Abstract
Fulvestrant is recommended for patients with hormone receptor-positive (HR+) advanced breast cancer (ABC) who progress after aromatase inhibitor therapy. As most patients in this setting have already developed mechanisms of resistance to endocrine therapy, targeting biological pathways associated with endocrine resistance in combination with fulvestrant may improve outcomes. Therefore, evidence supporting a combinatorial treatment approach in the second-line setting was investigated based on a search of PubMed and ClinicalTrials.gov. Twenty-eight studies of targeted therapies plus fulvestrant as second-line treatment for HR+ ABC were identified, including three and six key randomized trials exploring cyclin-dependent kinase 4/6 (CDK4/6) inhibitors and phosphatidylinositol 3-kinase (PI3K)/mammalian target of rapamycin (mTOR) inhibitors plus fulvestrant respectively. Additional combinations with fulvestrant included inhibitors of epidermal growth factor receptors, androgen receptor, and the bromodomain and extra-terminal family of proteins. Across the studies reviewed with available data, the addition of targeted therapies to fulvestrant resulted in clinically meaningful improvements in progression-free survival compared with fulvestrant alone. While some challenging toxicities were observed, most adverse events could be effectively managed. Selection of second-line targeted therapy for use with fulvestrant should consider prior treatment as well as the mutation status of the tumor. In conclusion, available data indicate that fulvestrant combined with agents targeting mechanisms of endocrine resistance is a promising approach. The ongoing trials identified in this review will help further inform the selection of combination treatments with fulvestrant for HR+ ABC.
Similar content being viewed by others
In the second-line setting, there are several recommended treatment options for patients with hormone receptor-positive (HR+) advanced breast cancer (ABC) with progression after aromatase inhibitor therapy including fulvestrant-based combination therapies |
Fulvestrant combined with targeted therapies that inhibit activated signaling pathways in estrogen receptor-positive ABC shows greater benefit than either therapy alone |
Further research of various targeted therapies such as CDK4/6 inhibitors, PI3K inhibitors, tyrosine kinase inhibitors, and AR inhibitors will help to determine additional therapeutic options for fulvestrant-based treatment combinations in the second-line setting of HR+ ABC |
1 Introduction
Breast cancer is the most common cancer in women, with an estimated 2,400,000 cases and 523,000 deaths worldwide in 2015 [1]. Approximately 60–80% of breast cancer cases are hormone receptor-positive (HR+), and the highest incidence is observed in older, postmenopausal women [2,3,4,5]. The standard of care for the treatment of HR+ breast cancer is endocrine therapy (ET), which blocks the growth-promoting effects of estrogen via the estrogen receptor (ER) [6, 7]. There are several types of ET available that work via the following mechanisms: selective ER modulators (SERMs; e.g., tamoxifen), which exert dual agonistic/antagonistic effects on ER transcription; third-generation aromatase inhibitors (AIs; e.g., letrozole, anastrozole, and exemestane), which inhibit estrogen biosynthesis; and the selective ER down-regulator (SERD) fulvestrant, which binds and prevents ER dimerization, leading to rapid degradation and loss of cellular ER [3, 8].
First-line endocrine therapies for HR+ advanced breast cancer (ABC) have been reviewed recently [9]. In the advanced and adjuvant settings, the SERM tamoxifen and AIs comprise the standard of care and are backbone ETs [6, 7, 10]. In patients with HR+ ABC, the addition of a cyclin-dependent kinase 4 and 6 (CDK4/6) inhibitor to an AI has prolonged progression-free survival (PFS) and is an option for first-line treatment of advanced disease [10,11,12]. Fulvestrant received U.S. Food and Drug Administration approval as a monotherapy in the first-line setting (for ET-naïve patients) [13] after significantly improving PFS compared with anastrozole in an ET-naïve population (corresponding to a 20% reduction in the risk of disease progression or death; hazard ratio [HR] 0.80 [95% confidence interval {CI} 0.64–1.0]; P < 0.049) [14]. Both treatments were associated with an acceptable safety profile, with the most common adverse events (AEs) among patients who received fulvestrant (500 mg) vs anastrozole (1 mg) being (≥ 10% any grade) arthralgia 17% vs 10%, hot flash 11% vs 10%, fatigue 11% vs 7%, and nausea 11% vs 10% [14]. Despite the advances in the first-line setting, endocrine resistance eventually develops and disease progresses [8, 15,16,17].
In the second-line setting, fulvestrant is one of a variety of recommended options for patients with HR+ ABC with progression after AI therapy [6, 7, 10]. The use of second-line fulvestrant monotherapy in patients with HR+ ABC is well tolerated, but has limited efficacy [18, 19]. The phase 3 CONFIRM trial comparing single-agent fulvestrant 500 mg vs 250 mg reported median PFS intervals of 6.5 and 5.5 months respectively [18]. The statistically significant increase in PFS (HR 0.80 [95% CI 0.68–0.94]; P < 0.006) with no increased toxicity in the CONFIRM trial supported the use of the 500 mg dose [18]. Therefore, the recommended dose for fulvestrant is 500 mg injected intramuscularly on days 1, 15, and 29, and then once monthly [6]. The most common side-effects of single-agent fulvestrant 500 mg from the CONFIRM trial were (≥ 10% any grade; grouped terms) gastrointestinal (GI) disturbances (20%), joint pain (19%), and injection site reactions (14%) [18]. However, fulvestrant is extremely well tolerated overall, with rare occurrence of grade 3 adverse events (AEs), thus lending itself to combination therapy [8]. In a recent review, fulvestrant is the only ET that improved PFS and overall survival (OS) in both the first- and second-line treatment of HR+ ABC [20].
One potential shortcoming of second-line fulvestrant monotherapy is that many patients in this setting have already developed resistance to ET [8, 18, 19, 21]. Studies have shown that common mechanisms of endocrine resistance include the upregulation of pathways downstream of ER signaling and adaptive cross-talk between ER and growth factor receptor signaling pathways [16, 22, 23]. Targeting the key biological pathways associated with endocrine resistance may be a rational approach for combination therapy with fulvestrant (Fig. 1) [24]. Clinical trials of several types of targeted therapy in combination with fulvestrant in the second-line setting are either ongoing or have recently reported data. These include the CDK4/6 inhibitors palbociclib, ribociclib, and abemaciclib [19, 25, 26]; the mammalian target of rapamycin (mTOR) inhibitors everolimus (mTOR complex 1 [mTORC1] inhibitor) and vistusertib (mTORC1 and mTOR complex 2 [mTORC2] dual inhibitor) [27, 28]; and the phosphatidylinositol 3-kinase (PI3K) inhibitors buparlisib (pan-PI3K inhibitor), taselisib (PI3K p110β-sparing inhibitor), and alpelisib (PI3K p110α-specific inhibitor) [29,30,31,32].
Growth factor receptor signaling and the PI3K, mTOR, MAPK, ER, and CDK4/6 pathways in ER+ breast cancer. Akt protein kinase B, CoA coenzyme A, CoR coenzyme R, CDK4/6 cyclin-dependent kinase 4/6, E2F transcription factor E2F, eIF4B eukaryotic translation initiation factor 4B, ER estrogen receptor, ER+ estrogen receptor-positive, G growth, IRS1 insulin receptor substrate 1, MAPK mitogen-activated protein kinase, MEK methyl ethyl ketone, mTOR mammalian target of rapamycin, mTORC1 mammalian target of rapamycin complex 1, mTORC2 mammalian target of rapamycin complex 2, PI3K phosphatidylinositol 3-kinase, PI(3)P phosphatidylinositol 3-phosphate, PIP2 phosphatidylinositol (4,5)-bisphosphate, PIP3 phosphatidylinositol (3,4,5)-trisphosphate, PTEN phosphatase and tensin homolog, RAF rapidly accelerated fibrosarcoma, RB retinoblastoma protein, S synthesis, S6K S6 kinase, TF transcription factor
2 Materials and Methods
We searched PubMed, oncology congresses, and ClinicalTrials.gov for trials investigating targeted agents plus fulvestrant in second-line HR+ ABC. The available efficacy and safety data in these study populations were then reviewed. All authors contributed to the writing of the manuscript, approved the final version, and were responsible for the decision to submit the manuscript for publication. Data sharing was not applicable to this article as no datasets were generated or analyzed.
