Abstract
Health-related quality of life (HRQoL) is an important patient-reported outcome, yet research regarding HRQoL during pregnancy is limited. We examined HRQoL during pregnancy using the Patient Reported Outcomes Measurement Information System (PROMIS) Global Short Form (GSF) and validated the GSF compared to legacy HRQoL measures. We evaluated HRQoL among 161 women seeking pregnancy care in urban clinic settings. Participants completed measures of HRQoL, social support, antenatal depression, and utility. Descriptive statistics and correlation coefficients were calculated. Participants averaged 27(±6.6) years and were culturally diverse: 42% self-identified as Hispanic, 37% Black, non-Hispanic, 14% White, non-Hispanic and 7% multiracial or other. Mean estimated gestational age was 9 (±4.6) weeks. PROMIS GSF Physical T-scores were significantly correlated with SF-12 Physical Component Score (PCS) and Mental Component Score (MCS) HRQoL measures (correlation coefficient=0.40 and 0.49, p-value<0.0001, respectively), the Modified Kendler Social Support Index (MKSSI) (correlation coefficient=0.42, p-value<0.0001), and the Visual Analog Scale (VAS) measure of utility (correlation coefficient=0.19, p-value =0.04). GSF Mental T-scores were associated with SF-12 MCS and PCS (correlation coefficient=0.66, p-value<0.0001, and 0.26, p-value<0.01, respectively), MKSSI (correlation coefficient=0.50, p-value<0.0001), and VAS (correlation coefficient=0.29, p-value<0.01). GSF Physical and Mental scores were inversely associated with the Edinburgh Postpartum Depression Scale (EPDS), correlation coefficient= −0.62 and − 0.71, respectively (p-value<0.0001). GSF-derived utility measures demonstrate significant correlation with SF-12 PCS and MCS, MKSSI, EPDS, and VAS. Overall, PROMIS GSF domains demonstrate correlation with legacy HRQoL measures as well as validated measures of social support, depression, and utility among a diverse cohort of pregnant women.
Similar content being viewed by others
References
Alcantara, J., Alcantara, J. D., & Alcantara, J. (2015). The use of validated outcome measures in the chiropractic care of pregnant patients: a systematic review of the literature. Complementary Therapies in Clinical Practice, 21(2), 131–136. doi:10.1016/j.ctcp.2015.01.003.
Biratu, A., & Haile, D. (2015). Prevalence of antenatal depression and associated factors among pregnant women in Addis Ababa, Ethiopia: a cross-sectional study. Reproductive Health, 12, 99. doi:10.1186/s12978-015-0092-x.
Cella, D., Riley, W., Stone, A., Rothrock, N., Reeve, B., Yount, S., et al. (2010). The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. Journal of Clinical Epidemiology, 63(11), 1179–1194. doi:10.1016/j.jclinepi.2010.04.011.
Cella, D., Yount, S., Rothrock, N., Gershon, R., Cook, K., Reeve, B., et al. (2007). The Patient-Reported Outcomes Measurement Information System (PROMIS): progress of an NIH Roadmap cooperative group during its first two years. Medical Care, 45(5 Suppl 1), S3–S11. doi:10.1097/01.mlr.0000258615.42478.55.
Chang, S. R., Chen, K. H., Lin, M. I., Lin, H. H., Huang, L. H., & Lin, W. A. (2014). A repeated measures study of changes in health-related quality of life during pregnancy and the relationship with obstetric factors. Journal of Advanced Nursing, 70(10), 2245–2256. doi:10.1111/jan.12374.
Cox, J. L., Chapman, G., Murray, D., & Jones, P. (1996). Validation of the Edinburgh Postnatal Depression Scale (EPDS) in non-postnatal women. Journal of Affective Disorders, 39(3), 185–189.
Cox, J. L., Holden, J. M., & Sagovsky, R. (1987). Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. British Journal of Psychiatry, 150, 782–786.
Creinin, M. D. (2000). Randomized comparison of efficacy, acceptability and cost of medical versus surgical abortion. Contraception, 62(3), 117–124.
Curtin, S.C., Abma, J.C., & Ventura, S.J. (2013). Pregnancy rates for U.S. women continue to drop. In NCHS Data Brief Number 136, U.S. Department of Health and Human Services, CDC.
DeWalt, D. A., Rothrock, N., Yount, S., Stone, A. A., & Group, P. C. (2007). Evaluation of item candidates: the PROMIS qualitative item review. Medical Care, 45(5 Suppl 1), S12–S21. doi:10.1097/01.mlr.0000254567.79743.e2.
EuroQol, G. (1990). EuroQol--a new facility for the measurement of health-related quality of life. Health Policy, 16(3), 199–208.
Finer, L. B., & Zolna, M. R. (2014). Shifts in intended and unintended pregnancies in the United States, 2001–2008. American Journal of Public Health, 104(Suppl 1), S43–S48. doi:10.2105/AJPH.2013.301416.
