM. Epidemiology of hepatocellular carcinoma. Surg Oncol Clin N Am 2015;24:1–17.
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin 2011;61:69–90.
Grazi GL, Ercolani G, Pierangeli F, Del Gaudio M, Cescon M, Cavallari A, et al. Improved results of liver resection for hepatocellular carcinoma on cirrhosis give the procedure added value. Ann Surg 2001;234:71–8.
Poon RT-P, Fan ST, Lo CM, Liu CL, Wong J. Long-Term Survival and Pattern of Recurrence After Resection of Small Hepatocellular Carcinoma in Patients With Preserved Liver Function. Annals of Surgery 2002;235:373–82. doi:https://doi.org/10.1097/00000658-200203000-00009.
Spolverato G, Vitale A, Ejaz A, Kim Y, Maithel SK, Cosgrove DP, et al. The relative net health benefit of liver resection, ablation, and transplantation for early hepatocellular carcinoma. World J Surg 2015;39:1474–84.
Kang KJ, Ahn KS. Anatomical resection of hepatocellular carcinoma: A critical review of the procedure and its benefits on survival. World J Gastroenterol 2017;23:1139–46.
Kim S, Kim S, Song I, Chun K. Comparison of survival outcomes after anatomical resection and non-anatomical resection in patients with hepatocellular carcinoma. Korean Journal of Hepato-Biliary-Pancreatic Surgery 2015;19:161. doi:https://doi.org/10.14701/kjhbps.2015.19.4.161.
Hirokawa F, Kubo S, Nagano H, Nakai T, Kaibori M, Hayashi M, et al. Do patients with small solitary hepatocellular carcinomas without macroscopically vascular invasion require anatomic resection? Propensity score analysis. Surgery 2015;157:27–36.
Li S-Q, Huang T, Shen S-L, Hua Y-P, Hu W-J, Kuang M, et al. Anatomical versus non-anatomical liver resection for hepatocellular carcinoma exceeding Milan criteria. Br J Surg 2017;104:118–27.
Eltawil KM, Kidd M, Giovinazzo F, Helmy AH, Salem RR. Differentiating the impact of anatomic and non-anatomic liver resection on early recurrence in patients with Hepatocellular Carcinoma. World Journal of Surgical Oncology 2010;8:43. doi:https://doi.org/10.1186/1477-7819-8-43.
Famularo S, Di Sandro S, Giani A, Lauterio A, Sandini M, De Carlis R, et al. Long-term oncologic results of anatomic vs. parenchyma-sparing resection for hepatocellular carcinoma. A propensity score-matching analysis. Eur J Surg Oncol 2018;44:1580–7.
Makuuchi M, Hasegawa H, Yamazaki S. Ultrasonically guided subsegmentectomy. Surg Gynecol Obstet 1985;161:346–50.
Sakon M, Nagano H, Nakamori S, Dono K, Umeshita K, Murakami T, et al. Intrahepatic recurrences of hepatocellular carcinoma after hepatectomy: analysis based on tumor hemodynamics. Arch Surg 2002;137:94–9.
Regimbeau J-M, Kianmanesh R, Farges O, Dondero F, Sauvanet A, Belghiti J. Extent of liver resection influences the outcome in patients with cirrhosis and small hepatocellular carcinoma. Surgery 2002;131:311–7.
Hasegawa K, Kokudo N, Imamura H, Matsuyama Y, Aoki T, Minagawa M, et al. Prognostic impact of anatomic resection for hepatocellular carcinoma. Ann Surg 2005;242:252–9.
Shindoh J, Makuuchi M, Matsuyama Y, Mise Y, Arita J, Sakamoto Y, et al. Complete removal of the tumor-bearing portal territory decreases local tumor recurrence and improves disease-specific survival of patients with hepatocellular carcinoma. J Hepatol 2016;64:594–600.
Marubashi S, Gotoh K, Akita H, Takahashi H, Ito Y, Yano M, et al. Anatomical versus non-anatomical resection for hepatocellular carcinoma. Br J Surg 2015;102:776–84.
Okamura Y, Ito T, Sugiura T, Mori K, Uesaka K. Anatomic versus nonanatomic hepatectomy for a solitary hepatocellular carcinoma : a case-controlled study with propensity score matching. J Gastrointest Surg 2014;18:1994–2002.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 2010;8:336–41.
Luchini C, Stubbs B, Solmi M, Veronese N. Assessing the quality of studies in meta-analyses: Advantages and limitations of the Newcastle Ottawa Scale. World Journal of Meta-Analysis 2017;5:80. doi:https://doi.org/10.13105/wjma.v5.i4.80.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603–5.
Quality AFHRA, Agency for Healthcare Research and Quality. National Healthcare Quality Report, 2012. PsycEXTRA Dataset 2013. doi:https://doi.org/10.1037/e553742013-001.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Medical Research Methodology 2005;5. doi:https://doi.org/10.1186/1471-2288-5-13.
Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med 1998;17:2815–34.
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 2007;8:16.
Zhao H, Chen C, Gu S, Yan X, Jia W, Mao L, et al. Anatomical versus non-anatomical resection for solitary hepatocellular carcinoma without macroscopic vascular invasion: A propensity score matching analysis. J Gastroenterol Hepatol 2017;32:870–8.
Ishii M, Mizuguchi T, Kawamoto M, Meguro M, Ota S, Nishidate T, et al. Propensity score analysis demonstrated the prognostic advantage of anatomical liver resection in hepatocellular carcinoma. World J Gastroenterol 2014;20:3335–42.
Kaibori M, Kon M, Kitawaki T, Kawaura T, Hasegawa K, Kokudo N, et al. Comparison of anatomic and non-anatomic hepatic resection for hepatocellular carcinoma. J Hepatobiliary Pancreat Sci 2017;24:616–26.