3 Results
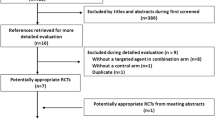
3.1 Summary of Search Results
Twelve key studies were selected for discussion in this review, including three randomized trials evaluating CDK4/6 inhibitors plus fulvestrant and six randomized trials evaluating PI3K/mTOR inhibitors plus fulvestrant. We also include additional trials of targeted combinations with fulvestrant, incorporating epidermal growth factor receptors, androgen receptor (AR), or the bromodomain and extra-terminal family of proteins (Table 1) [19, 25,26,27,28,29,30,31,32,33,34,35,36,37,38].
3.2 CDK4/6 Inhibition Plus Fulvestrant
CDK4/6 plays a key role in cell cycle progression, and its deregulation is a common feature of HR+ breast cancer [19, 39, 40]. ET-naïve and -resistant preclinical breast cancer cell lines are sensitive to CDK4/6 inhibition, and synergy is seen when CDK4/6 inhibitors are combined with ET [41,42,43]. Inhibition of CDK4/6 may overcome resistance to ET, as well as enhancing the efficacy of ET in patients with HR+, human epidermal growth factor receptor 2-negative (HER2−) ABC [19, 25, 26]. Three CDK4/6 inhibitors are currently approved for the treatment of ABC: palbociclib, ribociclib, and abemaciclib. Palbociclib, ribociclib, and abemaciclib are approved for combination therapy with an AI in the first-line ABC setting, based on positive study results [11, 44,45,46,47,48]. Palbociclib and abemaciclib are approved for combination therapy with fulvestrant in the second-line ABC setting [45, 47], with abemaciclib also being approved as a monotherapy after ET and prior chemotherapy for ABC [47].
3.2.1 PALOMA-3
PALOMA-3 was a multicenter, randomized, double-blind, placebo-controlled, phase 3 trial (NCT01942135) investigating the efficacy and safety of palbociclib (125 mg once daily [QD], days 1–21 of each 28-day cycle) plus fulvestrant (500 mg, per label) in women with HR+, HER2− ABC who had relapsed or progressed on prior ET [19, 49]. Relapse or progression was defined as that occurring on/after ET with an AI for postmenopausal women or tamoxifen for premenopausal or perimenopausal women (during or within 1 month after treatment in the advanced setting, or during or within 12 months of completing adjuvant therapy). One previous line of chemotherapy was allowed for advanced disease. The primary endpoint was investigator-assessed PFS according to Response Evaluation Criteria in Solid Tumors (RECIST; v1.1), and secondary endpoints included tumor tissue biomarkers (e.g., PIK3CA mutations) and safety.
A total of 521 patients were randomized 2:1 to receive palbociclib plus fulvestrant (n = 347) or placebo plus fulvestrant (n = 174). With regard to most recent treatment, these patients had received either adjuvant therapy (21% and 23% respectively) or treatment for advanced or metastatic breast cancer (79% and 76% respectively). Palbociclib plus fulvestrant was associated with a significant improvement in PFS vs placebo plus fulvestrant (9.5 vs 4.6 months; HR 0.46 [95% CI 0.36–0.59]; P < 0.0001). This improvement in PFS for palbociclib plus fulvestrant was observed in patients treated in the first-line advanced setting — patients who received neoadjuvant or adjuvant therapy only but no previous systemic therapy for metastatic breast cancer (MBC; 9.5 vs 5.4 months; HR 0.55 [95% CI 0.32–0.92]; P = 0.02) — and in patients treated in the second-line advanced setting (patients who received at least one previous systemic therapy for MBC; 9.9 vs 4.2 months; HR 0.43 [95% CI 0.33–0.57]; P < 0.0001). Palbociclib plus fulvestrant also exhibited a manageable safety profile [19]. Neither PIK3CA status, hormone receptor expression level, nor mutation status of the ER gene, ESR1, significantly affected treatment response [19, 50]. All-grade and grade 3/4 neutropenia occurred more frequently in patients treated with palbociclib plus fulvestrant (81% and 65% respectively) than with placebo plus fulvestrant (3% and 1% of patients respectively) [19], which can be managed with palbociclib dose reductions and delays [51]. The overall mean index score from the European Quality of Life Five Dimensions self-administered patient-reported outcomes questionnaire was significantly higher in patients treated with palbociclib plus fulvestrant compared with those treated with fulvestrant alone (0.74 vs 0.69; P < 0.05) [52].
3.2.2 MONALEESA-3
MONALEESA-3 was a randomized, double-blind, placebo-controlled, phase 3 trial (NCT02422615) of ribociclib (600 mg QD, days 1–21 of each 28-day cycle) plus fulvestrant (500 mg, per label) for men and postmenopausal women with HR+, HER2− ABC who had received 0 or 1 line of prior ET [25]. Eligible patients included those with newly diagnosed, treatment-naïve, relapsed breast cancer that had progressed at any time during or following neoadjuvant ET with no prior treatment for metastatic disease, relapsed breast cancer occurring > 12 months post-adjuvant ET and having subsequently progressed after one line of ET for metastatic disease, or newly diagnosed ABC that had progressed after one line of ET. Prior chemotherapy (except neoadjuvant chemotherapy) was not permitted in this study. The primary endpoint was centrally assessed PFS according to RECIST v1.1, and secondary endpoints included centrally assessed OS (RECIST v1.1) and overall response rate (ORR) [25].
A total of 726 patients were randomized 2:1 to receive ribociclib plus fulvestrant (n = 484) or placebo plus fulvestrant (n = 242). Patients received the study treatment either as first-line (49% ribociclib arm, 53% placebo arm; patients who had no [neo]adjuvant endocrine therapy or relapsed > 12 months after [neo]adjuvant endocrine therapy and were treatment-naïve for advanced disease) or second-line (49% ribociclib arm, 45% placebo arm; patients who had received one line of endocrine therapy for advanced disease or relapsed ≤ 12 months from completion of [neo]adjuvant endocrine therapy) treatment [25, 53]. Ribociclib plus fulvestrant significantly improved PFS vs placebo plus fulvestrant (20.5 vs 12.8 months; HR 0.59 [95% CI 0.48–0.73]; P < 0.001), and improvement was consistent for first-line (HR 0.58; 95% CI 0.42–0.80) and second-line treatment (HR 0.57; 95% CI 0.43–0.74) for advanced disease [25].
Most AEs with ribociclib plus fulvestrant were mild or moderate in severity. Grade 3 AEs reported in ≥ 10% of patients in either arm (ribociclib plus fulvestrant vs placebo plus fulvestrant) were neutropenia (47% vs 0) and leukopenia (13% vs 0), while neutropenia was the only grade 4 AE occurring in ≥ 5% of patients (7% vs 0) [25]. AE-related treatment discontinuations were rare (8% ribociclib plus fulvestrant vs 4% placebo plus fulvestrant), supporting the manageable safety profile of ribociclib-based combinations [25, 53].