Gibson, J., McKenzie-McHarg, K., Shakespeare, J., Price, J., & Gray, R. (2009). A systematic review of studies validating the Edinburgh postnatal depression scale in antepartum and postpartum women. Acta Psychiatrica Scandinavica, 119(5), 350–364. doi:10.1111/j.1600-0447.2009.01363.x.
Goldhaber-Fiebert, J. D., & Brandeau, M. L. (2015). Evaluating cost-effectiveness of interventions that affect fertility and childbearing: how health effects are measured matters. Medical Decision Making, 35(7), 818–846. doi:10.1177/0272989X15583845.
Hays, R. D., Bjorner, J. B., Revicki, D. A., Spritzer, K. L., & Cella, D. (2009). Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Quality of Life Research, 18(7), 873–880. doi:10.1007/s11136-009-9496-9.
Heron, J., O’Connor, T. G., Evans, J., Golding, J., Glover, V., & Team, A. S. (2004). The course of anxiety and depression through pregnancy and the postpartum in a community sample. Journal of Affective Disorders, 80(1), 65–73. doi:10.1016/j.jad.2003.08.004.
Jomeen, J., & Martin, C. R. (2005). The factor structure of the SF-36 in early pregnancy. Journal of Psychosomatic Research, 59(3), 131–138. doi:10.1016/j.jpsychores.2005.02.018.
Klem, M., Saghafi, E., Abromitis, R., Stover, A., Dew, M. A., & Pilkonis, P. (2009). Building PROMIS item banks: librarians as co-investigators. Quality of Life Research, 18(7), 881–888. doi:10.1007/s11136-009-9498-7.
Lubinga, S. J., Levine, G. A., Jenny, A. M., Ngonzi, J., Mukasa-Kivunike, P., Stergachis, A., et al. (2013). Health-related quality of life and social support among women treated for abortion complications in western Uganda. Health and Quality of Life Outcomes, 11, 118. doi:10.1186/1477-7525-11-118.
Lyon, D., McCain, N., Elswick, R. K., Sturgill, J., Ameringer, S., Jallo, N., et al. (2014). Biobehavioral examination of fatigue across populations: report from a P30 Center of Excellence. Nursing Outlook, 62(5), 322–331. doi:10.1016/j.outlook.2014.06.008.
Matthey, S., Henshaw, C., Elliott, S., & Barnett, B. (2006). Variability in use of cut-off scores and formats on the Edinburgh postnatal depression scale: implications for clinical and research practice. Archives of Women’s Mental Health, 9(6), 309–315. doi:10.1007/s00737-006-0152-x.
Mogos, M. F., August, E. M., Salinas-Miranda, A. A., Sultan, D. H., & Salihu, H. M. (2013). A systematic review of quality of life measures in pregnant and postpartum mothers. Applied Research in Quality of Life, 8(2), 219–250.
Mortazavi, F., Mousavi, S. A., Chaman, R., & Khosravi, A. (2014). Maternal quality of life during the transition to motherhood. Iranian Red Crescent Medical Journal, 16(5), e8443. doi:10.5812/ircmj.8443.
Myers, E. R. (2015). How should we estimate the cost-effectiveness of interventions that affect reproduction? Medical Decision Making, 35(7), 812–814. doi:10.1177/0272989X15602227.
Petrou, S., Morrell, J., & Spiby, H. (2009). Assessing the empirical validity of alternative multi-attribute utility measures in the maternity context. Health and Quality of Life Outcomes, 7, 40. doi:10.1186/1477-7525-7-40.
PROMIS (2010). Scoring PROMIS Global Short Form. https://www.assessmentcenter.net/documents/Scoring%20PROMIS%20Global%20short%20form.pdf. Accessed 27 Jan 2016.
Revicki, D. A., Kawata, A. K., Harnam, N., Chen, W. H., Hays, R. D., & Cella, D. (2009). Predicting EuroQol (EQ-5D) scores from the patient-reported outcomes measurement information system (PROMIS) global items and domain item banks in a United States sample. Quality of Life Research, 18(6), 783–791. doi:10.1007/s11136-009-9489-8.
Robinson, A., Loomes, G., & Jones-Lee, M. (2001). Visual analog scales, standard gambles, and relative risk aversion. Medical Decision Making, 21(1), 17–27.
Rochat, T. J., Richter, L. M., Doll, H. A., Buthelezi, N. P., Tomkins, A., & Stein, A. (2006). Depression among pregnant rural South African women undergoing HIV testing. JAMA, 295(12), 1376–1378. doi:10.1001/jama.295.12.1376.
Schwarz, E. B., Smith, R., Steinauer, J., Reeves, M. F., & Caughey, A. B. (2008). Measuring the effects of unintended pregnancy on women’s quality of life. Contraception, 78(3), 204–210. doi:10.1016/j.contraception.2008.04.120.
