Abstract
Background
Hepatocellular carcinoma (HCC) is one of the fastest growing causes of cancer-related death in the USA. Studies that investigated the impact of HCC therapeutic delays are limited to single centers, and no large-scale database research has been conducted. This study investigated the association of surgical delay and survival in HCC patients.
Methods
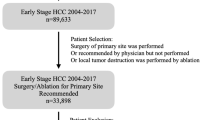
Patients underwent local tumor destruction and hepatic resection for stages I–III HCC were identified from the 2004 to 2013 Commission on Cancer’s National Cancer Database. Surgical delay was defined as > 60 days from the date of diagnosis to surgery. Generalized linear-mixed model assessed the demographic and clinical factors associated with delay, and frailty Cox proportional hazard analysis examined the prognostic factors for overall survival.
Results
A total of 12,102 HCC patients met the eligibility criteria. Median wait time to surgery was 50 days (interquartile range, 29–86), and 4987 patients (41.2%) had surgical delay. Delayed patients demonstrated better 5-year survival for local tumor destruction (29.1 vs. 27.6%; P = .001) and resection (44.1 vs. 41.0%; P = .007). Risk-adjusted model indicated that delayed patients had a 7% decreased risk of death (HR, 0.93; 95% CI, 0.87–0.99; P = .027). Similar findings were also observed using other wait time cutoffs at 50, 70, 80, 90, and 100 days.
Conclusions
A plausible explanation of this finding may be case prioritization, in which patients with more severe and advanced disease who were at higher risk of death received earlier surgery, while patients with less-aggressive tumors were operated on later and received more comprehensive preoperative evaluation.




Similar content being viewed by others
References
Islami F, Miller KD, Siegel RL, Fedewa SA, Ward EM, Jemal A. Disparities in liver cancer occurrence in the United States by race/ethnicity and state. CA Cancer J Clin. 2017;67(4):273–289.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017;67:7–30.
U.S. Cancer Statistics Working Group. United States Cancer Statistics: 1999–2014 Incidence and Mortality Web-based Report. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute. 2017. Available at: www.cdc.gov/uscs. Accessed 22 December 2017.
Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology, 2011;53(3):1020–1022.
McCormack L, Dutkowski P, El-Badry AM, Clavien PA. Liver transplantation using fatty livers: always feasible? J Hepatol. 2011;54(5):1055–1062.
Bhardwaj N, Perera MTPR, Silva MA. Current treatment approaches to HCC with a special consideration to transplantation. J Transplant. 2016;2016:7926264.
Giannini EG, Farinati F, Ciccarese F, Pecorelli A, Rapaccini GL, Di Marco M, Benvegnu L, Caturelli E, Zoli M, Borzio F, Chiaramonte M, Trevisani F, Italian Liver Cancer (ITA.LI.CA) Group Prognosis of untreated hepatocellular carcinoma. Hepatology. 2015;61(1):184–190.
Singal AG, Tiro JA, Gupta S. Improving hepatocellular carcinoma screening: applying lessons from colorectal cancer screening. Clin Gastroenterol Hepatol. 2013;11(5):472–477.
Singal AG, Waljee AK, Patel N, Chen EY, Tiro JA, Marrero JA, Yopp AC. Therapeutic delays lead to worse survival among patients with hepatocellular carcinoma. J Natl Compr Canc Netw. 2013;11(9):1101–1108.
Neal RD, Tharmanathan P, France B, Din NU, Cotton S, Fallon-Ferguson J, Hamilton W, Hendry A, Hendry M, Lewis R, Macleod U, Mitchell ED, Pickett M, Rai T, Shaw K, Stuart N, Tørring ML, Wilkinson C, Williams B, Williams N, Emery J. Is increased time to diagnosis and treatment in symptomatic cancer associated with poorer outcomes? Systematic review. Br J Cancer. 2015;112 Suppl 1:S92-S107.
Huo TI, Huang YH, Chiang JH, Wu JC, Lee PC, Chi CW, Lee SD. Survival impact of delayed treatment in patients with hepatocellular carcinoma undergoing locoregional therapy: is there a lead-time bias? Scan J Gastroenterol. 2007;42(4):485–492.
Chen WT, Fernandes ML, Lin CC, Lin SM. Delay in treatment of early-stage hepatocellular carcinoma using radiofrequency ablation may impact survival of cirrhotic patients in a surveillance program. J Surg Oncol. 2011;103(2):133–139.
Brahmania M, Ahmed O, Kelley M, Wong D, Kowgier M, Khalili K, Beercroft R, Renner EL, Shah H, Feld J, Janssen HLA, Sherman M. Wait time for curative intent radio frequency ablation is associated with increased mortality in patients with early stage hepatocellular carcinoma. Ann Hepatol. 2017;16(5):765–771.
