Abstract
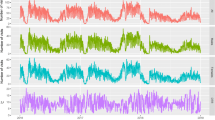
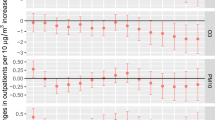
Ambient air pollutants have been linked to adverse health outcomes, but evidence is still relatively rare in college students. Upper respiratory tract infection (URTI) is a common disease of respiratory system among college students. In this study, we assess the acute effect of air pollution on clinic visits of college students for URTI in Wuhan, China. Data on clinic visits due to URTI were collected from Wuhan University Hospital, meteorological factors (including daily temperature and relative humidity) provided by Wuhan Meteorological Bureau, and air pollutants by Wuhan Environmental Protection Bureau. In the present study, generalized additive model with a quasi-Poisson distribution link function was used to examine the association between ambient air pollutants (fine particulate matter (PM2.5), particulate matter (PM10), sulfur dioxide (SO2), nitrogen dioxide (NO2), and ozone (O3)) and the daily number of clinic visits of college students for URTI at Wuhan University Hospital in Wuhan, China. In the meantime, the model was adjusted for the confounding effects of long-term trends, seasonality, day of the week, public holidays, vacation, and meteorological factors. The best degrees of free in model were selected based on AIC (Akaike Information Criteria). The effect modification by gender was also examined. A total of 44,499 cases with principal diagnosis of URTI were included from January 1, 2016, to December 31, 2018. In single-pollutant models, the largest increment of URTI visits were found at lag 0 day in single-day lags, and the effect values in cumulative lags were greater than those in single-day lags. PM2.5 (0.74% (95%CI: 0.05, 1.44)) at lag 0 day, PM10 (0.61% (95%CI: 0.12, 1.11)) and O3 (1.01% (95%CI: 0.24, 1.79)) at lag 0–1 days, and SO2 (9.18% (95%CI: 3.27, 15.42)) and NO2 (3.40% (95% CI:1.64, 5.19)) at lag 0–3 days were observed to be strongly and significantly associated with clinic visits for URTI. PM10 and NO2 were almost still significantly associated with URTI after controlling for the other pollutants in our two-pollutant models, where the effect value of SO2 after inclusion of O3 appeared to be the largest and the effects of NO2 were also obvious compared with the other pollutants. Subgroups analysis demonstrated that males were more vulnerable to PM10 and O3, while females seemed more vulnerable to exposure to SO2 and NO2. This study implied that short-term exposure to ambient air pollution was associated with increased risk of URTI among college students at Wuhan University Hospital in Wuhan, China. And gaseous pollutants had more negative health impact than solid pollutants. SO2 and NO2 were the major air pollutants affecting the daily number of clinic visits on URTI, to which females seemed more vulnerable than males.




Similar content being viewed by others
Availability of data and materials
Not applicable.