3.2.3 MONARCH-2
MONARCH-2 was a randomized, double-blind, placebo-controlled, phase 3 trial (NCT02107703) of abemaciclib plus fulvestrant in women with HR+, HER2– ABC who progressed on prior ET [26]. Patients were randomized 2:1 to receive abemaciclib (150 mg every 12 h on a continuous schedule [cont]) plus fulvestrant (500 mg, per label) or placebo plus fulvestrant, stratified by metastatic site (visceral, bone only, or other) and resistance to prior ET (primary vs secondary). Patients were required to have disease that progressed while receiving neoadjuvant or adjuvant ET, up to 12 months after adjuvant ET, or while receiving ET for ABC. Patients must not have received more than one ET or any prior chemotherapy for ABC. The primary endpoint was investigator-assessed PFS, with secondary endpoints of ORR and additional efficacy and safety endpoints.
A total of 669 patients were randomized to abemaciclib plus fulvestrant (n = 446) or placebo plus fulvestrant (n = 223). Of these patients, 25% had primary ET resistance, and the majority (59%) had received their most recent ET in the neoadjuvant or adjuvant setting. A significant improvement in PFS with abemaciclib plus fulvestrant vs placebo plus fulvestrant was observed (median PFS 16.4 vs 9.3 months respectively; HR 0.553 [95% CI 0.449–0.681]; P < 0.001 by log-rank test) [26]. In patients with measurable disease, the ORR for patients treated with abemaciclib plus fulvestrant was 48.1% vs 21.3% for those treated with placebo plus fulvestrant [26]. The most frequent treatment-emergent AEs in patients treated with abemaciclib plus fulvestrant vs placebo plus fulvestrant respectively, were diarrhea (86.4% vs 24.7%), neutropenia (46.0% vs 4.0%), nausea (45.1% vs 22.9%), and fatigue (39.9% vs 26.9%) [26].
In summary, the addition of a CDK4/6 inhibitor to fulvestrant has shown excellent clinical efficacy in patients who have progressed on ET, with a manageable side-effect profile. The U.S. Food and Drug Administration has approved fulvestrant in combination with palbociclib or abemaciclib in women with disease progression following ET. As regulatory approval for second-line therapy with fulvestrant in combination with ribociclib is possible in the near future, physicians will face a three-way choice of which CDK4/6 inhibitor to combine with fulvestrant. Based on currently available data, such decisions may be influenced primarily by previous treatment regimens, respective side-effect profiles, and/or costs.
3.3 mTOR Inhibition Plus Fulvestrant
A well-studied mechanism of endocrine resistance is aberrant signaling through the PI3K–protein kinase B (Akt)–mTOR signaling pathway [54, 55]. mTOR is a serine/threonine protein kinase which is located both upstream and downstream of the PI3K pathway and regulates cell growth, proliferation, and survival via mTORC1 and mTORC2 [56,57,58]. Preclinical studies have shown that Akt can activate the ER pathway independently of estrogen availability and that mTOR inhibitors in combination with ET can overcome endocrine resistance [59]. Sensitivity to ET may be restored by treatment with mTOR inhibitors such as everolimus [59].
The mTORC1 inhibitor everolimus is currently approved in combination with exemestane for treatment of patients with HR+, HER2− ABC after failure on letrozole or anastrozole therapy [60]. Approval was based on data from the phase 3 BOLERO-2 clinical trial, which reported improvements in PFS of 7.8 vs 3.2 months by investigator review (HR 0.45 [95% CI 0.38–0.54]; log-rank P < 0.001) in the everolimus plus exemestane arm vs the placebo plus exemestane arm [61]. A phase 2 trial is ongoing for the mTORC1 and mTORC2 dual inhibitor vistusertib [28].
3.3.1 PrE0102
PrE0102 was a randomized, placebo-controlled, phase 2 trial (NCT01797120) of everolimus (10 mg daily) plus fulvestrant (500 mg, per label) in postmenopausal women with HR+, HER2− MBC with relapse during adjuvant AI therapy or progression after one or more AIs for ABC [27]. Patients could also have received up to one prior chemotherapy regimen for metastases. A total of 131 patients were randomized 1:1 to receive everolimus plus fulvestrant or placebo plus fulvestrant. Treatment arms were balanced for stratification factors, including prior chemotherapy for metastasis (18%). The primary endpoint of PFS was met, with a significant improvement in PFS with everolimus plus fulvestrant vs placebo plus fulvestrant (median 10.3 vs 5.1 months respectively; HR 0.61 [95% CI 0.40–0.92]; stratified log-rank P = 0.02) [27]. Treatment-related grade 3 AEs occurred more frequently with everolimus vs the placebo arm, including (≥ 5% of patients) stomatitis (oral mucositis; 11% vs 0), fatigue (6% vs 5%), and pneumonitis (6% vs 0) [27]. There were no grade 4 AEs in the everolimus arm and one (elevated aspartate aminotransferase [AST]) in the placebo arm [27]. It should be noted that prophylactic corticosteroid mouthwash was not used in this trial but has been shown to reduce the incidence and severity of stomatitis [62]. The addition of everolimus to fulvestrant had a manageable toxicity profile and showed clinical efficacy, suggesting this regimen could be a possible option for second-line therapy and beyond.
3.3.2 MANTA
MANTA is an ongoing, investigator-led, randomized, open-label, phase 2 trial (NCT02216786) of fulvestrant plus vistusertib or everolimus in postmenopausal women with ER-positive (ER+) ABC [28]. Patients were randomized 2:3:3:2 to receive either fulvestrant alone (500 mg, per label), continuous vistusertib (50 mg twice daily [BID] cont) plus fulvestrant, intermittent vistusertib (125 mg BID 2 days on, 5 days off, intermittent [int]) plus fulvestrant, or everolimus (10 mg QD) plus fulvestrant. Randomization was stratified by the presence or absence of measurable disease and sensitivity or resistance to ET [33]. Patients were required to have disease recurrence on or within 12 months of completing adjuvant therapy with an AI, or progression within 1 month of completing AI therapy for locally advanced or metastatic disease. The primary endpoint was investigator-assessed PFS by RECIST [33].
At the interim analysis, median PFS was: fulvestrant, 4.6 months (95% CI 3.4–6.9; n = 66); vistusertib (cont) plus fulvestrant, 7.5 months (95% CI 5.6–9.4; n = 101); vistusertib (int) plus fulvestrant, 7.6 months (95% CI 5.5–9.6; n = 95); and everolimus plus fulvestrant, 12.2 months (95% CI 7.5–14.3; n = 64) [28]. No significant difference in PFS was observed between the vistusertib (cont) plus fulvestrant arm vs fulvestrant arm (HR 0.87 [95% CI 0.62–1.23]; log-rank P = 0.42), vistusertib (int) plus fulvestrant arm vs fulvestrant arm (HR 0.78 [95% CI 0.55–1.12]; log-rank P = 0.16), or vistusertib (cont) plus fulvestrant arm vs vistusertib (int) plus fulvestrant arm (HR 1.11 [95% CI 0.81–1.52]; log-rank P = 0.52) [28]. In contrast, PFS was significantly longer in the everolimus plus fulvestrant arm vs vistusertib (cont) plus fulvestrant arm (HR 0.64 [95% CI 0.45–0.91]; log-rank P = 0.01) and in the everolimus plus fulvestrant arm vs fulvestrant arm (HR 0.64 [95% CI 0.43–0.94]; log-rank P = 0.02) [28]. The estimated date of final data collection for primary outcome measure is June 2019 [33].
