Abstract
Purpose
Postoperative superficial surgical site infection is a major complication in hepatobiliary-pancreatic surgery. We aimed to compare the efficacy of subcuticular sutures versus staples for skin closure in preventing superficial surgical site infection in hepatobiliary-pancreatic surgery.
Methods
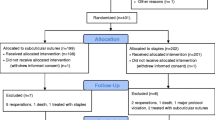
Consecutive patients who underwent hepatobiliary-pancreatic surgery at our hospital from October 2006 to March 2011 and from April 2012 to March 2015 were reviewed retrospectively. Superficial surgical site infection incidence was evaluated in patients who received subcuticular sutures and those who received staples for skin closure. Propensity score matching analysis was used to adjust bias from confounding factors.
Results
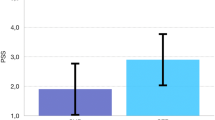
A total of 691 patients were included. Patients with skin staple closures (n = 346) were compared with patients with subcuticular suture closures (n = 345). After a propensity score matching analysis, a significant difference in superficial surgical site infection incidence was found between the skin stapler group (11.3%) and subcuticular sutures group (2.6%). The same comparison was performed by a subgroup analysis and supported this finding in patients after hepatectomy without biliary reconstruction, pancreatoduodenectomy, or open laparotomy surgeries and in patients with body mass index < 25.
Conclusions
Subcuticular suturing after hepatobiliary-pancreatic surgery was more efficacious in reducing postoperative superficial surgical site infection incidence than staples for skin closure.

Similar content being viewed by others
References
Leaper DJ. Risk factors for and epidemiology of surgical site infections. Surg Infect (Larchmt) 2010;11:283–287.
Broex EC, van Asselt AD, Bruggeman CA, van Tiel FH. Surgical site infections: how high are the costs? J Hosp Infect 2009;72:193–201.
Lee I, Agarwal RK, Lee BY, Fishman NO, Umscheid CA. Systematic review and cost analysis comparing use of chlorhexidine with use of iodine for preoperative skin antisepsis to prevent surgical site infection. Infect Control Hosp Epidemiol 2010;31:1219–1229.
Artinyan A, Orcutt ST, Anaya DA, Richardson P, Chen GJ, Berger DH. Infectious postoperative complications decrease long-term survival in patients undergoing curative surgery for colorectal cancer: a study of 12,075 patients. Ann Surg 2015;261:497–505.
Dimick JB, Chen SL, Taheri PA, Henderson WG, Khuri SF, Campbell DA Jr. Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg 2004;199:531–537.
Merkow RP, Ju MH, Chung JW, Hall BL, Cohen ME, Williams MV, Tsai TC, Ko CY, Bilimoria KY. Underlying reasons associated with hospital readmission following surgery in the United States. JAMA. 2015;313:483–495.
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 1999;20:250–278.
Mu Y, Edwards JR, Horan TC, Berrios-Torres SI, Fridkin SK. Improving risk-adjusted measures of surgical site infection for the national healthcare safety network. Infect Control Hosp Epidemiol 2011;32:970–986.
Edwards JR, Peterson KD, Mu Y, Banerjee S, Allen-Bridson K, Morrell G, Dudeck MA, Pollock DA, Horan TC. National Healthcare Safety Network (NHSN) report: data summary for 2006 through 2008, issued December 2009. Am J Infect Control 2009;37:783–805.
Japan Society for Infection Prevention and Control. Japanese Healthcare Associated Infections Surveillance. SSI surveillance 2016. http://www.kankyokansen.org/uploads/uploads/files/jsipc/jhais_ssi-surveillance2016.pdf. 2017.
Nakahira S, Shimizu J, Miyamoto A, Kobayashi S, Umeshita K, Ito T, Monden M, Doki Y, Mori M. Proposal for a sub-classification of hepato-biliary-pancreatic operations for surgical site infection surveillance following assessment of results of prospective multicenter data. J Hepatobiliary Pancreat Sci 2013;20:504–511.
Yang T, Tu PA, Zhang H, Lu JH, Shen YN, Yuan SX, Lau WY, Lai ECH, Lu CD, Wu MC, Li JW, Shen F. Risk factors of surgical site infection after hepatic resection. Infect Control Hosp Epidemiol 2014;35:317–320.
Dohmen PM. Influence of skin flora and preventive measures on surgical site infection during cardiac surgery. Surg Infect (Larchmt) 2006;7:S13-S17.
Leaper D, Nazir J, Roberts C, Searle R. Economic and clinical contributions of an antimicrobial barrier dressing: a strategy for the reduction of surgical site infections. J Med Econ 2010;13:447–452.
Jarral OA, McCormack DJ, Ibrahim S, Shipolini AR. Should surgeons scrub with chlorhexidine or iodine prior to surgery? Interact Cardiovasc Thorac Surg 2011;12:1017–1021.
Nikfarjam M, Weinberg L, Fink MA, Muralidharan V, Starkey G, Jones R, Staveley-O’Carroll K, Christophi C. Pressurized pulse irrigation with saline reduces surgical-site infections following major hepatobiliary and pancreatic surgery: randomized controlled trial. World J Surg 2014;38:447–455.
Ng WK, Awad N. Performance improvement initiative: prevention of surgical site infection (SSI). BMJ Qual Improv Rep 2015;4:u205401.w3279.