References
Aboubakri O, Khanjani N, Jahani Y, Bakhtiari B (2019a) Attributable risk of mortality associated with heat and heat waves: a time-series study in Kerman, Iran during 2005-2017. J Therm Biol 82:76–82
Aboubakri O, Khanjani N, Jahani Y, Bakhtiari B (2019b) The impact of heat waves on mortality and years of life lost in a dry region of Iran (Kerman) during 2005-2017. Int J Biometeorol 63:1139–1149
Aboubakri O, Khanjani N, Jahani Y, Bakhtiari B, Mesgari E (2020) Projection of mortality attributed to heat and cold; the impact of climate change in a dry region of Iran, Kerman. Sci Total Environ 728:138700
Altug H, Gaga EO, Dogeroglu T, Brunekreef B, Hoek G, Van Doorn W (2014) Effects of ambient air pollution on respiratory tract complaints and airway inflammation in primary school children. Sci Total Environ 479-480:201–209
Amarillo AC, Carreras HA (2012) The effect of airborne particles and weather conditions on pediatric respiratory infections in Cordoba, Argentine. Environ Pollut 170:217–221
Brugha R, Grigg J (2014) Urban air pollution and respiratory infections. Paediatr Respir Rev 15:194–199
Cai J, Zhao A, Zhao JZ, Chen RJ, Wang WB, Ha SD, Xu XH, Kan HD (2014) Acute effects of air pollution on asthma hospitalization in Shanghai, China. Environ Pollut 191:139–144
Chai GR, He H, Sha YZ, Zhai GY, Zong SL (2019) Effect of PM2.5 on daily outpatient visits for respiratory diseases in Lanzhou, China. Sci Total Environ 649:1563–1572
Chen RJ, Chu C, Tan JG, Cao JS, Song WM, Xu XH, Jiang C, Ma WJ, Yang CX, Chen BH, Gui YH, Kan HD (2010) Ambient air pollution and hospital admission in Shanghai, China. J Hazard Mater 181:234–240
Chen R, Li T, Cai J, Yan M, Zhao Z, Kan H (2014) Extreme temperatures and out-of-hospital coronary deaths in six large Chinese cities. J Epidemiol Community Health 68:1119–1124
Chen RJ, Yin P, Meng X, Liu C, Wang LJ, Xu XH, Ross JA, Tse LA, Zhao ZH, Kan HD, Zhou MG (2017) Fine particulate air pollution and daily mortality a nationwide analysis in 272 Chinese cities. Am J Respir Crit Care Med 196:73–81
Chen ZJ, Cui LL, Cui XX, Li XW, Yu KK, Yue KS, Dai ZX, Zhou JW, Jia G, Zhang J (2019) The association between high ambient air pollution exposure and respiratory health of young children: a cross sectional study in Jinan, China. Sci Total Environ 656:740–749
Chi R, Li HY, Wang Q, Zhai QR, Wang DD, Wu M, Liu QC, Wu SW, Ma QB, Deng FR, Guo XB (2019) Association of emergency room visits for respiratory diseases with sources of ambient PM2.5. J Environ Sci 86:154–163
Chiu HF, Weng YH, Chiu YW, Yang CY (2017) Short-term effects of ozone air pollution on hospital admissions for myocardial infarction: a time-stratified case-crossover study in Taipei. J Toxicol Environ Health A 80:251–257
Collaborators, G. B. D. Causes of Death (2018) Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392:1736–1788
DALYs GBD, Hale Collaborators (2018) Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392:1859–1922
Darrow LA, Klein M, Flanders WD, Mulholland JA, Tolbert PE, Strickland MJ (2014) Air pollution and acute respiratory infections among children 0-4 years of age: an 18-year time-series study. Am J Epidemiol 180:968–977
Ge EJ, Lai KF, Xiao X, Luo M, Fang ZF, Zeng YJ, Ju H, Zhong NS (2018) Differential effects of size-specific particulate matter on emergency department visits for respiratory and cardiovascular diseases in Guangzhou, China. Environ Pollut 243:336–345
Hill TD, Jorgenson AK, Ore P, Balistreri KS, Clark B (2019) Air quality and life expectancy in the United States: an analysis of the moderating effect of income inequality. Ssm-Popul Health 7:100346
Hwang JS, Chan CC (2002) Effects of air pollution on daily clinic visits for lower respiratory tract illness. Am J Epidemiol 155:1–10
