Abstract
The involvement of the cervical spine in musculoskeletal diseases can be crucial in terms of prognosis and morbidity. Early diagnosis of possible involvement of the craniocervical junction is essential to avoid the onset of neurological complications with poor prognosis. Among inflammatory diseases, rheumatoid arthritis affects the cervical spine frequently (in about 25% of patients). Atlantoaxial inflammatory changes are also detectable in spondyloarthritis. The involvement of the cervical spine in diffuse idiopathic skeletal hyperostosis is recognized as the cause of various clinical manifestations that may involve the pharynx, larynx and esophagus. The cervical spine may be specifically frequently implicated in crystal-associated arthropathies. Spinal cord infections are infrequent diseases that account for 3–4% of all spine infections. This pictorial review attempts to provide insights to interpret the radiological appearances of the craniocervical junction on conventional radiography, computed tomography and magnetic resonance imaging in relation to various musculoskeletal disease processes.









Similar content being viewed by others
References
Carotti M, Salaffi F, Di Carlo M, Sessa F, Giovagnoni A (2019) Magnetic resonance imaging of the craniovertebral junction in early rheumatoid arthritis. Skeletal Radiol 48(4):553–561
Zoli A, Priolo F, Galossi A et al (2000) Craniocervical junction involvnt in rheumatoid arthritis: a clinical and radiological study. J Rheumatol 27:1178–1182
Bundschuh C, Modic MT, Kearney F et al (1988) Rheumatoid arthritis of the cervical spine: surface-coil MR imaging. AJR Am J Roentgenol 151:181–187
Salaffi F, Di Carlo M, Vojinovic J et al (2018) Validity of the rheumatoid arthritis impact of disease (RAID) score and definition of cut-off points for disease activity states in a population-based European cohort of patients with rheumatoid arthritis. Joint Bone Spine 85(3):317–322
Aggarwal A, Kulshreshtha A, Chaturvedi V, Misra R (1996) Cervical spine involvement in rheumatoid arthritis: prevalence and relationship with overall disease severity. J Assoc Phys India 44(7):468–471
Zikou AK, Alamanos Y, Argyropoulou MI et al (2005) Radiological cervical spine involvement in patients with rheumatoid arthritis: a cross sectional study. J Rheumatol 32(5):801–806
Joaquim AF, Appenzeller S (2014) Cervical spine involvement in rheumatoid arthritis—a systematic review. Autoimmun Rev 13:1195–1202
Bogduk N, Major GA, Carter J (1984) Lateral subluxation of the atlas in rheumatoid arthritis: a case report and post-mortem study. Ann Rheum Dis 43:341–346
Nguyen HV, Ludwig SC, Silber J et al (2004) Rheumatoid arthritis of the cervical spine. Spine J 4:329–334
Reiter MF, Oden SD (1998) Inflammatory disorders of the cervical spine. Spine 23:2755–2766
Scott DL, Coulton BL, Propert AJ (1986) Long term progression of joint damage in rheumatoid arthritis. Ann Rheum Dis 45:373–378
Jansen LMA, van der Horst-Bruinsma E, van Schaardenburg D, Bezemer PD, Dijkamns BAC (2001) Predictors of radiographic joint damage in patients with early rheumatoid arthritis. Ann Rheum Dis 60:924–927
Pellici PM, Ranawat CS, Tsairis P, Bryan WJ (1981) A prospective study of the progression of rheumatoid arthritis of the cervical spine. J Bone Joint Surg Am 63:342–350