3.4 PI3K Inhibition Plus Fulvestrant
PI3Ks are heterodimers consisting of a p110 catalytic subunit and a p85 regulatory subunit. There are four catalytic isoforms encoded by their respective genes: p110α (PIK3CA), p110β (PIK3CB), p110δ (PIK3CD), and p110γ (PIK3CG) [63, 64]. The PI3K pathway is one of the most frequently activated in breast cancer [65, 66]. Activating PIK3CA mutations are frequently observed in HR+ breast cancer and associated with disease progression and resistance to ET [55, 56, 65,66,67,68,69]. In early clinical studies, PI3K inhibitors demonstrated limited single-agent activity; however, combining a PI3K inhibitor with fulvestrant has been shown to suppress hormone-independent growth in vitro and induce marked tumor regressions in vivo [66, 68]. Phase 3 data are available for the pan-PI3K inhibitor buparlisib and the PI3K p110β-sparing inhibitor taselisib; a phase 3 trial is ongoing for the PI3K p110α-specific inhibitor alpelisib [29,30,31,32].
3.4.1 BELLE-2
BELLE-2 was a multicenter, randomized, double-blind, placebo-controlled, phase 3 trial (NCT01610284) of buparlisib (100 mg QD) plus fulvestrant (500 mg, per label) in postmenopausal women with HR+, HER2− ABC who progressed on or after AI therapy [29]. Eligible patients progressed within 12 months of receiving AI therapy in the adjuvant setting, or within 1 month for metastatic/advanced disease. Patients could have received any number of lines of ET before or after being defined as refractory to AI therapy. Patients could have received other anticancer therapies before or after progression on an AI therapy, and up to one prior line of chemotherapy for advanced disease. Randomization was stratified by PI3K activation status (activated status included PIK3CA mutations or loss of PTEN expression) and visceral disease status. The co-primary endpoints were investigator-assessed PFS by RECIST v1.1 in the full population, in patients with known (activated/non-activated) PI3K pathway tumor status, and in patients with activated PI3K pathway tumor status.
A total of 1147 patients were randomized to receive either buparlisib plus fulvestrant (n = 576) or placebo plus fulvestrant (n = 571); 73% and 75% respectively of these patients received prior ET in the metastatic setting, and 24% and 31% respectively received prior chemotherapy in the metastatic setting. BELLE-2 met one of its co-primary endpoints: the median PFS for patients in the full population (N = 1147) treated with buparlisib plus fulvestrant was 6.9 months vs 5.0 months for patients treated with placebo plus fulvestrant (HR 0.78 [95% CI 0.67–0.89]; one-sided P = 0.0002). However, the prespecified statistical significance for PFS was not reached in patients with PI3K pathway-activated tumors (n = 372), where the median PFS for buparlisib plus fulvestrant vs placebo plus fulvestrant was 6.8 vs 4.0 months respectively (HR 0.76 [95% CI 0.60–0.97]; one-sided P = 0.014 at a one-sided α = 0.01 level of significance) [29]. In patients with ctDNA PIK3CA mutations (n = 200), a clinically meaningful improvement in PFS was observed in patients treated with buparlisib plus fulvestrant vs those with placebo plus fulvestrant (median 7.0 vs 3.2 months respectively; stratified HR 0.58 [95% CI 0.41–0.82]; nominal one-sided P = 0.001), but not in those with wild-type PIK3CA (median 6.8 vs 6.8 months respectively; stratified HR 1.02 [95% CI 0.79–1.30]; nominal one-sided P = 0.557) [29]. The median duration of exposure to buparlisib was 1.9 months and to placebo was 4.4 months, and was limited by the increased rates of AEs leading to dose interruptions (50.6% vs 14.2%), reductions (45.0% vs 5.6%), and discontinuations (38.7% vs 4.9%) for buparlisib vs placebo. Of the AEs leading to discontinuation in the buparlisib arm, the most common were elevated alanine aminotransferase (ALT; 10.1%), elevated AST (7.0%), hyperglycemia (3.3%), depression (3.0%), and rash (2.8%) [29].
3.4.2 BELLE-3
BELLE-3 was a randomized, double-blind, placebo-controlled, phase 3 trial (NCT01633060) of buparlisib (100 mg QD) plus fulvestrant (500 mg, per label) in postmenopausal women with HR+, HER2− ABC who received prior AI therapy and progressed on or within 30 days of combination therapy with ET plus mTOR inhibitor treatment [30]. Patients may have received up to one chemotherapy regimen for ABC. The primary endpoint was investigator-assessed PFS by RECIST v1.1, the key secondary endpoint was OS, and other secondary endpoints included: ORR and clinical benefit rate (CBR) in the full population; PFS, OS, ORR, and CBR based on ctDNA PIK3CA status; and overall safety, pharmacokinetics, and quality of life.
A total of 432 patients were randomized 2:1 to receive buparlisib plus fulvestrant or placebo plus fulvestrant. PFS was significantly prolonged with the addition of buparlisib to fulvestrant (median 3.9 vs 1.8 months respectively; HR 0.67 [95% CI 0.53–0.84]; one-sided P < 0.001) [30]. When PIK3CA mutation status was determined by ctDNA (n = 348), PFS benefit was higher in patients with PIK3CA mutations who were treated with buparlisib plus fulvestrant vs placebo plus fulvestrant (median 4.2 vs 1.6 months respectively; HR 0.46 [95% CI 0.29–0.73]) than in those with wild-type PIK3CA (median 3.9 vs 2.7 months respectively; HR 0.73 [95% CI 0.53–1.00]) [30]. Similar results were observed when PIK3CA mutation status was determined using tumor tissue [30]. The rate of adverse events was higher in the buparlisib arm; the most frequent adverse events in the buparlisib plus fulvestrant and placebo plus fulvestrant arms, respectively, were elevated ALT (38.9% vs 7.1%), elevated AST (37.2% vs 10%), hyperglycemia (35.8% vs 2.9%), nausea (34.4% vs 17.9%), diarrhea (26.0% vs 9.3%), and fatigue (23.3% vs 18.6%) [30]. Due to the toxicity associated with the combination of buparlisib and fulvestrant, no further studies are being pursued [29].
3.4.3 SANDPIPER
SANDPIPER was a randomized, double-blind, placebo-controlled, phase 3 trial (NCT02340221) of the PI3K p110β-sparing inhibitor taselisib (4 mg QD) plus fulvestrant (500 mg, per label) in postmenopausal women with ER+, HER2− locally advanced or metastatic breast cancer with recurrence or progression during or after AI therapy, enriched for patients with PIK3CA-mutant tumors [32]. No more than one prior line of chemotherapy for ABC was allowed. Patients were randomized 2:1 to receive either taselisib plus fulvestrant or placebo plus fulvestrant, stratified by visceral disease, endocrine sensitivity, and geographic region. Patients with PIK3CA-mutant tumors were randomized separately from those with non-mutant tumors. The primary endpoint was investigator-assessed PFS in patients with PIK3CA-mutant tumors. Other endpoints included OS, ORR, CBR, duration of response, and safety [32].
