Abstract
Introduction
Neoadjuvant therapy (NT) is the standard of care for clinical stage II-III rectal adenocarcinoma, but utilization remains suboptimal. We aimed to determine the underlying reasons for omission of local staging and NT.
Methods
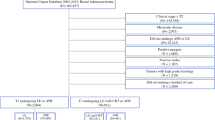
We conducted a retrospective study of patients with clinical stage II-III or undocumented clinical stage/pathologic stage II-III rectal adenocarcinoma who were treated in 2010–2016 in one of nine Intermountain Healthcare hospitals. The outcomes of omission of local staging and NT were examined with multivariable models. Risk- and reliability-adjusted rates of local staging and NT were calculated for surgeons who treated ≥ 3 patients. Pathologic and long-term outcomes were examined after excluding patients who were not resected or who underwent local excision (N = 11).
Results
Local staging was omitted in 43/240 (17.9%) patients and NT was omitted in 41/240 (17.1%). The strongest risk factors for local staging and NT omission were upper rectal tumors and surgeons who treated ≤ 3 cases/year. Thirty-six of 41 (87.8%) cases of omitted NT had local staging omitted. Adjusted surgeon-specific local staging rates varied 1.6-fold (56.3–92.4%) and NT rates varied 2.8-fold (34.1–97.1%). Surgeon local staging and NT rates were strongly correlated (r = 0.92). NT was associated with lower rates of positive circumferential radial margins (7.9 vs. 20.0%; P = 0.02), node positivity (33.3 vs. 55.0%; P = 0.01), and local recurrences (7.6 vs. 14.9% at 5 years; P = 0.0176).
Conclusions
NT omission should be understood as a consequence of surgeon failure to perform local staging in most cases. Quality improvement efforts should focus on improving utilization of local staging.


Similar content being viewed by others
References
Monson JR, Probst CP, Wexner SD, Remzi FH, Fleshman JW, Garcia-Aguilar J, Chang GJ, Dietz DW, Consortium for Optimizing the Treatment of Rectal C. Failure of evidence-based cancer care in the United States: the association between rectal cancer treatment, cancer center volume, and geography. Ann Surg. 2014;260(4):625–31; discussion 31-2. doi:https://doi.org/10.1097/SLA.0000000000000928.
Sauer R, Becker H, Hohenberger W, Rodel C, Wittekind C, Fietkau R, Martus P, Tschmelitsch J, Hager E, Hess C, Karstens J, Liersch T, Schmidberger H, Raab R, GRCS Group. Preoperative versus Postoperative Chemoradiotherapy for Rectal Cancer. NEJM. 2004;351(17):1731–40.
NCCN Clinical Practice Guidelines in Oncology: Rectal Cancer. Version 3.17. [cited May 15, 2018]. Available at: https://www.nccn.org/professionals/physician_gls/pdf/rectal.pdf.
Sineshaw HM, Jemal A, Thomas CR, Jr., Mitin T. Changes in treatment patterns for patients with locally advanced rectal cancer in the United States over the past decade: An analysis from the National Cancer Data Base. Cancer. 2016;122(13):1996–2003. doi:https://doi.org/10.1002/cncr.29993.
Midura E, Jung, AD, Daly, MC, Hansenman, DJ, Shah, SA, Paquette, IM. Cancer Center Volume and Type Impact Stage-Specific Utilization of Neoadjuvant Therapy in Rectal Cancer. Dig Dis Sci. 2017;62(8):1906–12.
Delitto D, George TJ, Jr., Loftus TJ, Qiu P, Chang GJ, Allegra CJ, Hall WA, Hughes SJ, Tan SA, Shaw CM, Iqbal A. Prognostic Value of Clinical vs Pathologic Stage in Rectal Cancer Patients Receiving Neoadjuvant Therapy. J Natl Cancer Inst. 2018;110(5):460–6. doi:https://doi.org/10.1093/jnci/djx228.
Wexner S, Berho ME,. The Rationale for and Reality of the New National Accreditation Program for Rectal Cancer. Dis Colon Rectum. 2017;60(6):595–602.
Dietz DW, Consortium for Optimizing Surgical Treatment of Rectal C. Multidisciplinary management of rectal cancer: the OSTRICH. J Gastrointest Surg. 2013;17(10):1863–8. doi:https://doi.org/10.1007/s11605-013-2276-4.
