Abstract
To determine the cross-immunity between influenza strains, we design a novel statistical method, which uses a theoretical model and clinical data on attack rates and vaccine efficacy among school children for two seasons after the 1968 A/H3N2 influenza pandemic. This model incorporates the distribution of susceptibility and the dependence of cross-immunity on the antigenic distance of drifted strains. We find that the cross-immunity between an influenza strain and the mutant that causes the next epidemic is 88%. Our method also gives estimates of the vaccine protection against the vaccinating strain, and the basic reproduction number of the 1968 pandemic influenza.
Similar content being viewed by others
1 Introduction
Influenza is an important cause of morbidity and mortality in humans (Earn et al. 2002). Seasonal influenza accounts for more than 41,000 deaths each year in North America (Dushoff et al. 2006), whereas the 1918 influenza pandemic is estimated to have caused approximately 50 million deaths (Taubenberger et al. 2005). Influenza is caused by a fast mutating RNA virus in the family of Orthomyxoviridae (Earn et al. 2002). There are three type of influenza, namely A, B and C. Influenza A accounts for the majority of seasonal influenza deaths (Dushoff et al. 2006) and has caused all the pandemics since 1918. Influenza A undergoes two types of evolution (i) antigenic drift (point mutations) and (ii) antigenic shift (gene reassortment) (Earn et al. 2002; Webster et al. 1992). Antigenic shift produces new influenza A subtypes (Taubenberger et al. 2000), and these subtypes have caused four major pandemic outbreaks in the last century (Webster 1998). Antigenic drift is a rapid minor genetic variation in the RNA segments in currently circulating subtypes (Taubenberger et al. 2000; Webster et al. 1992). Due to this drift evolution, seasonal influenza outbreaks occur in almost every winter, usually November–April in the Northern hemisphere (the influenza season) (Earn et al. 2002; Webster 1998).
Seasonal influenza A strains tend to group in antigenic clusters rather than form a continuous antigenic lineage (Smith et al. 2004). Usually the strains in a cluster have small antigenic distance (number of different epitopes) and remain dominant for 3.3 seasons on average before a new cluster at a larger antigenic distance emerges (Smith et al. 2004). This makes it very difficult to predict which strains are going to cause an outbreak in the next season. Influenza vaccine is a main strategy for prevention and control of seasonal and pandemic influenza (Earn et al. 2002; Davenport 1962). The usual practice is that influenza vaccines are administered before the start of the seasonal epidemic. Due to antigenic drift, influenza vaccines (that are derived from the strains in the past season) are not completely protective in the next season against infection by drifted strains. However, influenza vaccine and natural infection give rise to cross-immunity (Yu et al. 2008; Potter 1979), that is, the reduction in the probability of infection to challenging strains. This probability is also called susceptibility. That is, for any individual, the cross-immunity and the susceptibility sum up to unity.
Cross-immunity reduces the final size (the fraction of individuals infected in an influenza outbreak, also called the attack rate) of seasonal epidemics because it reduces the probability of infection upon challenge. This reduction also reduces the number of challenges. The total reduction is reflected by a nonlinear relationship between the final size and the basic reproduction number (Ma and Earn 2006). The resulting change in final size influences the distribution of susceptibility in the population, which in turn shapes the natural selection of influenza strains (Ferguson et al. 2003). In addition, cross-immunity between the vaccine and challenging strains is a crucial measure for vaccine protection. Kucharski et al. (2015) developed a mechanistic model to measure cross-reactivity of antibodies to a challenging strain given a history of influenza A/H3N2 infection. They estimated that the exponential decay of cross-reactivity has the rate 0.29 per year. In the study by Kucharski et al. (2015), there are two limitations. One is that they considered in vitro response (cross-reactivity), which does not always represent the in vivo response (cross-immunity), since the latter involves complex mechanisms in addition to antibody cross-reactivity. The second is that they assumed that cross-reactivity decays exponentially with time, implying that the strain in one season directly evolves from the strain of the previous season. The genetic evolution of these strains is commonly represented by a phylogenetic tree (Viboud et al. 2005). Thus, the antigenic change can be represented by a similar tree, called the evolutionary tree of antigens. The second assumption of Kucharski et al. (2015) corresponds to a linear evolutionary tree of antigens.