Of 631 patients recruited, 516 with PIK3CA-mutant tumors were randomized 2:1 to receive taselisib plus fulvestrant (n = 340) or placebo plus fulvestrant (n = 176); these patients had received either adjuvant therapy (60% and 68% respectively), endocrine therapy for metastatic breast cancer (75% and 69% respectively), or tamoxifen (49% and 49% respectively) [32]. Taselisib plus fulvestrant significantly improved PFS vs placebo plus fulvestrant in patients with PIK3CA-mutant tumors (7.4 vs 5.4 months; HR 0.70 [95% CI 0.56–0.89]; P = 0.0037); ORR (28% vs 12%), CBR (52% vs 37%), and duration of response (8.7 vs 7.2 months) also favored taselisib plus fulvestrant vs placebo plus fulvestrant (OS data were immature) [32]. Grade ≥ 3 AEs were more frequent with taselisib plus fulvestrant (50%) vs placebo plus fulvestrant (16%); GI toxicities and hyperglycemia were the most frequent AEs with taselisib plus fulvestrant [32]. Treatment discontinuations due to AEs were frequent among patients treated with taselisib plus fulvestrant (17% vs 2% among patients treated with placebo plus taselisib); approximately 50% of AE-related taselisib discontinuations were due to GI toxicities, particularly diarrhea. With such a challenging toxicity profile, taselisib plus fulvestrant may have limited clinical benefit in this setting [32].
3.4.4 SOLAR-1
SOLAR-1 is an ongoing, randomized, double-blind, placebo-controlled, phase 3 trial (NCT02437318) of the PI3K p110α-specific inhibitor alpelisib plus fulvestrant in men and postmenopausal women with HR+, HER2− ABC progressing on or after any AI therapy (letrozole, anastrozole, or exemestane) [31]. Eligible patients can be newly diagnosed with progression after only one line of ET, or relapsed or progressed within 12 months of (neo)adjuvant ET with or without progression after only one subsequent line of ET [34]. Only (neo)adjuvant chemotherapy is allowed. Patients are randomly (1:1) assigned alpelisib (300 mg QD) plus fulvestrant (500 mg, per label) or placebo plus fulvestrant until disease progression or treatment discontinuation. Patients are stratified according to the presence of liver and/or lung metastases and prior use of CDK4/6 inhibitors. The primary endpoint of the study is investigator-assessed PFS by RECIST v1.1 in patients with known PIK3CA mutant status. OS is the key secondary endpoint, and other secondary endpoints include the association between PFS and baseline ctDNA PIK3CA status, ORR, CBR, and safety. The estimated date of final data collection for primary outcome measure is May 2018 [34].
3.5 Additional Targeted Combinations Plus Fulvestrant
3.5.1 Tyrosine Kinase Inhibition Plus Fulvestrant
HER2 mutations occur in approximately 2% of breast cancers, and preclinical models have suggested that neratinib, an irreversible HER2/epidermal growth factor receptor tyrosine kinase inhibitor, might be an effective treatment for patients with HER2-mutant breast cancer [35]. A non-randomized phase 2 trial (NCT01670877) of neratinib with or without fulvestrant in patients with metastatic HER2 non-amplified (HER2−) but HER2-mutant breast cancer is currently recruiting patients. Patients will be allocated to one of four treatment arms: 1) neratinib alone, 2) neratinib alone in ER− patients, 3) neratinib plus fulvestrant in fulvestrant-naïve ER+ patients, and 4) neratinib plus fulvestrant in fulvestrant-experienced ER+ patients [35, 36]. The neratinib single-agent arm of this study met its primary endpoint, with a CBR of 36% in a heavily pretreated patient population [35]. Given that most patients enrolled in the study had ER+ tumors, the combination of neratinib plus fulvestrant in this population will be of interest [35].
3.5.2 Androgen Receptor Inhibition Plus Fulvestrant
In breast cancers, androgen receptors are more widely expressed than estrogen-α receptors or progesterone receptors [70]. AR overexpression increases resistance to tamoxifen in both breast cancer cells in vitro and in xenograft models [71]. De-novo or acquired resistance to anti-estrogen therapies, therefore, may be due to tumor cells adapting from estrogen dependence to androgen dependence [71, 72].
Enzalutamide is an AR signaling inhibitor that impairs nuclear translocation and has no known agonistic activity at effective doses. As ARs are found in up to 90% of breast cancers and the AR signaling pathway is reported to have potential in mitigating resistance to anti-estrogen therapies, enzalutamide is a compelling candidate targeted agent for combination with fulvestrant for post-endocrine treatment of patients with HR+ ABC [73, 74]. A phase 2 trial (NCT02953860) is currently enrolling women with HR+, HER2− ABC to evaluate the safety and tolerability of enzalutamide (160 mg QD) plus fulvestrant (500 mg, per label). Patients include all those who are eligible for fulvestrant; exclusion criteria include prior treatment with anti-androgen therapy and systemic estrogens or androgens within 14 days prior to study treatment [37]. The primary endpoint of this study is CBR, and secondary endpoints include AR expression in breast tissue biopsies, PFS, ORR, and AR signaling in breast cancer tissue [37].
3.5.3 Bromodomain and Extra-Terminal Inhibition Plus Fulvestrant
The bromodomain (BRD) and extra-terminal (BET) family comprises BRD2, 3, and 4, and bromodomain testis-associated protein, all of which are functionally linked to pathways important in cellular viability and cancer development [75]. BRD4, the best characterized BET protein, is critical for cell cycle progression and promotes ESR1 transcription [75, 76] which, in turn, contributes to tamoxifen resistance [77]. Inhibition of BET proteins selectively suppresses key oncogenic drivers [78, 79] and may be an attractive therapeutic target for ER+ breast cancer [80].
GS-5829 is an oral BET inhibitor currently being investigated in combination with fulvestrant (500 mg, per label) or exemestane (25 mg QD) in patients with ER+, HER2− ABC in a phase 1b/2 study (NCT02983604). The primary outcome measure of the phase 1 dose escalation is the incidence of dose-limiting toxicities at each dose level of GS-5829. For the phase 2 part of the study, the primary outcome measure is PFS. Secondary endpoints include pharmacokinetics of GS-5829, safety, ORR, CBR, and OS. Recruitment is currently ongoing [38].
4 Discussion
This literature review demonstrates that fulvestrant is an appropriate and well-tolerated treatment backbone for combining with targeted agents to improve PFS in patients with HR+ ABC in the second-line setting. Across the studies reviewed, the addition of targeted therapy to fulvestrant resulted in clinically meaningful improvements in PFS compared with fulvestrant alone. In these studies, outcomes with fulvestrant alone in the second-line setting were usually poor, with median PFS typically < 6 months [19, 27, 29, 30]. Fulvestrant was generally well tolerated, and the addition of targeted therapy to fulvestrant did not appear to have cumulative effects that increased incidences of individual AEs. When combined with fulvestrant, the safety profiles of the approved CDK4/6 inhibitors appear largely predictable and consistent with previous findings. Safety was generally comparable across the three agents, with the notable exception of increased GI AEs reported with abemaciclib (in MONARCH-2, diarrhea was the most frequent serious AE possibly related to abemaciclib plus fulvestrant) [19, 25, 26]. Although high rates of grade 3/4 neutropenia were reported with palbociclib plus fulvestrant in PALOMA-3 [19] and ribociclib plus fulvestrant in MONALEESA-3 [25], neutropenia can be well managed with recommended dose reductions and delays [6]. For everolimus plus fulvestrant, increased rates of hyperglycemia and stomatitis were observed compared with fulvestrant alone [27]. These particular AEs are known side-effects of everolimus and can be resolved effectively using dose modification/interruption of everolimus and, in the case of stomatitis, prevented by the use of dexamethasone mouthwash [62]. For buparlisib plus fulvestrant, increased liver toxicity and hyperglycemia were observed compared with fulvestrant alone, as well as increased mood disorders (anxiety and depression) [29, 30]. These toxicities associated with pan-PI3K inhibition represented a clinically relevant challenge and, consequently, no further clinical trials are planned for buparlisib in the treatment of breast cancer, despite preliminary indications that PI3K inhibitors might be efficacious when combined with fulvestrant in this setting. Despite being β-sparing, taselisib still targets multiple isoforms of PI3K, and its combination with fulvestrant in the phase 3 SANDPIPER trial resulted in a challenging safety profile that included GI toxicities, hyperglycemia, and enough treatment discontinuations to have potentially limited its clinical benefit [32]. Clinical data for alpelisib remain immature, but early data indicate a manageable safety profile [81]. Data from the phase 3 SOLAR-1 trial of alpelisib are yet to be reported.
