Abstract
Background
Although relatively rare, non-unions and mal-unions of tibial plateau fractures present significant challenges for the orthopedic surgeon. With careful pre-operative planning, tibial plateau mal-union or non-union revision surgery with intra-articular and varus opening osteotomies can provides good functional results when performed early (within 1 year) after primary surgical procedure.
Questions/Purposes
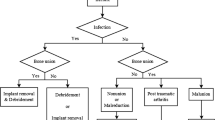
We present our treatment algorithm for approaching and treating non-union or mal-union of tibial plateau fractures. Our aim is to give surgeons treating these difficult injuries an overview of the pertinent literature as well as describe the challenges and pitfalls we have experienced when treating non-union or mal-union of tibial plateau fractures.
Methods
Using two case examples from our institution, one for mal-union and one for mal-reduction, we describe our treatment algorithm and surgical technique for managing these difficult injuries. We also provide a brief literature review outlining relevant studies and summarizing outcomes for similar injuries. A systematic literature review was conducted with the aim of determining the methods and outcomes commonly reported in the literature regarding revision surgery following tibial plateau non-union or mal-union. Due to the nature of revision surgery, there are no long-term randomized trials dealing with outcomes, but rather several smaller case series exist from which larger conclusions have to be drawn.
Results
To date, we have successfully treated approximately 35 patients with this technique, and clinical follow-up continues to show good functional outcomes with reduced pain and little radiographic evidence of arthritic changes. Restoring long leg alignment, anatomic reduction of the articular surface, and achieving stable internal fixation are paramount in achieving the best long-term outcome. Due to the shallow soft tissue envelope around the proximal tibia, and the tendency for these fractures to fall into progressive valgus collapse, these problems can seem intimidating and complex. However, with well-planned surgery and meticulous surgical technique, reliable healing can be achieved.
Conclusion
By outlining our method, we hope to provide other surgeons with an algorithm to guide clinical and operative decision making. These difficult injuries can be daunting to treat, but if performed before the onset of severe degenerative arthritis, early revision surgery, as we describe, can be a viable alternative to total knee arthroplasty, particularly in younger, more active patients.









Similar content being viewed by others
References
Borelli J Jr, Prickett W, Song E, Becker D, Ricci W. Extraosseous blood supply of the tibia and the effects of different plating techniques: a human cadaveric study. J Orthop Trauma. 2002; 16: 691-695.
Chan DB, Jeffcoat DM, Lorich DG, Helfet DL. Nonunions around the knee joint. International Orthopaedics. 2010; 34: 271-281.
Court-Brown CM, Caesar B. The epidemiology of fractures. In: Heckman JD, Buchholz RW, Court-Brown CM, eds. Rockwood and Greens Fractures in Adults. 6th ed. Philadelphia, PA: Lippincott, Williams and Wilkins; 2006: 95-113.
Kerkhoffs G, Rademakers M, Altena M, Marti R. Combined intra-articular and varus opening wedge osteotomy for lateral depression and valgus malunion of the proximal part of the tibia: surgical technique. J Bone Joint Surg Am. 2009; 91: 101-115.
Kerkhoffs G, Rademakers M, Altena M, Marti R. Combined intra-articular and varus opening wedge osteotomy for lateral depression and valgus malunion of the proximal part of the tibia. J Bond Joint Surg Am. 2008; 90: 1252-1257.
Krettek C, Hawi N, Jagodzinski M. Intracondylar segment osteotomy: correction of intra-articular malalignment after fracture of the tibial plateau. Unfallchirurg. 2013; 116(5): 413-426. German.
Marti RK, Verhage RA, Kerkhoffs GM, Moojen TM. Proximal tibial varus osteotomy. Indications, technique, and five to twenty-one-year results. J Bone Joint Surg Am. 2001; 83: 164-170.
Martinez A, Sarmiento A, Latta LL. Closed fractures of the proximal tibia treated with a functional brace. Clin Orthop. 2003; 417: 293-302.
Moore TM, Patzakis MJ, Harvey JP. Tibial plateau fractures, definition, demographics, treatment rationale, and long term results of closed traction management or operative reduction. J Orthop Trauma. 1987; 1(2): 97-119.
Stevens DG, Beharry R, McKee MD, et al. The long-term functional outcome of operatively treated tibial plateau fractures. J Orthop Trauma. 2001; 15: 312-320.
Toro-Arbelaez JB, Gardner MJ, Shindle MK, Cabas JM, Lorich DG, Helfet DL. Open reduction and internal fixation of intraarticular tibial plateau nonunions. Injury, Int. 2007; 38: 378-383.
Watson JT, Schatzker J. Tibial plateau fractures. In: Browner BD, ed. Skeletal trauma: basic science, management, and reconstruction. 3rd ed. Philadelphia, Pa: Saunders; 2003: 2047-2130.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
LT Dominic L. Van Nielen, MD, LCDR, Christopher S. Smith, MD, David L. Helfet, MD and Peter Kloen, MD, PhD, have declared that they have no conflict of interest.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent
Informed consent was waived from all patients for being included in the study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Disclaimers
The views expressed in this article are those of the author(s) and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the US Government.
Dr. Dominic Van Nielen and Dr. Christopher Smith are military service members. This work was prepared as part of their official duties. Title 17 U.S.C. 105 provides that “Copyright protection under this title is not available for any work of the United States Government.” Title 17 U.S.C. 101 defines a US Government work as a work prepared by a military service member or employee of the US Government as part of that person’s official duties.
Additional information
Level of Evidence: Level IV: Surgical Technique
Research performed at Academic Medical Center, University of Amsterdam, Amsterdam, Netherlands.
Rights and permissions
About this article
Cite this article
Van Nielen, D.L., Smith, C.S., Helfet, D.L. et al. Early Revision Surgery for Tibial Plateau Non-union and Mal-union. HSS Jrnl 13, 81–89 (2017). https://doi.org/10.1007/s11420-016-9529-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11420-016-9529-1