Fujiwara K, Owaki H, Fujimoto M, Yonenobu K, Ochi T (2000) A long-term follow-up study of cervical lesions in rheumatoid arthritis. J Spinal Disord 13:519–526
Sunahara N, Matsunaga S, Mori T, Ijiri K, Sakou T (1997) Clinical course of conservatively managed rheumatoid arthritis patients with myelopathy. Spine 22:2603–2607
Casey AT, Crockard HA, Stevens J (1997) Vertical translocation. Part II. Outcomes after surgical treatment of rheumatoid cervical myelopathy. J Neurosurg 87:863–869
Reichel H, Liebhaber A, Babinsky K, Keysser G (2002) Radiological changes in the cervical spine in rheumatoid arthritis—prognostic factors obtained by a cross-sectional study. Z Rheumatol 61(6):710–717
Neva MH, Isomaki P, Hannonen P, Kauppi M, Krishnan E, Sokka T (2003) Early and extensive erosiveness in peripheral joints predicts atlantoaxial subluxations in patients with rheumatoid arthritis. Arthritis Rheum 48:1808–1813
Paimela L, Laasonen L, Kankaanpaa E, Leirisalo-Repo M (1997) Progression of cervical spine changes in patients with early rheumatoid arthritis. J Rheumatol 24:1280–1284
Reichel H, Liebhaber A, Babinsky K, Keysser G (2002) Radiological changes in the cervical spine in rheumatoid arthritis—prognostic factors obtained by a cross-sectional study. Z Rheumatol 61:710–717
Scott DL, Pugner K, Kaarela K et al (2000) The links between joint damage and disability in rheumatoid arthritis. Rheumatology (Oxford) 39(2):122–132
Lindqvist E, Saxne T, Geborek P, Eberhardt K (2002) Ten year outcome in a cohort of patients with early rheumatoid arthritis: health status, disease process, and damage. Ann Rheum Dis 61(12):1055–1059
Ahn JK, Hwang JW, Oh JM et al (2011) Risk factors for development and progression of atlantoaxial subluxation in Korean patients with rheumatoid arthritis. Rheumatol Int 31:1363–1368
Conaghan PG, O’Connor P, McGonagle D et al (2003) Elucidation of the relationship between synovitis and bone damage: a randomized magnetic resonance imaging study of individual joints in patients with early rheumatoid arthritis. Arthritis Rheum 48:64–71
McQueen FM, Benton N, Perry D et al (2003) Bone edema scored on magnetic resonance imaging scans of the dominant carpus at presentation predicts radiographic joint damage of the hands and feet six years later in patients with rheumatoid arthritis. Arthritis Rheum 48:1814–1827
Schwarz-Eywill M, Friedberg R, Stosslein F, Unger L, Nusslein H (2005) Rheumatoid arthritis at the cervical spine—an underestimated problem. Dtsch Med Wochenschr 130:1866–1870
Magarelli N, Simone F, Amelia R et al (2010) MR imaging of atlantoaxial joint in early rheumatoid arthritis. Radiol Med 115(7):1111–1120
Ramos-Remus C, Gomez-Vargas A, Guzman-Guzman JL et al (1995) Frequency ofatlantoaxial subluxation and neurologic involvement in patients with ankylosing spondylitis. J Rheumatol 22:2120–2125
Hamdi W, Alaya Z, Ghannouchi MM, Haouel M, Kchir MM (2012) Associated risk factors with worse functional prognosis and hip replacement surgery in ankylosing spondylitis. Joint Bone Spine 79(1):94–96
Slobodin G, Shpigelman A, Dawood H et al (2015) Craniocervical junction involvement in ankylosing spondylitis. Eur Spine J 24(12):2986–2990
El Maghraoui A, Bensabbah R, Bahiri R, Bezza A, Guedira N, Hajjaj-Hassouni N (2003) Cervical spine involvement in ankylosing spondylitis. Clin Rheumatol 22:94–98
