Abstract
Background
Passage of flatus after abdominal surgery signals resolution of physiological postoperative ileus (POI) and often, particularly after complex open surgeries, serves as the trigger to initiate oral feeding. To date, there is no objective tool that can predict time to flatus allowing for timely feeding and optimizing recovery. In an open, prospective study, we examine the use of a noninvasive wireless patch system that measures electrical activity from gastrointestinal smooth muscles in predicting time to first flatus.
Methods
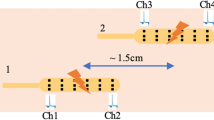
Eighteen patients who underwent open abdominal surgery at El Camino Hospital, Mountain View, CA, were consented and studied. Immediately following surgery, wireless patches were placed on the patients’ anterior abdomen. Colonic frequency peaks in the spectra were identified in select time intervals and the area under the curve of each peak times its duration was summed to calculate cumulative myoelectrical activity.
Results
Patients with early flatus had stronger early colonic activity than patients with late flatus. At 36 h post-surgery, a linear fit of time to flatus vs cumulative colonic myoelectrical activity predicted first flatus as much as 5 days (± 22 h) before occurrence.
Conclusions
In this open, prospective pilot study, noninvasive measurement of colon activity after open abdominal surgery was feasible and predictive of time to first flatus. Interventions such as feeding can potentially be optimized based on this prediction, potentially improving outcomes, decreasing length of stay, and lowering costs.






Similar content being viewed by others
References
Luckey A, Livingston E, Taché Y. Mechanisms and treatment of postoperative ileus. Arch Surg. 2003;138:206–14.
Mattei P, Rombeau JL. Review of the pathophysiology and management of postoperative ileus. World J Surg. 2006;30:1382–91.
Kehlet H, Holte K. Review of postoperative ileus. Am J Surg. 2001;182:3S–10S.
Ahmed J, Mehmood S, MacFie J. Postoperative Ileus in Elective Colorectal Surgery: Management Strategies. Contemp Issues Color Surg Pract. 2012. p. 35–54.
Goldstein JL, Matuszewski K A, Delaney CP, Senagore A, Chiao EF, Shah M, et al. Inpatient Economic Burden of Postoperative Ileus Associated with Abdominal Surgery in the United States. P&T. 2007;32:82–90.
Iyer S, Saunders WB, Stemkowski S. Economic burden of postoperative ileus associated with colectomy in the United States. J Manag Care Pharm. 2009;15:485–94.
Flynn DN, Speck RM, Mahmoud NN, David G, Fleisher LA. The impact of complications following open colectomy on hospital finances: a retrospective cohort study. Perioper Med. 2014;3:1.
Van Bree SHW, Bemelman WA, Hollmann MW, Zwinderman AH, Matteoli G, El Temna S, et al. Identification of clinical outcome measures for recovery of gastrointestinal motility in postoperative ileus. Ann Surg. 2014;259:708–14.
Grass F, Slieker J, Jurt J, Kummer A, Solà J, Hahnloser D, et al. Postoperative ileus in an enhanced recovery pathway—a retrospective cohort study. Int J Colorectal Dis. 2017;32:675–81.
Read TE, Brozovich M, Andujar JE, Ricciardi R, Caushaj PF. Bowel Sounds Are Not Associated with Flatus, Bowel Movement, or Tolerance of Oral Intake in Patients after Major Abdominal Surgery. Dis Colon Rectum. 2017;60:608–13.
Waldhausen JH, Shaffrey ME, Skenderis BS, Jones RS, Schirmer BD. Gastrointestinal myoelectric and clinical patterns of recovery after laparotomy. Ann Surg. 1990;211:777–84.
Massey RL. Return of bowel sounds indicating an end of postoperative ileus: is it time to cease this long-standing nursing tradition? Medsurg Nurs. 2012;21:146–50.
Sarna SK. Physiology and pathophysiology of colonic motor activity. Dig Dis Sci. 1991;36:827–62.
Condon, R E, Cowles, Verne, Schulte, William J, Frantzides, Constantinos, Matsumoto T. The effect of whole gut lavage on colon motility and gastrocolic response in the subhuman primate. Surgery. 1986;99:531–6.
Sarna SK. Myoelectric correlates of colonic motor complexes and contractile activity. Am J Physiol. 1986;250:G213–20.
Sarna SK, Waterfall WE, Bardakjian BL. Types of human colonic electrical activities recorded postoperatively. Gastroenterology. 1981;81:61–70.
Condon RE, Frantzides CT, Cowles VE, Mahoney JL, Schulte WJ, Sarna SK. Resolution of postoperative ileus in humans. Ann Surg. 1986;203:574–81.
Condon RE, Cowles VE, Ferraz AA, Carilli S, Carlson ME, Ludwig K, et al. Human colonic smooth muscle electrical activity during and after recovery from postoperative ileus. Am J Physiol. 1995;269:G408–17.