We consider in vivo response with realistic evolutionary trees of antigens and estimate the cross-immunity between strains of influenza A on the evolutionary tree. We develop a theoretical model that takes into account both the drift evolution (antigenic distance of influenza strains) and the cross-immunity gained from previous infections reducing the susceptibility to related strains of influenza. We fit our model to immune response data for influenza epidemics from the Seattle area for two seasons after the 1968 pandemic. We group influenza strains by their antigenic distance into a tree structure. Considering different evolutionary trees of antigens in our model, we determine the most likely structure during these seasons, which agrees with the observed tree structure found by Viboud et al. (2005). From our model, we also estimate the basic reproduction number of the pandemic influenza A/H3N2.
2 Sources of Data
The average cross-immunity in the population not only determines the attack rate of a seasonal epidemic (Andreasen 2003; Asaduzzaman et al. 2015), but also depends on the attack rate of previous seasons. The attack rate in turn depends on the distribution of susceptibility in the population. It is difficult to estimate this distribution for seasonal epidemics, except for the seasons immediately following a pandemic. In the season following a pandemic, individuals are either completely susceptible to a challenging strain (those who escaped the pandemic) or have the same cross-immunity (those who were infected by the pandemic). This gives us the initial condition for our model of the evolution of the distribution of susceptibility. Thus, we use the attack rates in the seasons immediately following the 1968 pandemic as given in Foy et al. (1971, 1973) for 1968–1971.
Time line of the A/H3N2 influenza study of Foy et al. (1971, 1973). The dotted line indicates the duration of the pandemic influenza in 1968, the solid lines indicate the summer time between influenza epidemics, and the broken lines indicate the duration of typical seasonal influenza epidemics. Influenza vaccine was administered in November–December 1968; blood samples were collected in March 1969, March 1970 and March–April 1972
Foy et al. (1973) conducted a field study among school children to evaluate the efficacy of a single dose of monovalent influenza vaccine. The study began in late November and early December of 1968 (Fig. 1) by vaccinating junior high school children in the Seattle urban and suburban areas; a total of 4133 children were vaccinated with influenza A/Aichi/2/68(H3N2) or influenza B/Mass/66 strain on one occasion only. On a random basis, half of the children received influenza A vaccine (the study group) and half received influenza B vaccine. The children who received influenza B vaccine are taken as the control group, since influenza B vaccine is not effective against influenza A. At the time of vaccination, a random 20% of the children had blood samples collected, and vaccinated children were monitored for a period of 3 years. Following the pandemic that peaked in December 1968, blood samples were collected again in March 1969; see Fig. 1 for the time line. An influenza A/H3N2 strain caused a seasonal influenza epidemic during the influenza season of 1969–1970. After this seasonal epidemic, blood samples were collected in March 1970 (Fig. 1) for serological analyses and estimating infection rates among vaccinated children. A fourfold or greater titer rise in Complement Fixation or Hemagglutination Inhibition or both tests were taken as infection during the influenza season. A sample of 165 influenza A vaccine and 152 influenza B vaccine recipients were tested for influenza infection in March 1970. There was no seasonal epidemic in the 1970–1971 season in the Seattle urban and suburban areas (Foy et al. 1973). Following the seasonal A/H3N2 epidemic in the influenza season of 1971–1972, blood samples were collected in March–April 1972; serological analyses of blood samples for influenza infection were based on 147 influenza A vaccine and 156 influenza B vaccine recipients. The results of serological analyses of blood samples are summarized in Table 1.
Our method also depends on the pandemic attack rate in the general population, which is not available in Foy et al. (1971, 1973). However, Davis et al. (1970) provide this information in a similar high school population in another metropolitan area. Davis et al. (1970) conducted a retrospective questionnaire survey among high school students and their families in the Kansas City area for histories of influenza like illness between November 1, 1968, and January 17, 1969, during the A/H3N2 influenza pandemic. On January 17, 1969, each student was requested to donate a blood sample for serologic studies of influenza infection. A total of 139 students out of 285 samples were found with antibody titers of at least 1:10 of influenza A/H3N2, giving an estimate of 49% for the serologically confirmed attack rate of the pandemic.