Liu J, Zhu L, Jiang E, Zou S, Xu G (2019) Ankylosing spondylitis manifested by extensive cervical Erosions with spontaneous anterior atlantoaxial subluxation. World Neurosurg 122:583–589
Benmansour A, Toussirot E, Wendling D (1996) Upper cervical spine involvement in ankylosing spondylitis. Rachis 8(4):181–192
Chandran V, Barrett J, Schentag CT, Farewell VT, Gladman DD (2009) Axial psoriatic arthritis: update on a longterm prospective study. J Rheumatol 36:2744–2750
Blau RH, Kaufman RL (1987) Erosive and subluxing cervical spine disease in patients with psoriatic arthritis. J Rheumatol 14:111–117
Laiho K, Kauppi M (2002) The cervical spine in patients with psoriatic arthritis. Ann Rheum Dis 61(7):650–652
Jeannou J, Goupille P, Avimadje MA, Zerkak D, Valat JP, Fouquet B (1999) Cervical spine involvement in psoriatic arthritis. Rev Rhum Engl Ed 66(12):695–700
Jenkinson T, Armas J, Evison G, Cohen M, Lovell C, McHugh NJ (1994) The cervical spine in psoriatic arthritis: a clinical and radiological study. Br J Rheumatol 33(3):255–259
Bobek D, Babić-Naglić D, Potocki K, Kern J, Badovinac O, Curković B (2007) The cervical spine involvement in patients with psoriatic arthritis. Reumatizam 54(1):12–15
Salvarani C, Macchioni P, Cremonesi T et al (1992) The cervical spine in patients with psoriatic arthritis: a clinical, radiological and immunogenetic study. Ann Rheum Dis 51:73–77
Mader R, Verlaan JJ, Eshed I et al (2017) Diffuse idiopathic skeletal hyperostosis (DISH): where we are now and where to go next. RMD Open 3(1):e000472
Kagotani R, Yoshida M, Muraki S et al (2015) Prevalence of diffuse idiopathic skeletal hyperostosis (DISH) of the whole spine and its association with lumbar spondylosis and knee osteoarthritis: the ROAD study. J Bone Miner Metab 33(2):221–229
Hiyama A, Katoh H, Sakai D, Sato M, Tanaka M, Watanabe M (2018) Prevalence ofdiffuse idiopathic skeletal hyperostosis (DISH) assessed with whole-spine computed tomography in 1479 subjects. BMC Musculoskelet Disord 19(1):178
Resnick D, Niwayama G (1976) Radiographic and pathologic features of spinal involvement in diffuse idiopathic skeletal hyperostosis (DISH). Radiology 119:559–568
Forestier J, Lagier R (1971) Ankylosing hyperostosis of the spine. Clin Orthop Relat Res 74:65–81
Utsinger PD (1985) Diffuse idiopathic skeletal hyperostosis. Clin Rheum Dis 11:325–355
Leibushor N, Slonimsky E, Aharoni D et al (2017) CT abnormalities in the sacroiliac joints of patients with diffuse idiopathic skeletal hyperostosis. AJR Am J Roentgenol 208:834–837
Slonimsky E, Leibushor N, Aharoni D et al (2016) Pelvic enthesopathy on CT is significantly more prevalent in patients with diffuse idiopathic skeletal hyperostosis (DISH) compared with matched control patients. Clin Rheumatol 35:1823–1827
Olivieri I, D’Angelo S, Palazzi C, Padula A, Mader R, Khan MA (2009) Diffuse idiopathic skeletal hyperostosis: differentiation from ankylosing spondylitis. Curr Rheumatol Rep 11(5):321–328
Vengust R, Mihalic R, Turel M (2010) Two different causes of acute respiratory failure in a patient with diffuse idiopathic skeletal hyperostosis and ankylosed cervical spine. Eur Spine J 19(suppl 2):S130–S134
Gosavi K, Dey P, Swami S (2018) Airway management in case of diffuse idiopathic skeletal hyperostosis. Asian J Neurosurg 13(4):1260–1263
Varsak YK, Eryilmaz MA, Arbağ H (2014) Dysphagia and airway obstruction due to large cervical osteophyte in a patient with ankylosing spondylitis. J Craniofac Surg 25(4):1402–1403