Croome KP, Chudzinski R, Hanto DW. Increasing time delay from presentation until surgical referral for hepatobiliary malignancies. HPB (Oxford). 2010;12(9):644–648.
Lim C, Bhangui P, Salloum C, Gomez-Gavara C, Lahat E, Luciani A, Compagnon P, Calderaro J, Feray C, Azoulay D. Impact of time to surgery in the outcome of patients with liver resection for BCLC 0-A hepatocellular carcinoma. J Hepatol. 2017.
Akce M, Sansgiry S, Temple SL, Davila J, Sada Y. The effect of treatment delay on survival in patients with hepatocellular cancer. J Clin Oncol. 2017;35:15_Suppl.e15645.
Boffa DJ, Rosen JE, Mallin K, Loomis A, Gay G, Palis B, Thoburn K, Gress D, McKellar DP, Shulman LN, Facktor MA, Winchester DP. Using the National Cancer Database for outcomes research: a review. JAMA Oncol. 2017;3(12):1722–1728.
Chidi AP, Bryce CL, Han K, Dong ZM, Geller DA, Tsung A. Predictors of delay of surgical intervention in patients with hepatocellular carcinoma. J Surg Res. 2014;186:610–611.
Myrdal G, Lambe M, Hillerdal G, Lamberg K, Agustsson T, Stahle E. Effect of delays on prognosis in patients with non-small cell lung cancer. Thorax. 2004;59(1):45–49.
Diaconescu R, Lafond C, Whittom R. Treatment delays in non-small cell lung cancer and their prognostic implications. J Thorac Oncol. 2011;6(7):1254–1259.
González-Barcala FJ, García-Prim JM, Álvarez-Dobaño JM, Moldes-Rodriguez M, Garcia-Sanz MT, Pose-Reino A, Valdes-Cuadrado L. Effects of delays on survival in patients with lung cancer. Clin Transl Oncol. 2010(12);12:836.
Amri R, Bordeianou LG, Sylla P, Berger DL. Treatment delay in surgically-treated colon cancer: does it affect outcomes? Ann Surg Oncol. 2014;21(12):3909–3016.
Crawford SC, Davis JA, Siddiqui NA, de Caestecker L, Gills CR, Hole D, Penney G. The wait time paradox: population based retrospective study of treatment delay and survival of women with endometrial cancer in Scotland. BMJ. 2002;325(7357):196.
Wallace DM, Bryan RT, Dunn JA, Begum G, Bathers S, West Midlands Urological Research Group Delay and survival in bladder cancer. BJU Int. 2002;89(9):868–878.
Hoehn RS, Hanseman DJ, Jernigan PL, Wima K, Ertel AE, Abbott DE, Shah SA. Disparities in care for patients with curable hepatocellular carcinoma. HPB (Oxford). 2015;17(9):747–752.
Bilimoria KY, Ko CY, Tomlinson JS, Stewart AK, Talamonti MS, Hynes DL, Winchester DP, Bentrem DJ. Wait times for cancer surgery in the United States: trends and predictors of delays. Ann Surg. 2011;253(4):779–785.
Jindal M, Zheng C, Quadri HS, Ihemelandu CU, Hong YK, Smith AK, Dudeja V, Shara NM, Johnson LB, Al-Refaie WB. Why do long-distance travelers have improved pancreatectomy outcomes? J Am Coll Surg. 2017;225(2):216–225.
Haddad AQ, Hutchinson R, Wood EL, Miranda G, Gershman B, Messer J, Svatek R, Black PC, Boorjian SA, Shah J, Daneshmand S, Lotan Y. Association of distance to treatment facility with survival and quality outcomes after radical cystectomy: a multi-institutional study. Clin Genitourin Cancer. 2017;15(6):689–695.e2.
Funding Source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
KX contributed to the study design, conceptualization, statistical analysis, and drafted the original paper. KMMI was responsible for data acquisition. SWG and FR also contributed to the study design and conceptualization, and JL assisted with statistical analysis. FR, PF, HW, and KMMI critically reviewed and edited the paper for important intellectual content. SWG supervised research activities.
Corresponding author
Ethics declarations
The data used in the study are derived from a de-identified NCDB file. The American College of Surgeons and the Commission on Cancer have not verified and are not responsible for the analytic or statistical methodology employed, or the conclusions drawn from these data by the investigator.
Ethics Committee Approval
The study was exempted from review by the University of Nebraska Medical Center Institutional Review Board.
Conflict of Interest
The authors declare that they have no conflict of interest.
Electronic Supplementary Material
ESM 1
(DOCX 45 kb)
Rights and permissions
About this article
Cite this article
Xu, K., Watanabe-Galloway, S., Rochling, F.A. et al. Surgical Delay Is Associated with Improved Survival in Hepatocellular Carcinoma: Results of the National Cancer Database. J Gastrointest Surg 23, 933–943 (2019). https://doi.org/10.1007/s11605-018-3925-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-3925-4