When considering the sequence and selection of an appropriate targeted therapy for combination with fulvestrant in the second-line setting, it should be noted that the results from different trials cannot be compared directly. This is due to differences with regard to permitted prior ET and whether patients were treated in the second-line setting only, or in both the first- and second-line settings (and beyond). For example, PALOMA-3 specified the type of ET by menopausal status and allowed one previous line of chemotherapy for advanced disease [19], MONARCH-2 did not require any specific type of prior ET and did not allow previous chemotherapy for metastatic disease [26], and MONALEESA-3 allowed treatment-naïve patients as well as patients who had received up to one previous line of endocrine therapy for advanced disease [25]. Therefore, treatment decisions should consider the first-line treatment that individual patients received as well as the current mutation status of the tumor. For example, many patients with ER+ ABC may receive an AI plus CDK4/6 inhibitor in the first-line setting and, therefore, alternative targeted therapeutic options might be required in subsequent lines. The clinical efficacy of fulvestrant with CDK4/6 inhibition after progression on a first-line CDK4/6 inhibitor is unknown and the ideal sequence of therapy requires further investigation. In this regard, the BYLieve study (NCT03056755) is investigating treatment with the PI3K inhibitor alpelisib plus ET in patients with HR+, HER2− ABC who progressed on or after CDK4/6 treatment with an AI or fulvestrant [82]. A key inclusion criterion of the BELLE-3 study of buparlisib plus fulvestrant was progression on an mTOR inhibitor, the rationale being that mTORC1 inhibition elicits Akt phosphorylation (feedback activation), which PI3K inhibitors abrogate or attenuate [30]. This rationale appears to be supported by the fact that PFS was significantly prolonged in patients treated with buparlisib plus fulvestrant compared with those treated with placebo plus fulvestrant [30].
Multiple studies have analyzed the effects of tumor mutation status on PFS [29,30,31]. In PALOMA-3, treatment with palbociclib plus fulvestrant resulted in a numerically longer median PFS in patients without detectable PIK3CA mutations vs those with PIK3CA mutations, although this difference was not significant [19]. In the BELLE-2 and BELLE-3 studies, PFS was significantly prolonged in patients with ctDNA PIK3CA-mutant status who were treated with buparlisib plus fulvestrant vs placebo plus fulvestrant, but not in those with wild-type PIK3CA [29, 30]. Across the studies reviewed, PIK3CA mutation status appears generally to be an indicator of poor response to fulvestrant alone and of greater benefit from the addition of a PI3K inhibitor to fulvestrant. Further, the addition of fulvestrant to the tyrosine kinase inhibitor neratinib is being investigated in patients with HER2 mutations [36].
5 Conclusions
Due to adaptive cross-talk between ER and growth factor receptor signaling pathways, the addition of fulvestrant to small-molecule inhibitors targeting various activated pathways in ER+ ABC shows synergy and greater benefit than either therapy alone. Data from ongoing trials of CDK4/6 inhibitors, PI3K inhibitors, and other targeted therapies (e.g., tyrosine kinase inhibitors and AR inhibitors) will help identify further therapeutic options for fulvestrant-based treatment combinations in the second-line setting.
Change history
08 December 2018
The article Fulvestrant-Based Combination Therapy for Second-Line Treatment of Hormone Receptor-Positive Advanced Breast Cancer, written by Sarah Sammons, Noah S. Kornblum and Kimberly L. Blackwell, was originally published electronically on the publisher’s internet portal (currently SpringerLink).
References
Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Allen C, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA Oncol. 2017;3:524–48.
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;62:87–108.
Kümler I, Knoop AS, Jessing CA, Ejlertsen B, Nielsen DL. Review of hormone-based treatments in postmenopausal patients with advanced breast cancer focusing on aromatase inhibitors and fulvestrant. ESMO Open. 2016;1:e000062.
Howlader N, Altekruse SF, Li CI, et al. US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst. 2014;106(5): https://doi.org/10.1093/jnci/dju055.
Huang HJ, Neven P, Drijkoningen M, et al. Association between tumour characteristics and HER-2/neu by immunohistochemistry in 1362 women with primary operable breast cancer. J Clin Pathol. 2005;58:611–6.
Rugo H, Rumble R, Macrae E, et al. Endocrine therapy for hormone receptor–positive metastatic breast cancer: American Society of Clinical Oncology guideline. J Clin Oncol. 2016;34:3069–103.
Cardoso F, Costa A, Senkus E, et al. 3rd ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 3). Ann Oncol. 2017;28:16–33.
Ciruelos E, Pascual T, Arroyo Vozmediano ML, et al. The therapeutic role of fulvestrant in the management of patients with hormone receptor-positive breast cancer. Breast. 2014;23:201–8.
Abdel-Razeq H. Current frontline endocrine treatment options for women with hormone receptor-positive, human epidermal growth factor receptor 2 (HER2)-negative advanced-stage breast cancer. Hematol Oncol Stem Cell Ther. 2018; https://doi.org/10.1016/j.hemonc.2018.04.002.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology (NCCN guidelines). Breast cancer. Version 4.2017. https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf; 2017 Accessed February 1, 2018.
Finn RS, Martin M, Rugo HS, et al. Palbociclib and letrozole in advanced breast cancer. N Engl J Med. 2016;375:1925–36.
Hortobagyi C, Stemmer S, Burris H, et al. Updated results from MONALEESA-2, a phase 3 trial of first-line ribociclib + letrozole in hormone receptor-positive (HR+), HER2-negative (HER2–), advanced breast cancer (ABC) [abstract]. J Clin Oncol. 2017;35(15 suppl):1038.
Faslodex® (fulvestrant) injection [prescribing information]: AstraZeneca Pharmaceuticals; 2017.
Robertson JF, Bondarenko IM, Trishkina E, et al. Fulvestrant 500 mg versus anastrozole 1 mg for hormone receptor-positive advanced breast cancer (FALCON): an international, randomised, double-blind, phase 3 trial. Lancet. 2016;388:2997–3005.
Ali S, Rasool M, Chaoudhry H, et al. Molecular mechanisms and mode of tamoxifen resistance in breast cancer. Bioinformation. 2016;12:135–9.
Osborne CK, Schiff R. Mechanisms of endocrine resistance in breast cancer. Annu Rev Med. 2011;62:233–47.
Glück S. Consequences of the convergence of multiple alternate pathways on the estrogen receptor in the treatment of metastatic breast cancer. Clin Breast Cancer. 2017;17:79–90.
Di Leo A, Jerusalem G, Petruzelka L, et al. Results of the CONFIRM phase III trial comparing fulvestrant 250 mg with fulvestrant 500 mg in postmenopausal women with estrogen receptor–positive advanced breast cancer. J Clin Oncol. 2010;28:4594–600.
Cristofanilli M, Turner NC, Bondarenko I, et al. Fulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2-negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): final analysis of the multicentre, double-blind, phase 3 randomised controlled trial. Lancet Oncol. 2016;17:425–39.
