Abstract
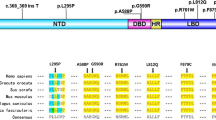
We investigated the androgen receptor (AR) gene mutation profiles of Chinese patients exhibiting severe androgen insensitivity syndrome (AIS) phenotypes. The present study enrolled 28 patients with genetically diagnosed AIS, who presented with severe phenotypes (Prader grade 0–3). Patients and some family members were screened via amplification and sequencing of their AR exons 1–8, including the corresponding intronic flanking regions. Luteinizing (LH), follicle-stimulating (FSH), and testosterone (T) hormone levels were found to be slightly, but not significantly, higher in patients with complete androgen insensitivity syndrome (CAIS) than in patients with partial androgen insensitivity syndrome (PAIS) (P>0.05). We identified 24 different AR mutations, including 12 that were novel. Ten patients (cases 2, 3, 10, 28, 11, 12, 19, 20, 24, and 25) were found to carry five recurrent mutations (p.Y572S, p.P914S, p.S176R, p.Y782N, and p.R841H); of these, p.Y572S, p.S176R, and p.Y782N were novel. Among the mutations identified in patients with CAIS, six (66.7%) were characterized as single-nucleotide missense mutations, and six (66.7%) were found to be located in the AR ligand-binding domain (LBD). Among the mutations identified in patients with PAIS, 15 (93.8%) were found to be missense, and 11 (68.8%) were found to be located in the LBD. Patients 10 and 28 were determined to harbor the same missense mutation (p.P914S), but were diagnosed with CAIS and PAIS, respectively. Sex hormone levels were slightly, but not significantly, elevated in patients with CAIS compared to those with PAIS. Missense mutations spanning AR exons 1–8 were the predominant form of identified mutations, and these were mostly located in the AR LBD. Approximately 50% of the identified mutations were novel, and have enriched the AR gene-mutation database. Patients harboring identical mutations were in some instances found to exhibit divergent phenotypes.
Similar content being viewed by others
References
Ahmed, S.F., Cheng, A., Dovey, L., Hawkins, J.R., Martin, H., Rowland, J., Shimura, N., Tait, A.D., and Hughes, I.A. (2000). Phenotypic features, androgen receptor binding, and mutational analysis in 278 clinical cases reported as androgen insensitivity syndrome 1. J Clin Endocrinol Metab 85, 658–665.
Avila, D.M., Wilson, C.M., Nandi, N., Griffin, J.E., and McPhaul, M.J. (2002). Immunoreactive AR and genetic alterations in subjects with androgen resistance and undetectable AR levels in genital skin fibroblast ligand-binding assays. J Clin Endocrinol Metab 87, 182–188.
Alhomaidah, D., McGowan, R., and Ahmed, S.F. (2017). The current state of diagnostic genetics for conditions affecting sex development. Clin Genet 91, 157–162.
Audi, L., Fernández-Cancio, M., Carrascosa, A., Andaluz, P., Torán, N., Piró, C., Vilaró, E., Vicens-Calvet, E., Gussinyé, M., Albisu, M.A., Yeste, D., Clemente, M., Hernández de la Calle, I., Del Campo, M., Vendrell, T., Blanco, A., Martínez-Mora, J., Granada, M.L., Salinas, I., Forn, J., Calaf, J., Angerri, O., Martínez-Sopena, M.J., Del Valle, J., García, E., Gracia-Bouthelier, R., Lapunzina, P., Mayayo, E., Labarta, J.I., Lledó, G., Sánchez Del Pozo, J., Arroyo, J., Pérez-Aytes, A., Beneyto, M., Segura, A., Borrás, V., Gabau, E., Caimarí, M., Rodríguez, A., Martínez-Aedo, M.J., Carrera, M., Castaño, L., Andrade, M., Bermúdez de la Vega, J.A., and Bermúdez de la Vega, J.A. (2010). Novel (60%) and recurrent (40%) androgen receptor gene mutations in a series of 59 patients with a 46,XY disorder of sex development. J Clin Endocrinol Metab 95, 1876–1888.
Bangsbøll, S., Qvist, I., Lebech, P.E., and Lewinsky, M. (1992). Testicular feminization syndrome and associated gonadal tumors in Denmark. Acta Obstet Gynecol Scand 71, 63–66.
Boehmer, A.L.M., Brinkmann, A.O., Nijman, R.M., Verleun-Mooijman, M.C.T., de Ruiter, P., Niermeijer, M.F., and Drop, S.L.S. (2001). Phenotypic variation in a family with partial androgen insensitivity syndrome explained by differences in 5a dihydrotestosterone availability. J Clin Endocrinol Metab 86, 1240–1246.
Brown, C.J., Goss, S.J., Lubahn, D.B., Joseph, D.R., Wilson, E.M., French, F.S., and Willard, H.F. (1989). Androgen receptor locus on the human X chromosome: regional localization to Xq11-12 and description of a DNA polymorphism. Am J Hum Genet 44, 264–269.
Bang, A.K., Nordkap, L., Almstrup, K., Priskorn, L., Petersen, J.H., Rajpert-De Meyts, E., Andersson, A.M., Juul, A., and Jørgensen, N. (2017). Dynamic GnRH and hCG testing: establishment of new diagnostic reference levels. Eur J Endocrinol 176, 379–391.
Cools, M., Drop, S.L.S., Wolffenbuttel, K.P., Oosterhuis, J.W., and Looijenga, L.H.J. (2006). Germ cell tumors in the intersex gonad: old paths, new directions, moving frontiers. Endocr Rev 27, 468–484.
