Abstract
Purpose
High-intensity interval training (HIIT) and circuit training (CT) are popular methods of exercise, eliciting improvements in cardiorespiratory fitness (CRF). However, direct comparisons of these two training methods are limited. We investigated the effects of HIIT and CT on CRF.
Methods
Thirty-nine apparently healthy middle-aged participants [HIIT; mean age: 42.5 ± 12.3; \(\dot{V}{\text{O}}_{2\hbox{max} }\) 31.5 ± 7.1 (ml kg−1 min−1); 52% males; CT; mean age: 41.2 ± 12.9; \(\dot{V}{\text{O}}_{2\hbox{max} }\) 31.4 ± 6.8 (ml kg−1 min−1); 57% males] were randomly allocated to two sessions per week of HIIT or CT over 8 weeks. HIIT performed ten 1-min cycle-ergometry intervals at > 85% HRmax, separated by ten 1-min intervals of active recovery. The CT group performed up to 40-min of CT at 60–80% HRmax. CRF was measured using maximum oxygen uptake (\(\dot{V}{\text{O}}_{2\hbox{max} }\)), ventilatory anaerobic threshold (\(\dot{V}{\text{O}}_{2}\) at VAT) and maximum oxygen pulse (\(\dot{V}{\text{O}}_{2}\)/HR).
Results
\(\dot{V}{\text{O}}_{2\hbox{max} }\) increased by 12% following HIIT (mean difference 3.9 ml kg−1 min−1; 95% CI: 2.8–4.9; P < 0.001), and 3% in CT (mean difference 1.0 ml kg−1 min−1; 95% CI: − 0.4 to 2.0; P = 0.060). \(\dot{V}{\text{O}}_{2}\) at VAT increased by 16% following HIIT (mean difference 2.4 ml kg−1 min−1; 95% CI: 1.6–3.1; P < 0.001) and 4% in CT (mean difference 0.7 ml kg−1 min−1; 95% CI: − 0.1 to 1.4; P = 0.085). \(\dot{V}{\text{O}}_{2}\)/HR increased by 11% following HIIT (mean difference 1.4 ml beat−1; 95% CI: 0.9–2.0; P < 0.001) and 1% after CT (mean difference 0.3 ml beat−1; 95% CI: − 0.3 to 0.8; P = 0.318).
Conclusion
Our study demonstrated that HIIT led to greater improvements in CRF when compared to CT.
Clinical trial registration
ClinicalTrials.gov Identifier: NCT03700671.
Similar content being viewed by others
Introduction
Regular exercise is well known to have a positive effect on health [1, 2]. Many of these benefits are associated with improving maximal oxygen uptake (\(\dot{V}{\text{O}}_{2\hbox{max} }\)) [3, 4]. Increasing \(\dot{V}{\text{O}}_{2\hbox{max} }\) through exercise training may improve cardiometabolic health, quality of life and increase life-expectancy [4, 5]. Popular training methods aimed at improving \(\dot{V}{\text{O}}_{2\hbox{max} }\) are circuit and high-intensity interval training (HIIT) and are routinely adopted by the general population, health and fitness professionals and researchers [6]. Circuit training (CT) is typically performed at a moderate or high intensity, over a period of 30–50 min and involves a range of aerobic, body weight and resistance exercises with minimal rest [7, 8]. Low-volume HIIT is defined as ‘brief, intermittent bursts of vigorous activity, interspersed by periods of rest or low intensity exercise’ [9], typically prescribed at a training intensity between 80 and 100% of heart rate maximum (HRmax) [10].
Whole-body CT and low-volume HIIT consisting of 8–12 1-min interval bouts, interspersed with a similar recovery time have been shown to improve cardiometabolic health and cardiorespiratory fitness (CRF) [8, 11,12,13,14,15,16]. Increases in \({\dot{\text{V}}\text{O}}_{2\hbox{max} }\) and the anaerobic threshold (AT) have been observed following CT; however, published studies are limited to sedentary and older populations, with further markers of CRF not fully explored [8, 17]. Comparable improvements in \(\dot{V}{\text{O}}_{2\hbox{max} }\) and the AT have been shown following low-volume HIIT, with increases in maximum oxygen pulse (\(\dot{V}{\text{O}}_{2}\)/HR) also observed [16, 18, 19]. However, there is limited evidence directly comparing both training methods across a range of CRF markers, as such it is unknown which approach is most beneficial [20, 21].
