Abstract
Purpose
The aim of this study was to evaluate the advantages of ultra-high-resolution computed tomography (U-HRCT) for automatic bronchial segmentation.
Materials and methods
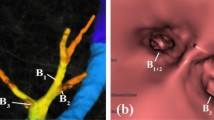
This retrospective study was approved by the Institutional Review Board, and written informed consent was waived. Thirty-three consecutive patients who underwent chest CT by a U-HRCT scanner were enrolled. In each patient, CT data were reconstructed by two different protocols: 512 × 512 matrix with 0.5-mm slice thickness (conventional HRCT mode) and 1024 × 1024 matrix with 0.25-mm slice thickness (U-HRCT mode). We used a research workstation to compare the two CT modes with regard to the numbers and total lengths of the automatically segmented bronchi.
Results
Significantly greater numbers and longer lengths of peripheral bronchi were segmented in the U-HRCT mode than in the conventional HRCT mode (P < 0.001, for fifth- to eighth-generation bronchi). For example, the mean numbers and total lengths of the sixth-generation bronchi were 81 and 1048 mm in the U-HRCT mode and 59 and 538 mm in the conventional HRCT mode.
Conclusions
The U-HRCT mode greatly improves automatic airway segmentation for the more peripheral bronchi, compared with the conventional HRCT mode. This advantage can be applied to routine clinical care, such as virtual bronchoscopy and automatic lung segmentation.


Similar content being viewed by others
References
Matsuoka S, Kurihara Y, Yagihashi K, Hoshino M, Nakajima Y. Airway dimensions at inspiratory and expiratory multisection CT in chronic obstructive pulmonary disease: correlation with airflow limitation. Radiology. 2008;248(3):1042–9.
Hasegawa M, Nasuhara Y, Onodera Y, Makita H, Nagai K, Fuke S, et al. Airflow limitation and airway dimensions in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006;173:1309–15.
Yamashiro T, Matsuoka S, San Jose Estepar R, Dransfield MT, Diaz A, Reilly JJ, et al. Quantitative assessment of bronchial wall attenuation on thin-section CT: an indicator of airflow limitation in chronic obstructive pulmonary disease. Am J Roentgenol. 2010;195(2):363–9.
Hogg JC, Macklem PT, Thurlbeck WM. Site and nature of airway obstruction in chronic obstructive lung disease. N Engl J Med. 1968;278:1355–60.
Kakinuma R, Moriyama N, Muramatsu Y, Gomi S, Suzuki M, Nagasawa H, et al. Ultra-high-resolution computed tomography of the lung: image quality of a prototype scanner. PLoS ONE. 2015;10(9):e0137165.
Yanagawa M, Hata A, Honda O, Kikuchi N, Miyata T, Uranishi A, et al. Subjective and objective comparisons of image quality between ultra-high-resolution CT and conventional area detector CT in phantoms and cadaveric human lungs. Eur Radiol. 2018;28(12):5060–8.
Hata A, Yanagawa M, Honda O, Kikuchi N, Miyata T, Tsukagoshi S, et al. Effect of matrix size on the image quality of ultra-high-resolution CT of the lung: comparison of 512 × 512, 1024 × 1024, and 2048 × 2048. Acad Radiol. 2018;25(7):869–76.
Honda O, Yanagawa M, Hata A, Kikuchi N, Miyata T, Tsukagoshi S, et al. Influence of gantry rotation time and scan mode on image quality in ultra-high-resolution CT system. Eur J Radiol. 2018;103(1):71–5.
Yoshioka K, Tanaka R, Takagi H, Ueyama Y, Kikuchi K, Chiba T, et al. Ultra-high-resolution CT angiography of the artery of Adamkiewicz: a feasibility study. Neuroradiology. 2018;60(1):109–15.
Takagi H, Tanaka R, Nagata K, Ninomiya R, Arakita K, Schuijf JD, et al. Diagnostic performance of coronary CT angiography with ultra-high-resolution CT: comparison with invasive coronary angiography. Eur J Radiol. 2018;101:30–7.