Hidaka M, Eguchi S. Impact of Anatomical Resection for Hepatocellular Carcinoma with Micro-portal Invasion (vp1): A Multi-institutional Study by the Kyushu Study Group of Liver Surgery. HPB 2018;20:S391. doi:https://doi.org/10.1016/j.hpb.2018.06.2692.
Cucchetti A, Qiao G-L, Cescon M, Li J, Xia Y, Ercolani G, et al. Anatomic versus nonanatomic resection in cirrhotic patients with early hepatocellular carcinoma. Surgery 2014;155:512–21.
Feng X, Su Y, Zheng S, Xia F, Ma K, Yan J, et al. A double blinded prospective randomized trial comparing the effect of anatomic versus non-anatomic resection on hepatocellular carcinoma recurrence. HPB 2017;19:667–74. doi:https://doi.org/10.1016/j.hpb.2017.04.010.
Ye JZ, Miao ZG, Wu FX, Zhao YN, Ye HH, Li LQ. Recurrence after anatomic resection versus nonanatomic resection for hepatocellular carcinoma: a meta-analysis. Asian Pac J Cancer Prev 2012;13:1771–7.
Zhou Y, Xu D, Wu L, Li B. Meta-analysis of anatomic resection versus nonanatomic resection for hepatocellular carcinoma. Langenbeck’s Archives of Surgery 2011;396:1109–17. doi:https://doi.org/10.1007/s00423-011-0784-9.
Moris D, Tsilimigras DI, Kostakis ID, Ntanasis-Stathopoulos I, Shah KN, Felekouras E, et al. Anatomic versus non-anatomic resection for hepatocellular carcinoma: A systematic review and meta-analysis. Eur J Surg Oncol 2018;44:927–38.
Tan Y, Zhang W, Jiang L, Yang J, Yan L. Efficacy and safety of anatomic resection versus nonanatomic resection in patients with hepatocellular carcinoma: A systemic review and meta-analysis. PLoS One 2017;12:e0186930.
Huang X, Lu S. A Meta-analysis comparing the effect of anatomical resection vs. non-anatomical resection on the long-term outcomes for patients undergoing hepatic resection for hepatocellular carcinoma. HPB 2017;19:843–9. doi:https://doi.org/10.1016/j.hpb.2017.06.003.
Cucchetti A, Cescon M, Ercolani G, Bigonzi E, Torzilli G, Pinna AD. A comprehensive meta-regression analysis on outcome of anatomic resection versus nonanatomic resection for hepatocellular carcinoma. Ann Surg Oncol 2012;19:3697–705.
D’Agostino RB. Adjustment Methods: Propensity Score Methods for Bias Reduction in the Comparison of a Treatment to a Non-Randomized Control Group. Tutorials in Biostatistics 2005:67–83. doi:https://doi.org/10.1002/0470023678.ch1b.
Xu X-L, Liu X-D, Liang M, Luo B-M. Radiofrequency Ablation versus Hepatic Resection for Small Hepatocellular Carcinoma: Systematic Review of Randomized Controlled Trials with Meta-Analysis and Trial Sequential Analysis. Radiology 2018;287:461–72.
Witowski J, Rubinkiewicz M, Mizera M, Wysocki M, Gajewska N, Sitkowski M, et al. Meta-analysis of short- and long-term outcomes after pure laparoscopic versus open liver surgery in hepatocellular carcinoma patients. Surgical Endoscopy 2019;33:1491–507. doi:https://doi.org/10.1007/s00464-018-6431-6.
Calise F, Giuliani A, Sodano L, Crolla E, Bianco P, Rocca A, et al. Segmentectomy: is minimally invasive surgery going to change a liver dogma? Updates Surg 2015;67:111–5.
Portolani N, Coniglio A, Ghidoni S, Giovanelli M, Benetti A, Tiberio GAM, et al. Early and Late Recurrence After Liver Resection for Hepatocellular Carcinoma. Annals of Surgery 2006;243:229–35. doi:https://doi.org/10.1097/01.sla.0000197706.21803.a1.
Chan AWH, Zhong J, Berhane S, Toyoda H, Cucchetti A, Shi K, et al. Development of pre and post-operative models to predict early recurrence of hepatocellular carcinoma after surgical resection. J Hepatol 2018;69:1284–93.
Yamamoto J, Kosuge T, Takayama T, Shimada K, Yamasaki S, Ozaki H, et al. Recurrence of hepatocellular carcinoma after surgery. Br J Surg 1996;83:1219–22.
Wang Z, Luo L, Cheng Y, He G, Peng B, Gao Y, et al. Correlation Between Postoperative Early Recurrence of Hepatocellular Carcinoma and Mesenchymal Circulating Tumor Cells in Peripheral Blood. J Gastrointest Surg 2018;22:633–9.
Acknowledgments
The authors are grateful to Davide Paolo Bernasconi, PhD (Center of Biostatistics for Clinical Epidemiology, School of Medicine and Surgery, University of Milan-Bicocca, Italy), for his contribution to the statistical analysis.
Authors’ Contribution Statement
Each author has contributed the same to the manuscript. In particular, each physician has met all the following: substantial contributions to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published; and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 110 kb)
Rights and permissions
About this article
Cite this article
Famularo, S., Ceresoli, M., Giani, A. et al. Is It Just a Matter of Surgical Extension to Achieve the Cure of Hepatocarcinoma? A Meta-Analysis of Propensity-Matched and Randomized Studies for Anatomic Versus Parenchyma-Sparing Liver Resection. J Gastrointest Surg 25, 94–103 (2021). https://doi.org/10.1007/s11605-019-04494-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04494-5