3 Modeling the Dynamics of Seasonal Influenza
3.1 Population Model
We adapt a theoretical model from Andreasen (2003), Andreasen and Sasaki (2006), Asaduzzaman et al. (2015) to investigate the cross-immunity between influenza strains depending on the evolutionary tree of antigens of influenza A/H3N2. Following the time line (Fig. 1), we fit the model to the influenza epidemic data in Table 1 for the 1969–1970 and 1971–1972 seasons in the Seattle area. Our model requires the knowledge of the immune status of susceptible individuals. To represent these immune status classes in the current season c, we introduce the symbol \(S_\ell ^c\) as the fraction of susceptible individuals who had their last seasonal influenza in season \(\ell \), and \(S_0^c\) as the fraction of susceptible individuals who have never been infected by the influenza A/H3N2 subtype.
The flow of individuals among the \(S_\ell ^c\) classes is depicted in Fig. 2. Let \(\epsilon \) be the proportion of individuals vaccinated who had an antibody response. For simplicity, we assume that natural infection and effective vaccination have the same level of immunological response. Thus, after the pandemic in 1968, the \(S_{68}^{68}\) class contains individuals who were either effectively vaccinated or infected during the pandemic. That is,
where \(A^{68}\) is the attack rate of the pandemic. In the vaccinated study group, because everyone is vaccinated, \(\epsilon \) is the fraction of vaccine recipients with an antibody response. For individuals who have no antibody response to the vaccine, a fraction \(A^{68}(1-\epsilon )\) were infected by the pandemic, and a fraction
escaped the pandemic.
For \({\ell } \in \{0, 68\}\), the classes \(S_{\ell }^{69}\) contain individuals in \(S_{\ell }^{68}\) who escaped influenza in the 1969–1970 season, and individuals who were infected during that season belong to \(S_{69}^{69}\). We assume that a fraction of individuals \(\phi _{\ell }^{69}\) (with \(0<\phi _{\ell }^{69}<1)\) for \({\ell } \in \{0, 68\}\) in \(S_{\ell }^{68}\) escaped influenza and a fraction \(1-\phi _{\ell }^{69}\) were infected by influenza in the 1969–1970 season. Thus,
There was no observed influenza epidemic in the Seattle area in 1970–1971 season (Foy et al. 1973), but an epidemic was observed in the 1971–1972 season. Thus, similarly at the end of the 1971–1972 epidemic season, individuals belonging to \(S_{\ell }^{71}\) for \({\ell } \in \{0, 68, 69\}\) and \(S_{71}^{71}\) classes are found as follows
where \(\phi _{\ell }^{71}\) is the fraction of individuals in \(S_{\ell }^{69}\) for \({\ell } \in \{0, 68, 69\}\) who escaped influenza infection during the 1971–1972 season. Knowing the parameters \(\epsilon \), \(A^{68}\), and \(\phi _{\ell }^{69}\) for \({\ell } \in \{0, 68\}\) and \(\phi _{\ell }^{71}\) for \({\ell } \in \{0, 68, 69\}\), the flow of individuals among \(S_{\ell }^c\) classes are completely determined by (1)–(6). In Sect. 3.2, we model the transmission dynamics of seasonal influenza with an SIR-type model to determine the parameters \(\phi _{\ell }^{69}\) and \(\phi _{\ell }^{71}\).