Masiero S, Padoan E, Bazzi M, Ponzoni A (2010) Dysphagia due to diffuse idiopathic skeletal hyperostosis: an analysis of five cases. Rheumatol Int 30:681–685
Carlson ML, Archibald DJ, Graner DE, Kasperbauer JL (2011) Surgical management of dysphagia and airway obstruction in patients with prominent ventral cervical osteophytes. Dysphagia 26:34–40
Giger R, Dulguerov P, Payer M (2006) Anterior cervical osteophytes causing dysphagia and dyspnea: an uncommon entity revisited. Dysphagia 21:259–263
Verlaan JJ, Boswijk PF, de Ru JA, Dhert WJ, Oner FC (2011) Diffuse idiopathic skeletal hyperostosis of the cervical spine: an underestimated cause of dysphagia and airway obstruction. Spine J 11:1058–1067
McAfee PC, Regan JJ, Bohlman HH (1987) Cervical cord compression from ossification of the posterior longitudinal ligament in non orientals. J Bone Joint Surg Br 69:569–575
Aydin E, Akdogan V, Akkuzu B, Kirbaş I, Ozgirgin ON (2006) Six cases of forestier syndrome, a rare cause of dysphagia. Acta Otolaryngol 126:775–778
Cammisa M, de Serio A, Guglielmi G (1998) Diffuse idiopathic skeletal hyperostosis. Eur J Radiol 27:S7–S11
Feydy A, Lioté F, Carlier R, Chevrot A, Drapé JL (2006) Cervical spine and crystal-associated diseases: imaging findings. Eur Radiol 16(2):459–468
Dieppe PA, Alexander GJ, Jones H et al (1982) Pyrophosphate arthropathy: a clinical and radiological study of 105 cases. Ann Rheum Dis 41:371–376
Baba H, Maezawa Y, Kawahara N, Omita K, Furusawa N, Imura S (1993) Calcium crystal deposition in the ligamentum flavum of the cervical spine. Spine 18:2174–2181
Bouvet JP, Le Parc JM, Michalski B, Benlahrache C, Auquier L (1985) Acute neck pain due to calcifications surrounding the odontoid process: the crowned dens syndrome. Arthritis Rheum 28:1417–1420
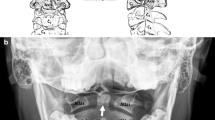
Salaffi F, Carotti M, Guglielmi G, Passarini G, Grassi W (2008) The crowned dens syndrome as a cause of neck pain: clinical and computed tomography study in patients with calcium pyrophosphate dihydrate deposition disease. Clin Exp Rheumatol 26(6):1040–1046
Aouba A, Bodaghi-Vuillemin V, Mutshler C, De Brandt M (2004) Crowned dens syndrome misdiagnosed as polymyalgia rheumatica, giant cell arteritis, meningitis or spondylitis: an analysis of eight cases. Rheumatology 43:1508–1512
Constantin A, Marin F, Bon E, Fedele M, Lagarrigue B, Bouteiller G (1996) Calcification of the transverse ligament of the atlas in chondrocalcinosis: computed tomography study. Ann Rheum Dis 55:137–139
Milz S, Schluter T, Putz R, Moriggl B, Ralphs JR, Benjamin M (2001) Fibrocartilage in the transverse ligament of the human atlas. Spine 26:1765–1771
Kakitsubada Y, Boutin RD, Theodorou DJ et al (2000) Calcium pyrophosphate dehydrate crystal deposition in and around the atlantoaxial joint: association with type 2 odontoid fractures in nine patients. Radiology 216:213–219
Garcia GM, McCord GC, Kumar R (2003) Hydroxyapatite crystal deposition disease. Semin Musculoskelet Radiol 7(3):187–193
Zibis AH, Giannis D, Malizos KN et al (2013) Acute calcific tendinitis of the longus colli muscle: case report and review of the literature. Eur Spine 22(suppl 3):S434–S438
Levy Z, Carroll J, Farley H (2012) Benign nuchal rigidity: the emergency department evaluation of acute prevertebral calcific tendonitis. West J Emerg Med 13:114–116