Kan HD, London SJ, Chen GH, Zhang YH, Song GX, Zhao NQ, Jiang LL, Chen BH (2008) Season, sex, age, and education as modifiers of the effects of outdoor air pollution on daily mortality in Shanghai, China: the Public Health and Air Pollution in Asia (PAPA) study. Environ Health Perspect 116:1183–1188
Kim KH, Kabir E, Kabir S (2015) A review on the human health impact of airborne particulate matter. Environ Int 74:136–143
Leitte AM, Petrescu C, Franck U, Richter M, Suciu O, Ionovici R, Herbarth O, Schlink U (2009) Respiratory health, effects of ambient air pollution and its modification by air humidity in Drobeta-Turnu Severin, Romania. Sci Total Environ 407:4004–4011
Li YR, Xiao CC, Li J, Tang J, Geng XY, Cui LJ, Zhai JX (2018) Association between air pollution and upper respiratory tract infection in hospital outpatients aged 0-14 years in Hefei, China: a time series study. Public Health 156:92–100
Liu YW, Xie SG, Yu Q, Huo XX, Ming XY, Wang J, Zhou Y, Peng Z, Zhang H, Cui XQ, Xiang H, Huang XJ, Zhou T, Chen WH, Shi TM (2017) Short-term effects of ambient air pollution on pediatric outpatient visits for respiratory diseases in Yichang city, China. Environ Pollut 227:116–124
Luo LS, Zhang YQ, Jiang JF, Luan HH, Yu CH, Nan PH, Luo B, You M (2018) Short-term effects of ambient air pollution on hospitalization for respiratory disease in Taiyuan, China: a time-series analysis. Int J Environ Res Public Health 15:2160
Ma YX, Xiao BS, Liu C, Zhao YX, Zheng XD (2016) Association between ambient air pollution and emergency room visits for respiratory diseases in spring dust storm season in Lanzhou, China. Int J Environ Res Public Health 13:613
Ma YX, Yang SX, Zhou JD, Yu ZA, Zhou J (2018) Effect of ambient air pollution on emergency room admissions for respiratory diseases in Beijing, China. Atmos Environ 191:320–327
Nhung NTT, Schindler C, Dien TM, Probst-Hensch N, Kunzli N (2019) Association of ambient air pollution with lengths of hospital stay for hanoi children with acute lower-respiratory infection, 2007-2016. Environ Pollut 247:752–762
Peng RD, Dominici F, Louis TA (2006) Model choice in time series studies of air pollution and mortality. J R Stat Soc: Series A (Stats Soc) 169:179–203
Phosri A, Ueda K, Phung VLH, Tawatsupa B, Honda A, Takano H (2019) Effects of ambient air pollution on daily hospital admissions for respiratory and cardiovascular diseases in Bangkok, Thailand. Sci Total Environ 651:1144–1153
Qiu H, Yu HY, Wang LY, Zhu XJ, Chen MD, Zhou L, Deng R, Zhang YL, Pu XR, Pan JP (2018) The burden of overall and cause-specific respiratory morbidity due to ambient air pollution in Sichuan Basin, China: a multi-city time-series analysis. Environ Res 167:428–436
Samoli E, Stergiopoulou A, Santana P, Rodopoulou S, Mitsakou C, Dimitroulopoulou C, Bauwelinck M, de Hoogh K, Costa C, Mari-Dell’Olmo M, Corman D, Vardoulakis S, Katsouyanni K, EURO-HEALTHY Consortium (2019) Spatial variability in air pollution exposure in relation to socioeconomic indicators in nine European metropolitan areas: a study on environmental inequality. Environ Pollut 249:345–353
Schwartz, Joel (2001) Is there harvesting in the association of airborne particles with daily deaths and hospital admissions? Epidemiology 12:55–61
Shou YK, Huang YL, Zhu XZ, Liu CQ, Hu Y, Wang HH (2019) A review of the possible associations between ambient PM2.5 exposures and the development of Alzheimer’s disease. Ecotoxicol Environ Saf 174:344–352
Song J, Lu MX, Lu JG, Chao L, An Z, Liu Y, Xu DQ, Wu WD (2019) Acute effect of ambient air pollution on hospitalization in patients with hypertension: a time-series study in Shijiazhuang, China. Ecotoxicol Environ Saf 170:286–292
Szyszkowicz M, Kousha T, Castner J, Dales R (2018) Air pollution and emergency department visits for respiratory diseases: a multi-city case crossover study. Environ Res 163:263–269