3.2 Seasonal Epidemic Model
We model the dynamics of seasonal influenza by taking into account an individual’s infection history since this determines the cross-immunity of an individual to the challenging strain (Andreasen 2003; Kucharski et al. 2015). Like Andreasen (2003), we assume that the level of cross-immunity is determined by the most recent infection. We denote by \(s_{\ell }^c(t)\) the fraction of susceptible individuals in season c at time t whose infection history belongs to \(\ell \), by i(t) the fraction of infected and infectious individuals, and by r(t) the fraction of recovered individuals. For \(c=69\), an individual’s infection history \(\ell \) belongs to \(\{0, 68 \}\), and \(\ell \in \{0, 68, 69 \}\) for \(c=71\). We ignore birth and death processes; thus, \(\sum _{\ell }s_{\ell }^c+i+r=1\) is a constant. We assume that individuals in \(s_{\ell }^c\) with \(\ell \ne 0\) have susceptibility \(\tau _{\ell }^c\). Individuals in \(s_0^c\) are assumed to have complete susceptibility, i.e., \(\tau _0^c=1\). We introduce nondimensional time such that the infectious period is 1. The transmission dynamics of influenza for the season 1969–1970 evolves according to the ordinary differential equations
The initial conditions are \(s_{\ell }^{69}(0)=S_{\ell }^{68}\) for \(\ell \in \{0, 68\}\) (from Sect. 3.1), i(0) is positive and small, and \(r(0)=0\). We assume that seasonal epidemics occur on a fast time scale, where the end of the epidemic is denoted by time \(\infty \); thus, \(r(\infty )=S_{69}^{69}\) and \(s_{\ell }^{69}(\infty )=S_{\ell }^{69}\). From (3), in this model \(\phi _{\ell }^{69}=\frac{S_{\ell }^{69}}{S_{\ell }^{68}}=\frac{s_{\ell }^{69}(\infty )}{s_{\ell }^{69}(0)}\) for \(\ell \in \{0, 68\}\). The final state of the seasonal epidemic can be calculated from (7a) by observing that
and integrating on the fast time scale from 0 to \(\infty \) gives
that is
To determine \(\phi _{0}^{69}\), sum (7a)and (7b) and integrate from 0 to \(\infty \)
At the beginning of the epidemic, i(0) is very small, so it can be taken as zero, and at the end of the epidemic \(i(\infty )\) is zero because no one is infectious anymore. Thus, using (9), the final size equation from (10) can be written as
Similarly, using \(s_{\ell }^{71}(0)=S_{\ell }^{69}\) for \(\ell \in \{0, 68, 69\}\), it follows that
and
With (9), (11)–(13), Eqs. (3)–(6) determine \(S_{\ell }^{69}\) and \(S_{\ell }^{71}\) once \(\tau _{\ell }^{69}\) and \(\tau _{\ell }^{71}\) are modeled; see Sect. 3.3.
3.3 Evolutionary Trees of Antigens
Figure 3 lists all possible canonical evolutionary trees of antigens of influenza A/H3N2 for the strains appearing in the 1969–1970 and 1971–1972 seasons, rooted at the 1968 pandemic strain. A node a represents the influenza strain in year a that caused an epidemic, and an arc connects from node a to node b if strain b evolves from strain a and causes an epidemic in year b. We define the unit antigenic distance as the average number of epitopes between two strains connected by an arc. Thus, the antigenic distance \(d(c, \ell )\) is the number of arcs between the nodes c and \(\ell \) on the evolutionary tree of antigens. For example, in Fig. 3, Model 1 assumes that the 69 strain is a mutant of (i.e., evolves from) the 68 strain, and the 71 strain is a mutant of the 68 strain, with \(d(68, 69)=1\) and \(d(68,71)=2\). Model 2 assumes that the 71 strain is a mutant of some \(70'\) strain that did not appear in the Seattle area, which is a mutant of the 69 strain. Model 3 assumes that the 69 and 71 strains are independent mutants of the 68 strain, and in Models 4–5 the 71 strain is a descendant of some \(70'\) strain that did not appear in the Seattle area; thus, for instance, in Model 5, \(d(68,71)=3\) and \(d(69,71)=4\).
We assume as Boni et al. (2006) that the cross-immunity decays exponentially with antigenic distance. This gives \(\tau _\ell ^c=1-q^{d(c,\ell )}\) as the susceptibility in the current season c, where q is the cross-immunity between strains connected by an arc. With parameters \(\epsilon \), q, \(\mathcal {R}_0\) and \(A^{68}\) and the evolutionary tree, the flow in Fig. 2 is uniquely determined.
4 Statistical Method for Parameter Estimation
We use the maximum likelihood method to estimate the cross-immunity q between influenza strains depending on the tree of A/H3N2 with unit antigenic distance, the vaccine protection \(\epsilon \) against the vaccinating strain, the basic reproduction number \(\mathcal {R}_0\), and the attack rate of the 1968 pandemic \(A^{68}\) by fitting the model of Sect. 3 to the four data points in Table 1. We assume that each individual has the same probability of being infected during the pandemic influenza or seasonal influenza after the pandemic. Denote by \(X^{68}\) the number of infected individuals in a sample of size N during the pandemic. Thus, \(X^{68}\) follows a Binomial distribution with parameter \(A^{68}\) and sample size N, i.e., \(X^{68} \sim \text {BIN}(N,A^{68})\), where \(X^{68}\) and N are, respectively, 139 and 285 from Davis et al. (1970); see Sect. 2.