Reinert T, Barrios CH. Overall survival and progression-free survival with endocrine therapy for hormone receptor-positive, HER2-negative advanced breast cancer: review. Ther Adv Med Oncol. 2017;9:693–709.
Jeselsohn R, Buchwalter G, De Angelis C, Brown M, Schiff R. ESR1 mutations—a mechanism for acquired endocrine resistance in breast cancer. Nat Rev Clin Oncol. 2015;12:573–83.
Johnston SR. New strategies in estrogen receptor-positive breast cancer. Clin Cancer Res. 2010;16:1979–87.
Selli C, Dixon J, Sims A. Accurate prediction of response to endocrine therapy in breast cancer patients: current and future biomarkers. Breast Cancer Res. 2016;18:118.
Ma C, Reinert T, Chmielewska I, Ellis M. Mechanisms of aromatase inhibitor resistance. Nat Rev Cancer. 2015;15:261–75.
Slamon DJ, Neven P, Chia S, et al. Phase III randomized study of ribociclib and fulvestrant in hormone receptor-positive, human epidermal growth factor receptor 2-negative advanced breast cancer: MONALEESA-3. J Clin Oncol. 2018; https://doi.org/10.1200/JCO.2018.78.9909.
Sledge GW, Toi M, Neven P, et al. MONARCH 2: Abemaciclib in combination with fulvestrant in women with HR+/HER2− advanced breast cancer who had progressed while receiving endocrine therapy. J Clin Oncol. 2017;35:2875–84.
Kornblum N, Zhao F, Manola J, et al. Randomized phase II trial of fulvestrant plus everolimus or placebo in postmenopausal women with hormone receptor-positive, human epidermal growth factor receptor 2-negative metastatic breast cancer resistant to aromatase inhibitor therapy: results of PrE0102. J Clin Oncol. 2018;36:1556–63.
Schmid P, Ferreira M, Dubey S, et al. MANTA: A randomized phase II study of fulvestrant in combination with the dual mTOR inhibitor AZD2014 or everolimus or fulvestrant alone in estrogen receptor-positive advanced or metastatic breast cancer [abstract]. San Antonio Breast Cancer Symposium. 2017; GS2–07.
Baselga J, Im SA, Iwata H, et al. Buparlisib plus fulvestrant versus placebo plus fulvestrant in postmenopausal, hormone receptor-positive, HER2-negative, advanced breast cancer (BELLE-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2017;18:904–16.
Di Leo A, Johnston S, Lee KS, et al. Buparlisib plus fulvestrant in postmenopausal women with hormone-receptor-positive, HER2-negative, advanced breast cancer progressing on or after mTOR inhibition (BELLE-3): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2018;19:87–100.
Rugo H, Andre F, Rubovszky G, et al. A phase 3 study of alpelisib (ALP) plus fulvestrant (FUL) in men and postmenopausal women with hormone receptor-positive (HR+), human epidermal growth factor receptor 2-negative (HER2-) ABC progressing on or after aromatase inhibitor (AI) therapy: SOLAR-1 [abstract]. J Clin Oncol. 2017;35(15 suppl):TPS1111.
Baselga J, Dent S, Cortés J, et al. Phase III study of taselisib (GDC-0032) + fulvestrant (FULV) in patients (pts) with estrogen receptor (ER)-positive, PIK3CA-mutant (MUT), locally advanced or metastatic breast cancer (MBC): primary analysis from SANDPIPER. J Clin Oncol. 2018;36(18 suppl):LBA1006.
ClinicalTrials.gov. A randomized study of AZD2014 in combination with fulvestrant in metastatic or advanced breast cancer (MANTA). https://clinicaltrials.gov/ct2/show/NCT02216786; 2017 Accessed February 1, 2018.
ClinicalTrials.gov. Study assessing the efficacy and safety of alpelisib plus fulvestrant in men and postmenopausal women with advanced breast cancer which progressed on or after aromatase inhibitor treatment. (SOLAR-1). https://clinicaltrials.gov/ct2/show/NCT02437318; 2018 Accessed February 1, 2018.
Ma C, Bose R, Gao F, et al. Phase II trial of neratinib for HER2 mutated, nonamplified metastatic breast cancer (HER2mut MBC) [abstract]. J Clin Oncol. 2016;34(15 suppl):516.
ClinicalTrials.gov. Neratinib +/− fulvestrant in metastatic HER2 non-amplified but HER2 mutant breast cancer. https://clinicaltrials.gov/ct2/show/NCT01670877; 2018 Accessed February 1, 2018.
ClinicalTrials.gov. Fulvestrant plus enzalutamide in ER+/Her2- advanced breast cancer. https://clinicaltrials.gov/ct2/show/NCT02953860; 2018 Accessed February 1, 2018.
ClinicalTrials.gov. GS-5829 in combination with fulvestrant or exemestane in women with advanced estrogen receptor positive, HER2 negative-breast cancer. https://clinicaltrials.gov/ct2/show/NCT02983604; 2018 Accessed February 1, 2018.
Dean JL, McClendon AK, Hickey TE, et al. Therapeutic response to CDK4/6 inhibition in breast cancer defined by ex vivo analyses of human tumors. Cell Cycle. 2012;11:2756–61.
Spring L, Bardia A, Modi S. Targeting the cyclin D-cyclin-dependent kinase (CDK) 4/6-retinoblastoma pathway with selective CDK 4/6 inhibitors in hormone receptor-positive breast cancer: rationale, current status, and future directions. Discov Med. 2016;21:65–74.
Finn RS, Dering J, Conklin D, et al. PD 0332991, a selective cyclin D kinase 4/6 inhibitor, preferentially inhibits proliferation of luminal estrogen receptor-positive human breast cancer cell lines in vitro. Breast Cancer Res. 2009;11:R77.
Dean JL, Thangavel C, McClendon AK, Reed CA, Knudsen ES. Therapeutic CDK4/6 inhibition in breast cancer: key mechanisms of response and failure. Oncogene. 2010;29:4018–32.
Thangavel C, Dean JL, Ertel A, et al. Therapeutically activating RB: reestablishing cell cycle control in endocrine therapy-resistant breast cancer. Endocr Relat Cancer. 2011;18:333–45.
Hortobagyi GN, Stemmer SM, Burris HA, et al. Ribociclib as first-line therapy for HR-positive, advanced breast cancer. N Engl J Med. 2016;375:1738–48.
Ibrance® (palbociclib) capsules [prescribing information]: New York, NY: Pfizer; 2017.
Kisqal® (ribociclib) tablets [prescribing information]: East Hanover, NJ: Novartis; 2017.
Verzenio™ (abemaciclib) tablets [prescribing information]: Indianapolis, IN: Lilly; 2017.
Goetz MP, Toi M, Campone M, et al. MONARCH 3: Abemaciclib as initial therapy for advanced breast cancer. J Clin Oncol. 2017;35:3638–46.
Turner N, Ro J, André F, et al. Palbociclib in hormone-receptor-positive advanced breast cancer. N Engl J Med. 2015;373:209–19.
Fribbens C, O’Leary B, Kilburn L, et al. Plasma ESR1 mutations and the treatment of estrogen receptor-positive advanced breast cancer. J Clin Oncol. 2016;34:2961–8.
Sammons SL, Topping DL, Blackwell KL. HR+, HER2- advanced breast cancer and CDK4/6 inhibitors: mode of action, clinical activity, and safety profiles. Curr Cancer Drug Targets. 2017;17:637–49.