Axelrod S, Navalgund AR, Axelrod LA, Triadafilopoulos G. Mo1591 - A New Motility Tool: High Concordance Between Internal Smartpill Pressure Recordings and Myoelectric Events Measured by External Wireless G-Tech Patches. Gastroenterology [Internet]. Elsevier; 2018;154:S-763. Available from: https://doi.org/10.1016/S0016-5085(18)32642-8
Delaney CP, Kiran RP, Senagore AJ, Brady K, Fazio VW. Case-Matched Comparison of Clinical and Financial Outcome after Laparoscopic or Open Colorectal Surgery. Ann Surg. 2003;238:67–72.
Shapiro SB, Bray MS, Appel AL, Kallies KJ, Borgert AJ, Zinnel BA. Implementation of an Enhanced Recovery After Surgery Program for Colorectal Surgery at a Community Teaching Hospital. Wmj. 2017;22–7.
Frantzides, C T, Cowles, Verne, Salaymeh, Basil, Tekin, Ercument Condon, Robert. Morphine effects on human colonic myoelectrical activity in the postoperative period. Am J Surg. 1992;163:144–9.
Wolff BG, Michelassi F, Gerkin TM, Techner L, Gabriel K, Du W, et al. Alvimopan, a novel, peripherally acting μ opioid antagonist: Results of a multicenter, randomized, double-blind, placebo-controlled, phase III trial of major abdominal surgery and postoperative ileus. Ann Surg. 2004;240:728–35.
Drake TM, Ward AE. Pharmacological management to prevent ileus in major abdominal surgery: a systematic review and meta-analysis. J. Gastrointest. Surg. 2016. p. 1253–64.
Taylor I, Duthie HL, Smallwood RH, Linkens D. Large bowel myoelectrical activity in man. Gut. 1975;16:808–14.
Dinning PG, Szczesniak MM, Cook IJ. Twenty-four hour spatiotemporal mapping of colonic propagating sequences provides pathophysiological insight into constipation. Neurogastroenterol Motil. 2008;20:1017–21.
Smith TK, Park KJ, Hennig GW. Colonic migrating motor complexes, high amplitude propagating contractions, neural reflexes and the importance of neuronal and mucosal serotonin. J Neurogastroenterol Motil. 2014;20:423–46.
Sarna SK. Colonic motility: from bench side to bedside. Colloquium Series on Integrated Systems Physiology: From Molecule to Function. Morgan & Claypool Life Sciences.; 2010.
Stoddard CJ, Duthie HL, Smallwood RH, Linkens DA. Colonic myoelectrical activity in man: Comparison of recording techniques and methods of analysis. Gut. 1979;20:476–83.
Bharucha AE. High amplitude propogated contractions. Neurogastroenterol Motil. 2012;24:977–82.
Huizinga JD, Stern HS, Chow E, Diamant NE, El-Sharkawy TY. Electrophysiologic control of motility in the human colon. Gastroenterology. 1985;88:500–11.
Christensen J, Schedl HP, Clifton JA. The small intestinal basic electrical rhythm (slow wave) frequency gradient in normal men and in patients with a variety of diseases. Gastroenterology. The Williams & Wilkins Company; 1966;50:309–15.
Chang F, Lu C, Chen C, Luo J, Lee S, Wu H CJ. Fasting and postprandial small intestinal slow waves non-invasively measured in subjects with total gastrectomy. J Gastroenterol Hepatol. 2007;22:247–52.
Chen, Jian De, Schinner, D, McCallum RW. Measurement of small Intestine slow wave electrical activity with surface electrodes. IEEE Trans Biomed Eng. 1993;40.
Yin J, Chen JDZ. Electrogastrography: Methodology, validation and applications. J Neurogastroenterol Motil. 2013;19:5–17.
Acknowledgements
We would like to thank Ryan Schroeder, Director of Clinical Research, and his team at the El Camino Hospital, Mountain View, CA, for their help in recruiting and consenting patients for the study.
Grant Support
Work supported in part by a grant from the Kenneth Rainin Foundation. This work also received support from the Fogarty Institute for Innovation and Breakout Labs.
Author information
Authors and Affiliations
Contributions
Study design: AN, SA, SS, GT
Acquisition of data: AN, SA, LA, SS, KT, PL
Analysis and interpretation: AN, SA, LA, SS, KT, PL, GT
Manuscript draft: AN, SA, KT, GT
Critical review and revision: AN, SA, SS, KT, GT
Corresponding author
Ethics declarations
Conflict of interest
Authors SA, LA, and AN are employees of G-Tech Medical. Author GT is an advisor to G-Tech Medical. Patches for this study were supplied by G-Tech Medical.
Additional information
Poster presentation
The work was presented as a poster at the 2018 Digestive Disease Week (DDW) held in Washington D.C, June 2018.
Rights and permissions
About this article
Cite this article
Navalgund, A., Axelrod, S., Axelrod, L. et al. Colon Myoelectric Activity Measured After Open Abdominal Surgery with a Noninvasive Wireless Patch System Predicts Time to First Flatus. J Gastrointest Surg 23, 982–989 (2019). https://doi.org/10.1007/s11605-018-4030-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-4030-4