Let \(X^c\) and \(\tilde{X}^c\) be the number of infected individuals among influenza A and influenza B vaccinated individuals (control group) in a sample of size \(N^c\) and \(\tilde{N}^c\) in a season c, where \(c=69\) for the 1969–1970 season and \(c=71\) for the 1971–1972 season. The numerator and denominator of the first column of Table 1 correspond to \(X^{c}\) and \(N^{c}\), and the numerator and denominator of the second column of Table 1 correspond to \(\tilde{X}^{c}\) and \(\tilde{N}^{c}\) for a season c. We determine the attack rate of seasonal influenza in the 1969–1970 and 1971–1972 seasons in the influenza A vaccine recipient (\(\epsilon >0\)) and influenza B vaccine recipient (\(\epsilon =0\)) populations and taking these attack rates as a probability of infection during the seasonal influenza, \(X^{69} \sim \text {BIN}(N^{69},S_{69}^{69})\), \(X^{71} \sim \text {BIN}(N^{71}, S_{71}^{71})\) and \(\tilde{X}^{69} \sim \text {BIN}(\tilde{N}^{69}, \tilde{S}_{69}^{69})\), \(\tilde{X}^{71} \sim \text {BIN}(\tilde{N}^{71}, \tilde{S}_{71}^{71})\), where \(\tilde{S}_{69}^{69}\) and \(\tilde{S}_{71}^{71}\) denote the attack rates of seasonal influenza among influenza B vaccinated individuals in the 1969–1970 and 1971–1972 seasons. The log likelihood function of the parameters q, \(\epsilon \),\(\mathcal {R}_0\) and \(A^{68}\) is
where F(X; N, p) is the probability mass function of a Binomial random variable. We find the set of parameters for influenza A/H3N2 that maximizes the log likelihood function \(\mathcal {L}\) in (14) by using MATLAB fmincon function. The Akaike information criterion
where k is the number of parameters (\(k=4\)), is computed for the relative quality of the models for the data in Table 1. The 95% confidence interval for the parameters is found from the likelihood ratio test; see, for example, (Bain and Engelhardt 2000, pp. 417–422).
5 Model Validation and Results
The point estimates of the parameters of the models in Fig. 3 (with their corresponding \(\tau _{\ell }^c\)) and their AIC are summarized in Table 2. Among the candidate models in Fig. 3, the preferred model (minimum AIC) is Model 5. These five models have the same number of parameters, so the order of Bayesian information criterion (BIC) is the same as that for AIC. Viboud et al. (2005) presented an evolutionary tree for the influenza H3 gene during the period including 1968–1972. This suggests that the 69 and 71 strains are two different branches of the 68 strain. Our best fit evolutionary tree of antigens agrees with that of the evolutionary tree of the H3 gene, but differs from that of the N2 gene, given by Viboud et al. (2005, Fig. 4).
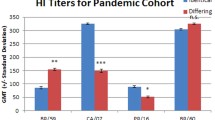
From the data in Table 1 and the susceptibility structure of the best fit evolutionary tree of antigens (Model 5, Fig. 3), we estimate that the cross-immunity between influenza strains with unit antigenic distance q is 88% (85–91%), the vaccine protection against the vaccinating strain \(\epsilon \) is 99% (65–100%), the basic reproduction number \(\mathcal {R}_0\) is 2.15 (1.84–2.59), and the attack rate of the pandemic \(A^{68}\) is 49% (42–56%.). The likelihood profile of the parameters is shown in Fig. 4. The point and interval estimates of the parameters are summarized in Table 3, with the distribution of the attack rate for each season given in Fig. 5.
Since there was no observable epidemic in the Seattle area in the 1970–1971 season, the strain \(70'\) may be a descendent of strain 69, 68 or \(69'\) (the latter is depicted in Model 5). Our estimated parameters yield a very small attack rate in the 1970–1971 influenza season (Fig. 5a–c), agreeing with the observation of Foy et al. (1973) that there was no observable epidemic in the 1970–1971 season.