Wakabayashi Y, Hori Y, Kondoh Y et al (2012) Acute calcific prevertebral tendonitis mimicking tension-type headache. Neurol Med Chir (Tokyo) 52:631–633
Agha RA, Fowler AJ, Saetta A, Barai I, Rajmohan S, Orgill DP, the SCARE group (2016) The SCARE statement: consensus-based surgical case report guidelines. Int J Surgm 34:180–186
Newmark H III, Forrester DM, Brown JC, Robinson A, Oiken SM, Bledsoe R (1978) Calcific tendinitis of the neck. Radiology 128:355–358
Hall FM, Docken WP, Curtis HW (1986) Calcific tendinitis of the longus coli: diagnosis by CT. Am J Roentgenol 147:742–743
Newmark H III, Blackford D, Roberts D, Chakmakian V, Adler J (1986) Computed tomography of acute cervical spine tendinitis. J Comput Tomogr 10:373–375
Eastwood JD, Hudgins PA, Malone D (1998) Retropharyngeal effusion in acute calcific prevertebral tendinitis: diagnosis with CT and MR imaging. Am J Neuroradiol 19:1789–1792
Park R, Halpert DE, Baer A, Kunar D, Holt PA (2009) Retropharyngeal calcific tendinitis: case report and review of the literature. Semin Arthritis Rheum 39(6):504–509
Kim YJ, Park JY, Choi KY, Moon BJ, Lee JK (2017) Case reports about an overlooked cause of neck pain: calcific tendinitis of the longus colli: case reports. Medicine (Baltimore) 96(46):e8343
Omezzine SJ, Hafsa C, Lahmar I et al (2008) Calcific tendinitis of the longus colli: diagnosis by CT. Joint Bone Spine 75:90–91
Alamoudi U, Al-Sayed AA, AlSallumi Y, Rigby MH et al (2017) Acute calcific tendinitis of the longus colli muscle masquerading as a retropharyngeal abscess: a case report and review of the literature. Int J Surg Case Rep 41:343–346
Harnier S, Kuhn J, Harzheim A, Bewermeyer H, Limmroth V (2008) Retropharyngeal tendinitis: a rare differential diagnosis of severe headaches and neck pain. Headache 48(1):158–161
Malca SA, Roche PH, Pellet W, Combalbert A (1995) Crowned dens syndrome: a manifestation of hydroxy-apatite rheumatism. Acta Neurochir 135:126–130
Weinberger A, Myers AR (1978) Intervertebral disc calcification in adults: a review. Semin Arthritis Rheum 8(1):69–75
Bagatur AE, Zorer G, Centel T (2001) Natural history of paediatric intervertebral disc calcification. Arch Orthop Trauma Surg 121:601–603
Chanchairujira K, Chung CB, Kim JY et al (2004) Intervertebral disk calcification of the spine in an elderly population: radiographic prevalence, location, and distribution and correlation with spinal degeneration. Radiology 230:499–503
Lumezanu E, Konatalapalli R, Weinstein A (2012) Axial (spinal) gout. Curr Rheumatol Rep 14(2):161–164
Cheng CW, Nguyen QT, Zhou H (2018) Tophaceous gout of the cervical and thoracic spine with concomitant epidural infection. AME Case Rep 10(2):35
Zhang T, Yang F, Li J, Pan Z (2019) Gout of the axial joint—a patient level systemic review. Semin Arthritis Rheum 48(4):649–657
Konatalapalli RM, Lumezanu EM, Jelinek JS et al (2010) A prospective study of correlates of axial gout. Arthritis Rheum 62:S869
Alarcon-Segovia DA, Cetina JA, Diaz-Jouanen E (1973) Sarcroilaic joints in primary gout. Clinical and roentgenographic study of 143 patients. Am J Roentgenol Radium Ther Nucl Med 118:438–443
Murshid WR, Moss TH, Ettles DF, Cummins BH (1994) Tophaceous gout of the spine causing spinal cord compression. Br J Neurosurg 8:751–754