Tam WWS, Wong TW, Ng L, Wong SYS, Kung KKL, Wong AHS (2014) Association between air pollution and general outpatient clinic consultations for upper respiratory tract infections in Hong Kong. PLoS One 9:e86913
Wang XY, Wang WC, Jiao SL, Yuan J, Hu CP, Wang L (2018a) The effects of air pollution on daily cardiovascular diseases hospital admissions in Wuhan from 2013 to 2015. Atmos Environ 182:307–312
Wang YY, Zu YQ, Huang L, Zhang HL, Wang CH, Hu JL (2018b) Associations between daily outpatient visits for respiratory diseases and ambient fine particulate matter and ozone levels in Shanghai, China. Environ Pollut 240:754–763
Winzar H (2015) The ecological fallacy: How to spot one and tips on how to use one to your advantage. Australas Mark J 23:86–92
Wong TW, Tam W, Yu ITS, Wun YT, Wong AHS, Wong CM (2006) Association between air pollution and general practitioner visits for respiratory diseases in Hong Kong. Thorax 61:585–591
Wu SW, Ni Y, Li HY, Pan L, Yang D, Baccarelli AA, Deng FR, Chen YH, Shima M, Guo XB (2016) Short-term exposure to high ambient air pollution increases airway inflammation and respiratory symptoms in chronic obstructive pulmonary disease patients in Beijing, China. Environ Int 94:76–82
Wu C, Hu W, Zhou MJ, Li S, Jia Y (2019) Data-driven regionalization for analyzing the spatiotemporal characteristics of air quality in China. Atmos Environ 203:172–182
Xu C, Kan HD, Fan YN, Chen RJ, Liu JH, Li YF, Zhang Y, Ji AL, Cai TJ (2016) Acute effects of air pollution on enteritis admissions in Xi’an, China. J Toxicol Environ Health A 79:1183–1189
Yu M, Zhu Y, Lin CJ, Wang S, Xing J, Jang C, Huang J, Huang J, Jin J, Yu L (2019) Effects of air pollution control measures on air quality improvement in Guangzhou, China. J Environ Manag 244:127–137
Yunginger JW, Reed CE, Oconnell EJ, Melton LJ, Ofallon WM, Silverstein MD (1992) A community-based study of the epidemiology of asthma-incidence rates, 1964-1983. Am Rev Respir Dis 146:888–894
Zanobetti A, Schwartz J (2009) The effect of fine and coarse particulate air pollution on mortality: a national analysis. Environ Health Perspect 117:898–903
Zeng Q, Wu ZT, Jiang GH, Wu XY, Li P, Ni Y, Xiong XQ, Wang XY, Parasat G, Li X, Pan XC (2017) The association between ambient inhalable particulate matter and the disease burden of respiratory disease: an ecological study based on ten-year time series data in Tianjin, China. Environ Res 157:71–77
Zhu JY, Zhang XH, Zhang X, Dong M, Wu JM, Dong YQ, Chen R, Ding XL, Huang CH, Zhang Q, Zhou WJ (2017) The burden of ambient air pollution on years of life lost in Wuxi, China, 2012-2015: a time-series study using a distributed lag non-linear model. Environ Pollut 224:689–697
Zhu FR, Ding R, Lei RQ, Cheng H, Liu J, Shen CW, Zhang C, Xu YC, Xiao CC, Li XR, Zhang JQ, Cao JY (2019) The short-term effects of air pollution on respiratory diseases and lung cancer mortality in Hefei: a time-series analysis. Respir Med 146:57–65
Author information
Authors and Affiliations
Contributions
Wei Zhu and Dejia Li conceived and designed the study; Chuangxin Wu and Miaoxuan Zhang collected and cleaned the data; Faxue Zhang and Han Zhang performed the data analysis and drafted the manuscript. Huan Feng helped revise the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval
This study was approved by the Ethics Committee of Wuhan University.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Responsible editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 366 kb)
Rights and permissions
About this article
Cite this article
Zhang, F., Zhang, H., Wu, C. et al. Acute effects of ambient air pollution on clinic visits of college students for upper respiratory tract infection in Wuhan, China. Environ Sci Pollut Res 28, 29820–29830 (2021). https://doi.org/10.1007/s11356-021-12828-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-12828-7