Tanaka R, Yoshioka K, Takagi H, Schuijf JD, Arakita K. Novel developments in non-invasive imaging of peripheral arterial disease with CT: experience with state-of-the-art, ultra-high-resolution CT and subtraction imaging. Clin Radiol. 2019;74(1):51–8.
Nagata H, Murayama K, Suzuki S, Watanabe A, Hayakawa M, Saito Y, et al. Initial clinical experience of a prototype ultra-high-resolution CT for assessment of small intracranial arteries. Jpn J Radiol. 2019;37(4):283–91.
Xu Y, Yamashiro T, Moriya H, Muramatsu S, Murayama S. Quantitative emphysema measurement on ultra-high-resolution CT scans. Int J Chron Obstruct Pulmon Dis. 2019;14(1):2283–90.
Tanabe N, Oguma T, Sato S, Kubo T, Kozawa S, Shima H, et al. Quantitative measurement of airway dimensions using ultra-high resolution computed tomography. Respir Investig. 2018;56(6):489–96.
Tanabe N, Shima H, Sato S, Oguma T, Kubo T, Kozawa S, et al. Direct evaluation of peripheral airways using ultra-high-resolution CT in chronic obstructive pulmonary disease. Eur J Radiol. 2019;120:108687.
Matsunaga Y, Chida K, Kondo Y, Kobayashi K, Kobayashi M, Minami K, et al. Diagnostic reference levels and achievable doses for common computed tomography examinations: results from the Japanese nationwide dose survey. Br J Radiol. 2019;92(1094):20180290.
Higham A, Quinn AM, Cançado JED, Singh D. The pathology of small airways disease in COPD: historical aspects and future directions. Respir Res. 2019;20(1):49.
James AL, Wenzel S. Clinical relevance of airway remodelling in airway diseases. Eur Respir J. 2007;30(1):134–55.
Washko GR, Dransfield MT, Estépar RS, Diaz A, Matsuoka S, Yamashiro T, et al. Airway wall attenuation: a biomarker of airway disease in subjects with COPD. J Appl Physiol. 2009;107(1):185–91.
Horton KM, Horton MR, Fishman EK. Advanced visualization of airways with 64-MDCT: 3D mapping and virtual bronchoscopy. AJR Am J Roentgenol. 2007;189(6):1387–96.
Higgins WE, Ramaswamy K, Swift RD, McLennan G, Hoffman EA. Virtual bronchoscopy for three-dimensional pulmonary image assessment: state of the art and future needs. Radiographics. 1998;18(3):761–78.
Vining DJ, Liu K, Choplin RH, Haponik EF. Virtual bronchoscopy. Relationships of virtual reality endobronchial simulations to actual bronchoscopic findings. Chest. 1996;109:549–53.
Asano F, Eberhardt R, Herth FJ. Virtual bronchoscopic navigation for peripheral pulmonary lesions. Respiration. 2014;88(5):430–40.
Lee HY, Lee KS. Ground-glass opacity nodules: histopathology, imaging evaluation, and clinical implications. J Thorac Imaging. 2011;26(2):106–18.
Oda S, Awai K, Liu D, Nakaura T, Yanaga Y, Nomori H, et al. Ground-glass opacities on thin-section helical CT: differentiation between bronchioloalveolar carcinoma and atypical adenomatous hyperplasia. Am J Roentgenol. 2008;190(5):1363–8.
Acknowledgements
The authors thank the engineers and technologists of Ziosoft for their excellent help in developing the research software.
Funding
University of the Ryukyus receives a research grant from Canon Medical Systems and Ziosoft.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Morita, Y., Yamashiro, T., Tsuchiya, N. et al. Automatic bronchial segmentation on ultra-HRCT scans: advantage of the 1024-matrix size with 0.25-mm slice thickness reconstruction. Jpn J Radiol 38, 953–959 (2020). https://doi.org/10.1007/s11604-020-01000-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-020-01000-9