Loibl S, Demichele A, Turner NM, et al. Impact of palbociclib plus fulvestrant on patient reported general health status compared with fulvestrant alone in HR+, HER2– metastatic breast cancer [abstract]. Ann Oncol. 2016;27(suppl 6), 260P.
Slamon D, Neven P, Chia S, et al. Ribociclib (RIB) + fulvestrant (FUL) in postmenopausal women with hormone receptor-positive (HR+), HER2-negative (HER2–) advanced breast cancer (ABC): results from MONALEESA-3. J Clin Oncol. 2018;36(18 suppl):1000.
Clark AS, West K, Streicher S, Dennis PA. Constitutive and inducible Akt activity promotes resistance to chemotherapy, trastuzumab, or tamoxifen in breast cancer cells. Mol Cancer Ther. 2002;1:707–17.
Miller T, Hennessy B, González-Angulo A, et al. Hyperactivation of phosphatidylinositol-3 kinase promotes escape from hormone dependence in estrogen receptor–positive human breast cancer. J Clin Invest. 2010;120:2406–13.
Paplomata E, O’Regan R. The PI3K/AKT/mTOR pathway in breast cancer: targets, trials and biomarkers. Ther Adv Med Oncol. 2014;6:154–66.
Hanahan D, Weinberg RA. The hallmarks of cancer. Cell. 2000;100:57–70.
Wander SA, Hennessy BT, Slingerland JM. Next-generation mTOR inhibitors in clinical oncology: how pathway complexity informs therapeutic strategy. J Clin Invest. 2011;121:1231–41.
Beeram M, Tan Q, Tekmal R, Russell D, Middleton A, DeGraffenried L. Akt-induced endocrine therapy resistance is reversed by inhibition of mTOR signaling. Ann Oncol. 2007;18:1323–8.
Afinitor® (everolimus) tablets [prescribing information]: East Hanover, NJ: Novartis; 2017.
Yardley D, Pritchard K, Burris H, et al. Everolimus plus exemestane in postmenopausal patients with HR+ breast cancer: BOLERO-2 final progression-free survival analysis. Adv Ther. 2013;30:870–84.
Rugo HS, Seneviratne L, Beck JT, et al. Prevention of everolimus-related stomatitis in women with hormone receptor-positive, HER2-negative metastatic breast cancer using dexamethasone mouthwash (SWISH): a single-arm, phase 2 trial. Lancet Oncol. 2017;18:654–62.
Okkenhaug K. Rules of engagement: distinct functions for the four class I PI3K catalytic isoforms in immunity. Ann N Y Acad Sci. 2013;1280:24–6.
Cintas C, Guillermet-Guibert J. Heterogeneity of phosphatidylinositol-3-kinase (PI3K)/AKT/mammalian target of rapamycin activation in cancer: is PI3K isoform specificity important? Front Oncol. 2018;7:330.
Ellis M, Perou CM. The genomic landscape of breast cancer as a therapeutic roadmap. Cancer Discov. 2013;3:27–34.
Miller TW, Balko JM, Arteaga CL. Phosphatidylinositol 3-kinase and antiestrogen resistance in breast cancer. J Clin Oncol. 2011;29:4452–61.
Cancer Genome Atlas Network. Comprehensive molecular portraits of human breast tumours. Nature. 2012;490:61–70.
Bosch A, Li Z, Bergamaschi A, et al. PI3K inhibition results in enhanced estrogen receptor function and dependence in hormone receptor-positive breast cancer. Sci Transl Med. 2015;7:283ra51.
Sanchez CG, Ma CX, Crowder RJ, et al. Preclinical modeling of combined phosphatidylinositol-3-kinase inhibition with endocrine therapy for estrogen receptor-positive breast cancer. Breast Cancer Res. 2011;13:R21.
Guedj M, Marisa L, de Reynies A, et al. A refined molecular taxonomy of breast cancer. Oncogene. 2012;31:1196–206.
De Amicis F, Thirugnansampanthan J, Cui Y, et al. Androgen receptor overexpression induces tamoxifen resistance in human breast cancer cells. Breast Cancer Res Treat. 2010;121:1–11.
Cochrane D, Bernales S, Jacobsen B, et al. Role of the androgen receptor in breast cancer and preclinical analysis of enzalutamide. Breast Cancer Res. 2014;16:R7.
Scher HI, Fizazi K, Saad F, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012;367:1187–97.
Rahim B, O’Regan R. AR signaling in breast cancer. Cancers (Basel). 2017;9(3):pii: E21
Pérez-Salvia M, Esteller M. Bromodomain inhibitors and cancer therapy: from structures to applications. Epigenetics. 2017;12:323–39.
Sahni JM, Gayle SS, Bonk KL, et al. Bromodomain and extraterminal protein inhibition blocks growth of triple-negative breast cancers through the suppression of aurora kinases. J Biol Chem. 2016;291:23756–68.
Feng Q, Zhang Z, Shea MJ, et al. An epigenomic approach to therapy for tamoxifen-resistant breast cancer. Cell Res. 2014;24:809–19.
Lovén J, Hoke HA, Lin CY, et al. Selective inhibition of tumor oncogenes by disruption of super-enhancers. Cell. 2013;153:320–34.
Chapuy B, McKeown MR, Lin CY, et al. Discovery and characterization of super-enhancer-associated dependencies in diffuse large B cell lymphoma. Cancer Cell. 2013;24:777–90.
De Angelis C, Nardone A, Cataldo ML, et al. A novel BRD4 inhibitor enhances endocrine therapy efficacy and circumvents endocrine-resistance in estrogen receptor-positive breast cancer models [abstract]. Cancer Res. 2017;77(4 suppl):S4–01.
Juric D, Rodon J, Tabernero J, et al. Phosphatidylinositol 3-kinase α-selective inhibition with alpelisib (BYL719) in PIK3CA-altered solid tumors: results from the first-in-human study. J Clin Oncol. 2018;36(13):1291–9.
ClinicalTrials.gov. Efficacy and safety of treatment with alpelisib plus endocrine therapy in patients with HR+, HER2-negative aBC, with PIK3CA mutations, whose disease has progressed on or after CDK 4/6 treatment with an aromatase inhibitor (AI) or fulvestrant (BYLieve). https://clinicaltrials.gov/ct2/show/NCT03056755; 2018 Accessed February 1, 2018.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Medical writing support was provided by Abbie Saunders PhD and Dean Clarke PhD (Articulate Science Ltd). Financial support for medical editorial assistance and funding for open access publication were provided by Novartis Pharmaceuticals Corporation. Novartis Pharmaceuticals Corporation did not influence the content of the manuscript.
Conflicts of Interest
Kimberly Blackwell received grants paid to institution from AstraZeneca, Genentech, Novartis, and Pfizer; received honoraria from Advaxis, AstraZeneca, Bayer, Celgene, Celldex, Celltrion, Coherus Biosciences, Eisai, Eli Lilly, Genentech, GI Therapeutics, MacroGenics, Merck, Mylan GmbH, Novartis, Pfizer, Pierian Biosciences, Puma, Roche, Sandoz, Seattle Genetics, Syndax, and Visante; and is now employed by Eli Lilly. Sarah Sammons and Noah Kornblum have declared no conflicts of interest.
Additional information
The original version of this article was revised due to a retrospective Open Access order.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Sammons, S., Kornblum, N.S. & Blackwell, K.L. Fulvestrant-Based Combination Therapy for Second-Line Treatment of Hormone Receptor-Positive Advanced Breast Cancer. Targ Oncol 14, 1–12 (2019). https://doi.org/10.1007/s11523-018-0587-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-018-0587-9