Tran A, Prentice D, Chan M (2011) Tophaceous gout of the odontoid process causing glossopharyngeal, vagus, and hypoglossal nerve palsies. Int J Rheum Dis 14(1):105–108
Fenton P, Young S, Prutis K (1995) Gout of the spine. Two case reports and a review of the literature. J Bone Joint Surg Am 77:767–771
Neogi T, Jansen TL, Dalbeth N, Fransen J, Schumacher HR, Berendsen D et al (2015) 2015 Gout classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis 74(10):1789–1798
Nicolaou S, Yong-Hing CJ, Galea-Soler S et al (2010) Dual-energy CT as a potential new diagnostic tool in the management of gout in the acute setting. Am J Roentgenol 194:1072–1078
Carotti M, Salaffi F, Beci G, Giovagnoni A (2019) The application of dual-energy computed tomography in the diagnosis of musculoskeletal disorders: a review of current concepts and applications. Radiol Med. https://doi.org/10.1007/s11547-019-01015-x
Gormley W, Rock J (1994) Spontaneous atlantoaxial osteomyelitis: no longer a rare case? Case report. Neurosurgery 35:132–136
Suchomel P, Buchvald P, Barsa P, Lukas R, Soukup T (2003) Pyogenic osteomyelitis of the odontoid process: single stage decompression and fusion. Spine 28:E239–E244
Wetzel FT, La Rocca H (1989) Grisel’s syndrome. Clin Orthop Relat Res 240:141–152
Bocciolini C, Dall’Olio D, Cunsolo E, Cavazzuti PP, Laudadio P (2005) Grisel’s syndrome: a rare complication following adenoidectomy. Acta Otorhinolaryngol Ital 25:245–249
Sia KJ, Tang IP, Kong CK, Nasriah A (2012) Grisel’s syndrome: a rare complication of tonsillectomy. J Laryngol Otol 126(5):529–531
Kobayashi T, Miyakoshi N, Konno N, Abe E, Ishikawa Y, Shimada Y (2014) Acute neck pain caused by arthritis of the lateral atlantoaxial joint. Spine J 14:1909–1913
Coheh SP (2015) Epidemiology, diagnosis, and treatment of neck pain. Mayo Clin Proc 90(2):284–299
Frazier DD, Campbell DR, Garvey TA, Wiesel S, Bohlman HH, Eismont FJ (2001) Fungal infections of the spine. Report of eleven patients with long-term follow-up. J Bone Joint Surg Am 83:560–565
Ueda Y, Kawahara N, Murakami H, Matsui T, Tomita K (2009) Pyogenic osteomyelitis of the atlas: a case report. Spine (Phila Pa 1976) 34:E342–E345
Sasaki K, Nabeshima Y, Ozaki A et al (2006) Septic arthritis of the atlantoaxial joint: case report. J Spinal Disord Tech 19:612–615
Kanaan IU, Ellis M, Safi T, Al Kawi MZ, Coates R (1999) Craniocervical junction tuberculosis: a rare but dangerous disease. Surg Neurol 51:21–25
Lifeso R (1987) Atlanto-axial tuberculosis in adults. J Bone Joint Surg Br 69:183–187
Chaudhary K, Potdar P, Bapat M, Rathod A, Laheri V (2012) Structural odontoid lesions in craniovertebral tuberculosis: a review of 15 cases. Spine (Phila Pa 1976) 37(14):E836–E843
Kotil K, Dalbayrak S, Alan S (2004) Craniovertebral junction Pott’s disease. Br J Neurosurg 18:49–55
Raut AA, Narlawar RS, Nagar A et al (2003) An unusual case of CV junction tuberculosis presenting with quadriplegia 28:E309
Funding
This work has not been supported by any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
This article does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Salaffi, F., Carotti, M., Di Carlo, M. et al. Craniocervical junction involvement in musculoskeletal diseases: an area of close collaboration between rheumatologists and radiologists. Radiol med 125, 654–667 (2020). https://doi.org/10.1007/s11547-020-01156-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-020-01156-4