Glasgow SC, Morris AM, Baxter NN, Fleshman JW, Alavi KS, Luchtefeld MA, Monson JR, Chang GJ, Temple LK. Development of The American Society of Colon and Rectal Surgeons’ Rectal Cancer Surgery Checklist. Dis Colon Rectum. 2016;59(7):601–6. doi:https://doi.org/10.1097/DCR.0000000000000606.
Lee L, Dietz D, Fleming F, Remzi F, Wexner S, Winchester D, Monson J. Accreditation Readiness in US Multidisciplinary Rectal Cancer Care: A Survey of OSTRICH Member Institutions. JAMA Surg. 2018;153(4):388–90.
Orangio GR. A National Accreditation Program for Rectal Cancer: A Long and Winding Road. Dis Colon Rectum. 2018;61(2):145–6. doi:https://doi.org/10.1097/DCR.0000000000001011.
Commision on Cancer Measures for Quality of Cancer Care. [cited October 9, 2017]. Available at https://www.facs.org/quality-programs/cancer/ncdb/qualitymeasures.
Brady JT, Xu Z, Scarberry KB, Saad A, Fleming FJ, Remzi FH, Wexner SD, Winchester DP, Monson JRT, Lee L, Dietz DW, Consortium for Optimizing the Treatment of Rectal C. Evaluating the Current Status of Rectal Cancer Care in the US: Where We Stand at the Start of the Commission on Cancer's National Accreditation Program for Rectal Cancer. J Am Coll Surg. 2018;226(5):881–90. doi:https://doi.org/10.1016/j.jamcollsurg.2018.01.057.
Schrag D, Weiser MR, Goodman KA, Gonen M, Hollywood E, Cercek A, Reidy-Lagunes DL, Gollub MJ, Shia J, Guillem JG, Temple LK, Paty PB, Saltz LB. Neoadjuvant chemotherapy without routine use of radiation therapy for patients with locally advanced rectal cancer: a pilot trial. J Clin Oncol. 2014;32(6):513–8. doi:https://doi.org/10.1200/JCO.2013.51.7904.
Weiser MR FA, Schrag D, Boughey JC, You YN. Progress in the PROSPECT trial: precision treatment for rectal cancer?. Bull Am Coll Surg. 2015;100(4):51–2.
Sauer R, Liersch T, Merkel S, Fietkau R, Hohenberger W, Hess C, Becker H, Raab HR, Villanueva MT, Witzigmann H, Wittekind C, Beissbarth T, Rodel C. Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. J Clin Oncol. 2012;30(16):1926–33. doi:https://doi.org/10.1200/JCO.2011.40.1836.
Lai L, Fuller, CD, Kachnic, LA, Thomas, CR Jr,. Can pelvic radiotherapy be omitted in select patients with rectal cancer?. Semin Oncol. 2006;66(6 Suppl 11):S70–4.
Gunderson LL, Sargent DJ, Tepper JE, Wolmark N, O’Connell MJ, Begovic M, Allmer C, Colangelo L, Smalley SR, Haller DG, Martenson JA, Mayer RJ, Rich TA, Ajani JA, MacDonald JS, Willett CG, Goldberg RM. Impact of T and N stage and treatment on survival and relapse in adjuvant rectal cancer: a pooled analysis. J Clin Oncol. 2004;22(10):1785–96. doi:https://doi.org/10.1200/JCO.2004.08.173.
Tepper J, O'Connell, M, Niedzwiecki, D, Hollis, DR, Benson, AB 3rd, Cummings, B, Gunderson, LL, Macdonald, JS, Martenson, JA, Mayer, RJ. Adjuvant therapy in rectal cancer: analysis of stage, sex, and local control--final report of intergroup 0114. J Clin Oncol. . 2002;20(7):1744–50.
Schisterman EF, Cole SR, Platt RW. Over adjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology. 2009;20(4 ):488–95.
Deyo RA CD, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. Clin Epidemiol. 1992;45:613–9.
Rickles AS, Dietz DW, Chang GJ, Wexner SD, Berho ME, Remzi FH, Greene FL, Fleshman JW, Abbas MA, Peters W, Noyes K, Monson JR, Fleming FJ, Consortium for Optimizing the Treatment of Rectal C. High Rate of Positive Circumferential Resection Margins Following Rectal Cancer Surgery: A Call to Action. Ann Surg. 2015;262(6):891–8. doi:https://doi.org/10.1097/SLA.0000000000001391.
Zhang J, Yu KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1.
Knol MJ, LeCessie S, Algra A, Vandenbroucke JP, Groenwold RH. Overestimation of risk ratios by odds ratios in trials and cohort studies: alternatives to logistic regression. CMAJ. 2012;184(8):895–6.