6 Discussion
We used a novel statistical model to investigate the cross-immunity between strains of influenza A/H3N2. Our model incorporated the knowledge of the immune status of susceptible individuals depending on the evolutionary tree of antigens of influenza A/H3N2. The value of the cross-immunity between an influenza strain and its mutant strains implies that an individual infected by a strain has 12% probability of infection by a mutant strain in the next seasonal epidemic. We also determined that the vaccine is highly effective in inducing an immune response. Thus, a vaccinated individual can expect an infection with probability \(\le 0.01\) if the season’s influenza outbreak is caused by the vaccinating strain. Cross-immunity is a better measure of vaccine protection than vaccine efficacy because the latter depends on factors that are not related to the vaccine, for example, the probability of individuals in an unvaccinated population being challenged by the circulating strain.
(Color figure online) Distribution of the influenza A/H3N2 attack rates is given by boxplots, where the whiskers represent the 95% confidence intervals. The observed attack rates in the seasons 1969–1970 and 1971–1972 are depicted with a diamond \(\diamond \) symbol (given in Table 1). The labels 69C, 71C and 69V, 71V represent control and vaccinated groups of individuals in these years. For the 1970–1971 season, the strain that may have challenged in the Seattle area could be (a) a descendant of the 69 strain as in Model 2, (b) a descendant of the 68 strain as in Model 4 or (c) a descendant of some \(69'\) strain and the parent of the 71 strain as in Model 5
In a study of individuals tested against nine different influenza A/H3N2 strains isolated between 1968 and 2008, Kucharski et al. (2015) found a value \(\mathrm{e}^{-0.29}\approx 0.75\) roughly corresponding to our q, which is lower than the range in Table 3. This may be because we focused only on years following the 1968 pandemic, and strains from consecutive seasons may be on different branches of the evolutionary tree (Model 5) resulting in a smaller cross-immunity between seasons. In addition, in vivo cross-immunity is expected to be larger than in vitro cross-immunity because of more types of immune response.
The basic reproduction number \(\mathcal {R}_0\) of the 1968 pandemic influenza that we estimated agrees with previously estimated values of 1.5–2.2 in Cooper et al. (2006) and 1.60–2.12 in Jackson et al. (2010). The data that we used are for school children, who have higher contact rates than other age groups. So we expect that the attack rate and the basic reproduction number would be lower in a general population.
Our model assumes that the antigenic drift in each season is the same. However, some theoretical studies (e.g., Boni et al. 2006) suggest that the antigenic drift of the pandemic strain is larger than that of the seasonal strain of influenza because the pandemic has a much greater attack rate. We model this by assuming the cross-immunity between the 68 and 69 (or \(69'\)) strain is equal to \(\gamma q\), where \(\gamma \in [0, 1]\). The cross-immunity between the 69 and 71 strains becomes \(\gamma ^2 q^4\) in Model 5. For simplicity, we assume that the vaccine is effective for all individuals, i.e., \(\epsilon =1\). Running Model 5 with this hypothesis, the point estimates of the parameters remain identical with the values given in Table 3, and \(\gamma =1\). Thus, our model cannot distinguish this hypothesis, but it does not affect our estimates of cross-immunity q, and the basic reproduction number \(\mathcal {R}_0\). Our model also assumes that the effectiveness of the vaccine is all or nothing. However, the vaccine could be leaky (Halloran et al. 2010), i.e, every vaccinated individual is protected to some extent, but has a probability of infection. We need a new model to explore this hypothesis.
Our theoretical model connects the susceptibility distribution with the influenza evolutionary tree of antigens. Thus, a variant of our model in Sect. 3 can be used to study the evolution of influenza after any pandemic. Our findings of cross-immunity between influenza strains can be used to compute the basic reproduction number (fitness) of the challenging strain. This information may be helpful for predicting which strain of influenza may cause the next season’s epidemic, and give better suggestions for the composition of a seasonal influenza vaccine.