Gottlieb, B., Beitel, L.K., and Trifiro, M.A. (2001). Somatic mosaicism and variable expressivity. Trends Genets 17, 79–82.
Huang, H., Wang, C., and Tian, Q. (2017). Gonadal tumour risk in 292 phenotypic female patients with disorders of sex development containing Y chromosome or Y-derived sequence. Clin Endocrinol 86, 621–627.
Hughes, I.A., Davies, J.D., Bunch, T.I., Pasterski, V., Mastroyannopoulou, K., and MacDougall, J. (2012). Androgen insensitivity syndrome. Lancet 380, 1419–1428.
Gottlieb, B., Beitel, L.K., Nadarajah, A., Paliouras, M., and Trifiro, M. (2012). The androgen receptor gene mutations database: 2012 update. Hum Mutat 33, 887–894.
Hughes, I.A., Evans, B.A.J., Ismail, R., and Matthews, J. (1986). Complete androgen insensitivity syndrome characterized by increased concentration of a normal androgen receptor in genital skin fibroblasts. J Clin Endocrinol Metab 63, 309–315.
Hiort, O., Wodtke, A., Struve, D., Zöllner, A., and Sinnecker, G.H.G. (1994). Detection of point mutations in the androgen receptor gene using nonisotopic single strand conformation polymorphism analysis. Hum Mol Genet 3, 1163–1166.
Imasaki, K., Hasegawa, T., Okabe, T., Sakai, Y., Haji, M., Takayanagi, R., and Nawata, H. (1994). Single amino acid substitution (840Arg -> His) in the hormone-binding domain of the androgen receptor leads to incomplete androgen insensitivity syndrome associated with a thermolabile androgen receptor. Eur J Endocrinol 130, 569–574.
Jääskeläinen, J. (2012). Molecular biology of androgen insensitivity. Mol Cell Endocrinol 352, 4–12.
Jagiello, G., and Atwell, J.D. (1962). Prevalence of testicular feminisation. Lancet 279, 329.
Ledig, S., Jakubiczka, S., Neulen, J., Aulepp, U., Burck-Lehmann, U., Mohnike, K., Thiele, H., Zierler, H., Brewer, C., and Wieacker, P. (2005). Novel and recurrent mutations in patients with androgen insensitivity syndromes. Horm Res Paediatr 63, 263–269.
Lim, H.N., Nixon, R.M., Chen, H., Hughes, I.A., and Hawkins, J.R. (2001). Evidence that longer androgen receptor polyglutamine repeats are a causal factor for genital abnormalities. J Clin Endocrinol Metab 86, 3207–3210.
Manuel, M., Katayama, K.P., and Jones Jr., H.W. (1976). The age of occurrence of gonadal tumors in intersex patients with a Y chromosome. Am J Obstetr Gynecol 124, 293–300.
Mongan, N.P., Tadokoro-Cuccaro, R., Bunch, T., and Hughes, I.A. (2015). Androgen insensitivity syndrome. Best Pract Res Clin Endocrinol Metab 29, 569–580.
Quigley, C.A., Evans, B.A., Simental, J.A., Marschke, K.B., Sar, M., Lubahn, D.B., Davies, P., Hughes, I.A., Wilson, E.M., and French, F.S. (1992). Complete androgen insensitivity due to deletion of exon C of the androgen receptor gene highlights the functional importance of the second zinc finger of the androgen receptor in vivo. Mol Endocrinol 6, 1103–1112.
Simanainen, U., Brogley, M., Gao, Y.R., Jimenez, M., Harwood, D.T., Handelsman, D.J., and Robins, D.M. (2011). Length of the human androgen receptor glutamine tract determines androgen sensitivity in vivo. Mol Cell Endocrinol 342, 81–86.
Shaffer, P.L., Jivan, A., Dollins, D.E., Claessens, F., and Gewirth, D.T. (2004). Structural basis of androgen receptor binding to selective androgen response elements. Proc Natl Acad Sci USA 101, 4758–4763.
Siu, C.C., and Scott, M.D. (2014). Constitutive activity of the androgen receptor. Adv Pharmacol 70, 327–366.
Scheiber, D., Barta, C., Halász, Z., Sallai, Á., Rácz, K., Ságodi, L., Fekete, G., Hiort, O., and Solyom, J. (2003). Mutational analysis of hungarian patients with androgen insensitivity syndrome. J Pediat Endocrinol Metab 16, 367–373.
Wang, X., Wang, X.R., Liu, M.G., Wang, Q., and Liu, J.Y. (2006). Genetic analysis of a family with 46, XY “Female” associated with infertility. Acta Geneta Sin 33, 19–25.
Yen, J.L., Chang, K.H., Sheu, J.C., Lee, Y.J., and Tsai, L.P. (2005). Partial androgen insensitivity syndrome with R840H mutation in androgen receptor: report of one case. Acta Paediatr Taiwan 46, 101–105.
Acknowledgements
The authors thank the patients and families who gave their consent for, and collaborated in this study. This work was supported by the Public Health Project for Residents in Beijing (Z151100003915103), and the National Key Research and Development Program of China (2016YFC0901505).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, Y., Gong, C., Wang, X. et al. AR mutations in 28 patients with androgen insensitivity syndrome (Prader grade 0–3). Sci. China Life Sci. 60, 700–706 (2017). https://doi.org/10.1007/s11427-017-9084-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11427-017-9084-9