Senturk, V., Abas, M., Berksun, O., & Stewart, R. (2011). Social support and antenatal depression in extended and nuclear family environments in Turkey: a cross-sectional survey. BMC Psychiatry, 11, 48. doi:10.1186/1471-244X-11-48.
Shaheen, R., & Lindholm, L. (2006). Quality of life among pregnant women with chronic energy deficiency in rural Bangladesh. Health Policy, 78(2–3), 128–134. doi:10.1016/j.healthpol.2005.11.008.
Siu, A. L., U. S. P. S. T. Force, Bibbins-Domingo, K., Grossman, D. C., Baumann, L. C., Davidson, K. W., et al. (2016). Screening for depression in adults: US preventive services task force recommendation statement. JAMA, 315(4), 380–387. doi:10.1001/jama.2015.18392.
Spoozak, L., Gotman, N., Smith, M. V., Belanger, K., & Yonkers, K. A. (2009). Evaluation of a social support measure that may indicate risk of depression during pregnancy. Journal of Affective Disorders, 114(1–3), 216–223. doi:10.1016/j.jad.2008.07.015.
Tavoli, Z., Tavoli, A., Amirpour, R., Hosseini, R., & Montazeri, A. (2016). Quality of life in women who were exposed to domestic violence during pregnancy. BMC Pregnancy and Childbirth, 16(1), 19. doi:10.1186/s12884-016-0810-6.
Teresi, J. A., Ocepek-Welikson, K., Kleinman, M., Eimicke, J. P., Crane, P. K., Jones, R. N., et al. (2009). Analysis of differential item functioning in the depression item bank from the Patient Reported Outcome Measurement Information System (PROMIS): an item response theory approach. Psychology Science Quarterly, 51(2), 148–180.
Torrance, G. W. (1987). Utility approach to measuring health-related quality of life. Journal of Chronic Diseases, 40(6), 593–603.
Tsai, S. Y., Lee, P. L., Lin, J. W., & Lee, C. N. (2016). Cross-sectional and longitudinal associations between sleep and health-related quality of life in pregnant women: a prospective observational study. International Journal of Nursing Studies. doi:10.1016/j.ijnurstu.2016.01.001.
Ubel, P. A., Loewenstein, G., & Jepson, C. (2003). Whose quality of life? A commentary exploring discrepancies between health state evaluations of patients and the general public. Quality of Life Research, 12(6), 599–607.
van Mello, N. M., Mol, F., Hajenius, P. J., Ankum, W. M., Mol, B. W., van der Veen, F., et al. (2015). Randomized comparison of health-related quality of life in women with ectopic pregnancy or pregnancy of unknown location treated with systemic methotrexate or expectant management. European Journal of Obstetrics, Gynecology and Reproductive Biology, 192, 1–5. doi:10.1016/j.ejogrb.2015.06.007.
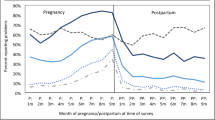
Vinturache, A., Stephenson, N., McDonald, S., Wu, M., Bayrampour, H., & Tough, S. (2015). Health-related quality of life in pregnancy and postpartum among women with assisted conception in Canada. Fertility and Sterility, 104(1), 188 e181–195 e181. doi:10.1016/j.fertnstert.2015.04.012.
Ware, J., Jr., Kosinski, M., & Keller, S. D. (1996). A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Medical Care, 34(3), 220–233.
Washington, C. I., Jamshidi, R., Thung, S. F., Nayeri, U. A., Caughey, A. B., & Werner, E. F. (2015). Timing of postpartum intrauterine device placement: a cost-effectiveness analysis. Fertility and Sterility, 103(1), 131–137. doi:10.1016/j.fertnstert.2014.09.032.
Weinstein, M. C., Torrance, G., & McGuire, A. (2009). QALYs: the basics. Value in Health, 12(Suppl 1), S5–S9. doi:10.1111/j.1524-4733.2009.00515.x.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Gariepy received a Clinical Translational Science Award (CTSA Grant Number UL1 TR000142) from the National Center for Advancing Translational Science (NCATS). Dr. Lundsberg was supported by CTSA Grant Number UL1 TR000142. Dr. Yonkers has no conflicts of interest related to the current publication; outside the submitted work; she has worked as a consultant for Pontifax regarding premenstrual dysphoric disorders, received NIH funding, and royalties from Up-to-Date. Dr. Schwarz and Dr. Vilardo declare no conflict of interest.
Ethical Approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Funding
This study was funded by CTSA Grant Number UL1 TR000142 from the National Center for Advancing Translational Science (NCATS), a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
Rights and permissions
About this article
Cite this article
Lundsberg, L.S., Schwarz, E.B., Vilardo, N.A. et al. Clinical Validation of PROMIS Global Short Form in Pregnancy. Applied Research Quality Life 13, 89–103 (2018). https://doi.org/10.1007/s11482-017-9507-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11482-017-9507-x