References
Andreasen V (2003) Dynamics of annual influenza A epidemics with immuno-selection. J Math Biol 46:504–536
Andreasen V, Sasaki A (2006) Shaping the phylogenetic tree of influenza by cross-immunity. Theor Popul Biol 70(2):164–173
Asaduzzaman SM, Ma J, van den Driessche P (2015) The coexistence or replacement of two subtypes of influenza. Math Biosci 270:1–9
Bain LJ, Engelhardt M (2000) Introduction to probability and mathematical statistics, 2nd edn. Duxbury Press, Pacific Grove
Boni MF, Gog JR, Andreasen V, Feldman MW (2006) Epidemic dynamics and antigenic evolution in a single season of influenza A. Proc R Soc Lond B Biol Sci 273:1307–1316
Cooper BS, Pitman RJ, Edmunds WJ, Gay NJ (2006) Delaying the international spread of pandemic influenza. PLoS Med 3(6):e212
Davenport FM (1962) Current knowledge of influenza vaccine. JAMA 182:11–13
Davis LE, Caldwell GG, Lynch RE, Bailey RE, Chin TDY (1970) Hong Kong influenza: the epidemiologic features of a high school family study analyzed and compared with a similar study during the 1957 Asian influenza epidemic. Am J Epidemiol 92(4):240–247
Dushoff J, Plotkin JB, Viboud C, Earn DJ, Simonsen L (2006) Mortality due to influenza in the United States—an annualized regression approach using multiple-cause mortality data. Am J Epidemiol 163(2):181–187
Earn D, Dushoff J, Levin SA (2002) Ecology and evolution of the flu. Trends Ecol Evol 17(7):334–340
Ferguson NM, Galvani AP, Bush RM (2003) Ecological and immunological determinants of influenza evolution. Nature 422:422–433
Foy HM, Cooney MK, McMahan R, Bor E, Grayston JT (1971) Single dose monovalent A/Hong Kong influenza vaccine efficacy 14 months after immunization. JAMA 217(8):1067–1071
Foy HM, Cooney MK, McMahan R (1973) A Hong Kong influenza immunity three years after immunization. JAMA 226(7):758–761
Halloran ME, Longini IM Jr, Struchiner CJ (2010) Design and analysis of vaccine studies. Springer, Berlin
Jackson C, Vynnycky E, Mangtani P (2010) Estimates of the transmissibility of the 1968 (Hong Kong) influenza pandemic: evidence of increased transmissibility between successive waves. Am J Epidemiol 171:465–478
Kucharski AJ, Lessler J, Read JM, Zhu H, Jiang CQ, Guan Y et al (2015) Estimating the life course of influenza A (H3N2) antibody response from cross-sectional data. PLoS Biol 13(3):e1002082
Ma J, Earn DJD (2006) Generality of the final size formula for an epidemic of a newly invading infectious disease. Bull Math Biol 68:679–702
Potter CW (1979) Determinants of immunity to influenza infection in man. Br Med Bull 35:69–75
Smith DJ, Lapedes AS, de Jong JC, Bestebroer TM, Rimmelzwaan GF, Osterhaus ADME et al (2004) Mapping the antigenic and genetic evolution of influenza virus. Science 305(5682):371–376
Taubenberger JK, Reid AH, Fanning TG (2000) The 1918 influenza virus: a killer comes into view. Virology 274:241–245
Taubenberger JK, Reid AH, Lourens RM, Wang R, Jin G, Fanning TG (2005) Characterization of the 1918 influenza virus polymerase gene. Nature 437:889–893
Viboud C, Grais RF, Lafont BAP, Miller MA, Simonsen L (2005) Multinational impact of the 1968 Hong Kong influenza pandemic: evidence for a smoldering pandemic. J Infect Dis 192(2):233–248
Webster RG (1998) Influenza: an emerging disease. Emer Infect Dis 4(3):436–441
Webster RG, Bean WJ, Gorman OT, Chambers TM, Kawaoka Y (1992) Evolution and ecology of influenza A viruses. Microbiol Rev 56(1):152–179
Yu X, Tsibane T, McGraw PA, House FS, Keefer CJ et al (2008) Neutralizing antibodies derived from the B cells of 1918 influenza pandemic survivors. Nature 455:532–536
Acknowledgements
This research is partially supported by NSERC Discovery grants to JM and PvdD. We thank the anonymous reviewers for their constructive comments and suggestions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Asaduzzaman, S.M., Ma, J. & van den Driessche, P. Estimation of Cross-Immunity Between Drifted Strains of Influenza A/H3N2. Bull Math Biol 80, 657–669 (2018). https://doi.org/10.1007/s11538-018-0395-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11538-018-0395-5