Abstract
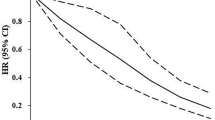
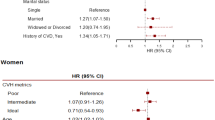
Existing evidence on the relationship between cardiovascular health (CVH) metrics and cardiovascular disease (CVD) was primarily derived from western populations. We aimed to evaluate the benefits of ideal CVH metrics on preventing incident atherosclerotic CVD (ASCVD) in Chinese population. This study was conducted among 93,987 adults from the China-PAR project (Prediction for ASCVD Risk in China) who were followed up until 2015. Cox proportional hazard regression models were used to estimate the hazard ratios (HRs) and their corresponding 95% confidence intervals (CIs) of CVH metrics for the risk of ASCVD, including coronary heart disease (CHD), stroke and ASCVD death. We further estimated the population-attributable risk percentage (PAR%) of these metrics in relation to each outcome. We observed gradient inverse associations between the number of ideal CVH metrics and ASCVD incidence. Compared with participants having ≤2 ideal CVH metrics, the multivariable-adjusted HRs (95% CIs) of ASCVD for those with 3, 4, 5, 6 and 7 ideal CVH metrics were 0.83 (0.74–0.93), 0.66 (0.59–0.74), 0.55 (0.48–0.61), 0.44 (0.38–0.50) and 0.24 (0.18–0.31), respectively (P for trend <0.0001). Approximately 62.1% of total ASCVD, 38.7% of CHD, 66.4% of stroke, and 60.5% of ASCVD death were attributable to not achieving all the seven ideal CVH metrics. After adjusting effects of ideal health factors, having four ideal health behaviors could independently bring adults health benefits in preventing 17.4% of ASCVD, 18.0% of CHD, 16.7% of stroke, and 10.1% of ASCVD death. Among all the seven CVH metrics, to keep with ideal blood pressure (BP) implied the largest public health gains against various ASCVD events (PAR% between 33.0% and 47.2%), while ideal diet was the metric most difficult to be achieved in the long term. Our study indicates that the more ideal CVH metrics adults have, the less ASCVD burden there is in China. Special efforts of health education and behavior modification should be made on keeping ideal BP and dietary habits in general Chinese population to prevent the epidemic of ASCVD.
Similar content being viewed by others
References
Bambs, C., and Reis, S.E. (2011). Embracing primordial prevention for ideal cardiovascular health. Fut Cardiol 7, 447–450.
Bellavia, A., Stilling, F., and Wolk, A. (2016). High red meat intake and allcause cardiovascular and cancer mortality: is the risk modified by fruit and vegetable intake? Am J Clin Nutr 104, 1137–1143.
Bi, Y., Jiang, Y., He, J., Xu, Y., Wang, L., Xu, M., Zhang, M., Li, Y., Wang, T., Dai, M., et al. (2015). Status of cardiovascular health in Chinese adults. J Am Coll Cardiol 65, 1013–1025.
Claas, S.A., and Arnett, D.K. (2016). The role of healthy lifestyle in the primordial prevention of cardiovascular disease. Curr Cardiol Rep 18, 56.
Dong, C., Rundek, T., Wright, C.B., Anwar, Z., Elkind, M.S.V., and Sacco, R.L. (2012). Ideal cardiovascular health predicts lower risks of myocardial infarction, stroke, and vascular death across whites, blacks, and hispanics: The Northern Manhattan Study. Circulation 125, 2975–2984.
Folsom, A.R., Yatsuya, H., Nettleton, J.A., Lutsey, P.L., Cushman, M., Rosamond, W.D., and Rosamond, W.D. (2011). Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol 57, 1690–1696.
GBD 2013 Mortality and Causes of Death Collaborators. (2015). Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 385, 117–171.
Gakidou, E., Afshin, A., Abajobir, A.A., Abate, K.H., Abbafati, C., Abbas, K.M., Abd-Allah, F., Abdulle, A.M., Abera, S.F., Aboyans, V., et al. (2017). Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390, 1345–1422.
Gu, D., He, J., Coxson, P.G., Rasmussen, P.W., Huang, C., Thanataveerat, A., Tzong, K.Y., Xiong, J., Wang, M., Zhao, D., et al. (2015). The costeffectiveness of low-cost essential antihypertensive medicines for hypertension control in China: a modelling study. PLoS Med 12, e1001–860.
Gu, D., He, J., Duan, X., Reynolds, K., Wu, X., Chen, J., Huang, G., Chen, C.S., and Whelton, P.K. (2006). Body weight and mortality among men and women in China. JAMA 295, 776–783.
He, J., Gu, D., Chen, J., Wu, X., Kelly, T.N., Huang, J., Chen, J., Chen, C. S., Bazzano, L.A., Reynolds, K., et al. (2009). Premature deaths attributable to blood pressure in China: a prospective cohort study. Lancet 374, 1765–1772.