Muller CJ, MacLehose RF. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int J Epidemiol. 2014;43(3):962–70.
Norton EC, Miller MM, Kleinman LC. Computing adjusted risk ratios and risk differences in Stata. Stata J. 2013;13(3):492–509.
Dimick JB WH, Birkmeyer JD. Surgical mortality as an indicator of hospital quality: the problem with small sample size. JAMA. 2004;292(7):847–51.
Dimick J, Staiger, DO, Birkmeyer, JD.,. Ranking hospitals on surgical mortality: the importance of reliability adjustment. Health Serv Res. 2010;45(6):1614–29.
Dimick JB, Ghaferi AA, Osborne NH, Ko CY, Hall BL. Reliability adjustment for reporting hospital outcomes with surgery. Ann Surg. 2012;255(4):703–7. doi:https://doi.org/10.1097/SLA.0b013e31824b46ff.
Bland J M, Altman D G. Correlation, regression, and repeated data. BMJ 1994;308(896).
Bland J M, Altman D G. Calculating correlation coefficients with repeated observations: Part 2—Correlation between subjects. BMJ. 1995;310(633).
Charlton ME, Lin C, Jiang D, Stitzenberg KB, Halfdanarson TR, Pendergast JF, Chrischilles EA, Wallace RB. Factors associated with use of preoperative chemoradiation therapy for rectal cancer in the Cancer Care Outcomes Research and Surveillance Consortium. Am J Clin Oncol. 2013;36(6):572–9. doi:https://doi.org/10.1097/COC.0b013e318261082b.
Charlton M, Hrabe, JE, Wright, KB, Schlichting, JA, McDowell, BD, Halfdanarson, TR, Lin, C, Stitzenberg, KB, Cromwell, JW. Hospital Characteristics Associated with Stage II/III Rectal Cancer Guideline Concordant Care: Analysis of Surveillance, Epidemiology and End Results-Medicare Data. J Gastrointest Surg. 2016;20(5):1002–11.
Charlton ME, Mattingly-Wells LR, Marcet JE, McMahon Waldschmidt BC, Cromwell JW. Association between surgeon characteristics and their preferences for guideline-concordant staging and treatment for rectal cancer. Am J Surg. 2014;208(5):817–23. doi:https://doi.org/10.1016/j.amjsurg.2014.03.010.
Chang JS, Lee Y, Lim JS, Kim NK, Baik SH, Min BS, Huh H, Koom WS. The magnetic resonance imaging-based approach for identification of high-risk patients with upper rectal cancer. Ann Surg. 2014;260(2):293–8. doi:https://doi.org/10.1097/SLA.0000000000000503.
Marinello F, Frasson, M, Baguena, G, Flor-Lorente, B, Cervantes, A, Roselló, S, Espí, A, García-Granero, E,. Selective approach for upper rectal cancer treatment: total mesorectal excision and preoperative chemoradiation are seldom necessary. Dis Colon Rectum. 2015;58(6):556–65.
Battersby NJ, How P, Moran B, Stelzner S, West NP, Branagan G, Strassburg J, Quirke P, Tekkis P, Pedersen BG, Gudgeon M, Heald B, Brown G, Group MIS. Prospective Validation of a Low Rectal Cancer Magnetic Resonance Imaging Staging System and Development of a Local Recurrence Risk Stratification Model: The MERCURY II Study. Ann Surg. 2016;263(4):751–60. doi:https://doi.org/10.1097/SLA.0000000000001193.
Author information
Authors and Affiliations
Contributions
Study conception and design: Swords, Skarda, Sause, Kim
Acquisition and analysis of data: Swords, Gygi
Interpretation of data: Swords, Skarda, Sause, Gawlick, Cannon, Lewis, Scaife, Gygi, Kim
Drafting of manuscript: Swords
Critical revision of manuscript: Swords, Skarda, Sause, Gawlick, Cannon, Lewis, Scaife, Gygi, Kim
Final approval of submission: Swords, Skarda, Sause, Gawlick, Cannon, Lewis, Scaife, Gygi, Kim
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Swords, D.S., Skarda, D.E., Sause, W.T. et al. Surgeon-Level Variation in Utilization of Local Staging and Neoadjuvant Therapy for Stage II-III Rectal Adenocarcinoma. J Gastrointest Surg 23, 659–669 (2019). https://doi.org/10.1007/s11605-019-04107-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04107-1