Chen M, Song X, Chen LZ, Lin ZD, Zhang XL. Comparing mechanical bowel preparation with both oral and systemic antibiotics versus mechanical bowel preparation and systemic antibiotics alone for the prevention of surgical site infection after elective colorectal surgery: a meta-analysis of randomized controlled clinical trials. Dis Colon Rectum 2016;59:70–78.
Tsujinaka T, Yamamoto K, Fujita J, Endo S, Kawada J, Nakahira S, Toshio Shimokawa T, Kobayashi S, Yamasaki M, Akamaru Y, Miyamoto A, Mizushima T, Shimizu J, Umeshita K, Ito T, Doki Y, Mori M; Clinical Study Group of Osaka University on Section of Risk Management. Subcuticular sutures versus staples for skin closure after open gastrointestinal surgery: a phase 3, multicentre, open-label, randomised controlled trial. Lancet 2013;382:1105–1112.
Morikane K. Epidemiology and risk factors associated with surgical site infection after different types of hepatobiliary and pancreatic surgery. Surg Today 2017;47:1208–1214.
Culver DH, Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG, Banerjee SN, Edwards JR, Tolson JS, Henderson TS, Hughes JM; National Nosocomial Infections Surveillance System. Surgical wound infection rates by wound class, operative procedure, and patient risk index. National Nosocomial Infections Surveillance System. Am J Med 1991;91:152S–157S.
Emori TG, Culver DH, Horan TC, Jarvis WR, White JW, Olson DR, Banerjee SN, Edwards JR, Martone WJ, Gaynes RP, Hughes JM. National nosocomial infections surveillance system (NNIS): description of surveillance methods. Am J Infect Control 1991;19:19–35.
Gaynes RP, Culver DH, Horan TC, Edwards JR, Richards C, Tolson JS. Surgical site infection (SSI) rates in the United States, 1992–1998: the National Nosocomial Infections Surveillance System basic SSI risk index. Clin Infect Dis. 2001;33:S69-S77.
Haley RW, Culver DH, Morgan WM, White JW, Emori TG, Hooton TM. Identifying patients at high risk of surgical wound infection. A simple multivariate index of patient susceptibility and wound contamination. Am J Epidemiol. 1985;121:206–215.
Tsujita E, Yamashita Y, Takeishi K, Matsuyama A, Tsutsui S, Matsuda H, Taketomi A, Shirabe K, Ishida T, Maehara Y. Subcuticular absorbable suture with subcutaneous drainage system prevents incisional SSI after hepatectomy for hepatocellular carcinoma. World J Surg 2012;36:1651–1656.
Macedo FIB, Mowzoon M, Parikh J, Sathyanarayana SA, Jacobs MJ. Disparities in the management and prophylaxis of surgical site infection and pancreatic fistula after pancreatoduodenectomy. J Hepatobiliary Pancreat Sci 2017;24:268–280.
Johnson RG, Cohn WE, Thurer RL, McCarthy JR, Sirois CA, Weintraub RM. Cutaneous closure after cardiac operations: a controlled, randomized, prospective comparison of intradermal versus staple closures. Ann Surg 1997;226:606–612.
Biancari F, Tiozzo V. Staples versus sutures for closing leg wounds after vein graft harvesting for coronary artery bypass surgery. Cochrane Database Syst Rev 2010;5:CD008057.
Shetty AA, Kumar VS, Morgan-Hough C, Georgeu GA, James KD, Nicholl JE. Comparing wound complication rates following closure of hip wounds with metallic skin staples or subcuticular vicryl suture: a prospective randomised trial. J Orthop Surg (Hong Kong) 2004;12:191–193.
Johnson A, Young D, Reilly J. Caesarean section surgical site infection surveillance. J Hosp Infect 2006;64:30–35.
Watanabe A, Kohnoe S, Shimabukuro R, Yamanaka T, Iso Y, Baba H, Higashi H, Orita H, Emi Y, Takahashi I, Korenaga D, Maehara Y. Risk factors associated with surgical site infection in upper and lower gastrointestinal surgery. Surg Today 2008;38:404–412.
Lacy AM, García-Valdecasas JC, Delgado S, Grande L, Fuster J, Tabet J, Ramos C, Piqué JM, Cifuentes A, Visa J. Postoperative complications of laparoscopic-assisted colectomy. Surg Endosc 1997;11:119–122.
Mayol J, Garcia-Aguilar J, Ortiz-Oshiro E, De-Diego Carmona JA, Fernandez-Represa JA. Risks of the minimal access approach for laparoscopic surgery: multivariate analysis of morbidity related to umbilical trocar insertion. World J Surg 1997;21:529–533.
Golub R, Siddiqui F, Pohl D. Laparoscopic versus open appendectomy: a metaanalysis. J Am Coll Surg 1998;186:545–553.
Author information
Authors and Affiliations
Contributions
KT contributed to the study concept and design, acquisition of data, statistical analysis, interpretation of data, and drafting of the manuscript. NC contributed to the study concept and design, statistical analysis, and interpretation of data. SO, KY, TG, KH, YO, MO, TS, and RT contributed to the acquisition of data. MS contributed to the interpretation of data. SK contributed to the study concept and design, and interpretation of data. All authors contributed to the critical manuscript revision.
Corresponding author
Rights and permissions
About this article
Cite this article
Tomita, K., Chiba, N., Ochiai, S. et al. Superficial Surgical Site Infection in Hepatobiliary-Pancreatic Surgery: Subcuticular Suture Versus Skin Staples. J Gastrointest Surg 22, 1385–1393 (2018). https://doi.org/10.1007/s11605-018-3754-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-3754-5