He, J., Gu, D., Wu, X., Reynolds, K., Duan, X., Yao, C., Wang, J., Chen, C. S., Chen, J., Wildman, R.P., et al. (2005). Major causes of death among men and women in China. N Engl J Med 353, 1124–1134.
Kim, J.Y., Ko, Y.J., Rhee, C.W., Park, B.J., Kim, D.H., Bae, J.M., Shin, M. H., Lee, M.S., Li, Z.M., and Ahn, Y.O. (2013). Cardiovascular health metrics and all-cause and cardiovascular disease mortality among middle-aged men in Korea: the Seoul Male Cohort Study. J Prev Med Public Health 46, 319–328.
Lloyd-Jones, D.M., Hong, Y., Labarthe, D., Mozaffarian, D., Appel, L.J., Van Horn, L., Greenlund, K., Daniels, S., Nichol, G., Tomaselli, G.F., et al. (2010). Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic impact goal through 2020 and beyond. Circulation 121, 586–613.
Montero, D., Walther, G., Perez-Martin, A., Roche, E., and Vinet, A. (2012). Endothelial dysfunction, inflammation, and oxidative stress in obese children and adolescents: markers and effect of lifestyle intervention. Obes Rev 13, 441–455.
Nahrendorf, M., and Swirski, F.K. (2015). Lifestyle effects on hematopoiesis and atherosclerosis. Circ Res 116, 884–894.
Nayor, M., Enserro, D.M., Vasan, R.S., and Xanthakis, V. (2016). Cardiovascular health status and incidence of heart failure in the Framingham Offspring Study. Circ Heart Fail 9, e002416.
Rebholz, C.M., Reynolds, K., Wofford, M.R., Chen, J., Kelly, T.N., Mei, H., Whelton, P.K., and He, J. (2013). Effect of soybean protein on novel cardiovascular disease risk factors: a randomized controlled trial. Eur J Clin Nutr 67, 58–63.
Schoenfeld, D. (1982). Partial residuals for the proportional hazards regression model. Biometrika 69, 239–241.
Shay, C.M., Ning, H., Allen, N.B., Carnethon, M.R., Chiuve, S.E., Greenlund, K.J., Daviglus, M.L., and Lloyd-Jones, D.M. (2012). Status of cardiovascular health in US adults: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2003-2008. Circulation 125, 45–56.
Spiegelman, D., Hertzmark, E., and Wand, H.C. (2007). Point and interval estimates of partial population attributable risks in cohort studies: examples and software. Cancer Causes Control 18, 571–579.
Wang, S.S., Lay, S., Yu, H.N., and Shen, S.R. (2016). Dietary Guidelines for Chinese Residents (2016): comments and comparisons. J Zhejiang Univ Sci B 17, 649–656.
Wu, H.Y., Sun, Z.H., Cao, D.P., Wu, L.X., and Zeng, Q. (2013). Cardiovascular health status in Chinese adults in urban areas: analysis of the Chinese Health Examination Database 2010. Int J Cardiol 168, 760–764.
Yang, G., Wang, Y., Zeng, Y., Gao, G.F., Liang, X., Zhou, M., Wan, X., Yu, S., Jiang, Y., Naghavi, M., et al. (2013). Rapid health transition in China, 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet 381, 1987–2015.
Yang, Q., Cogswell, M.E., Flanders, W.D., Hong, Y., Zhang, Z., Loustalot, F., Gillespie, C., Merritt, R., and Hu, F.B. (2012). Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA 307, 1273–1283.
Yang, X., Li, J., Hu, D., Chen, J., Li, Y., Huang, J., Liu, X., Liu, F., Cao, J., Shen, C., et al. (2016). Predicting the 10-year risks of atherosclerotic cardiovascular disease in Chinese population. Circulation 134, 1430–1440.
Zhang, C., Qin, Y.Y., Wei, X., Yu, F.F., Zhou, Y.H., and He, J. (2015). Tea consumption and risk of cardiovascular outcomes and total mortality: a systematic review and meta-analysis of prospective observational studies. Eur J Epidemiol 30, 103–113.
Zhang, Q., Zhou, Y., Gao, X., Wang, C., Zhang, S., Wang, A., Li, N., Bian, L., Wu, J., Jia, Q., et al. (2013). Ideal cardiovascular health metrics and the risks of ischemic and intracerebral hemorrhagic stroke. Stroke 44, 2451–2456.
Zhao, D. (1999). Poisson regression adjustment of event rates and its macro procedure ADJ_POIS. SAS Users Group 24th International Annual Conference. (Florida, USA).
Acknowledgements
The authors thank the staffs and participants of the China-PAR project for their important participation and contribution. This work was supported by grants from the CAMS Innovation Fund for Medical Sciences (2017-12M-1-004), Ministry of Science and Technology of China (2017YFC0211700), and National Natural Science Foundation of China (91643208).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Han, C., Liu, F., Yang, X. et al. Ideal cardiovascular health and incidence of atherosclerotic cardiovascular disease among Chinese adults: the China-PAR project. Sci. China Life Sci. 61, 504–514 (2018). https://doi.org/10.1007/s11427-018-9281-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11427-018-9281-6