Direct comparisons have been made investigating low-volume HIIT and moderate-intensity continuous training (MICT), which is typically 30–60 min in duration adopting the same modality of exercise [14,15,16]. The results demonstrate low-volume HIIT to be a time-efficient method, eliciting greater improvements in \(\dot{V}{\text{O}}_{2\hbox{max} }\), although these findings are not consistently shown [22].
While HIIT and CT are feasible and effective at improving CRF, no study has directly investigated the two. Therefore, the aim of this study was to compare the effect of two weekly sessions of low-volume HIIT and CT over an 8-week period on \(\dot{V}{\text{O}}_{2\hbox{max} }\) in apparently healthy middle-aged adults. We also investigated changes in other markers of CRF such as the first ventilatory anaerobic threshold (\(\dot{V}{\text{O}}_{2}\) at VAT) and maximum \(\dot{V}{\text{O}}_{2}\)/HR. Intervention fidelity was also evaluated. We hypothesised that HIIT would elicit superior improvements in \(\dot{V}{\text{O}}_{2\hbox{max} }\) and additional markers of CRF.
Methods
Study design
Participants were enrolled in a randomised control trial at the University of Hull to either 8 weeks of HIIT or CT (two supervised sessions per week, accompanied by an exercise physiologist). A sample size of 38 using G*Power 3.1 software was calculated based on previously published data in which the mean difference between HIIT and MICT was 3.2 ml kg−1 min−1 with a pooled standard deviation of 3 ml kg−1 min−1 [19]. Statistical significance was set at α = 0.05 and power set to 0.95. To allow for 10% attrition 42 individuals were recruited to the study. To assess the effectiveness of the interventions as determined by \(\dot{V}{\text{O}}_{2\hbox{max} }\), a maximal cardiopulmonary exercise test (CPET) to volitional exhaustion on an electronically braked cycle ergometer at baseline (visit one), and following an 8-week exercise intervention of HIIT or CT (visit two) was conducted. When attending the assessments participants were asked not to take part in any strenuous exercise 24 h prior to the appointment, to wear suitable comfortable clothing and avoid a large meal. For visit two, CPET was performed within 6 days of completing the exercise interventions. A thorough warm-up and cool down were before and after each exercise session. All were asked to maintain their habitual physical activity patterns during the intervention. Body mass index (BMI) was calculated by dividing body weight [23] by height in meters squared and was presented as kg m−2. Resting blood pressure was measured after 15 min of rest using a sphygmomanometer (A.C. Cossor & Son Ltd, London UK) and stethoscope (3 M Healthcare, St Paul, MN). To provide a comprehensive account of the study the Consensus on Exercise Reporting Template (CERT) was consulted [24].
Participants
Ethical approval was provided by the School of Life Sciences ethics committee at the University of Hull which was in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. A total of 42 apparently healthy men and women between the age of 18–65 years were recruited to the study. Participant characteristics are given in Table 1. Enrolled individuals reported no medical history of cardiometabolic or limiting respiratory disease, were non-smokers, had a body mass index < 30 kg m−2, classified as recreationally active [25] and none were taking any medication that would affect heart rate. A condition of enrolment for those over 45 years was to obtain written medical clearance from a general practitioner and undergo resting and exercise 12-lead electrocardiogram (ECG) (GE Healthcare, Chalfont St Giles, United Kingdom). Written informed consent and a pre-exercise medical questionnaire were completed by all.
Cardiopulmonary exercise testing
Maximal CPETs were conducted in accordance with the American Thoracic Society (ATS) and the American College of Chest Physicians (ACCP) guidelines [26]. An Oxycon pro (Jaeger, Hoechburg, Germany) breath-by-breath metabolic cart was used to collect respiratory gas exchange data. Automatic and manual calibration evaluated ambient temperature, humidity, barometric pressure and altitude. Calibration of the air flow volume was conducted using a 3 l syringe and by automatic calibration. Two-point gas calibration was also conducted to ensure accurate measures of inspired O2 and expired CO2 [27]. Tests were performed on a GE e-bike ergometer (GE Healthcare, Buckinghamshire, UK) using a ramp protocol [26]. The protocol consisted of a 3-min rest phase, 3 min of unloaded cycling, followed by a personalised ramp test [28] (ramp rate ranged between 15 and 30 W) with work rate continually increased every 1–3 s. Participants performed the same ramp rate pre- and post-testing. Participants were asked to pedal at a cadence of 70 rpm until they reached volitional exhaustion at a protocol duration between 8 and 12 min. Self-reported rating of perceived exertion (RPE) scores using the 6–20 scale [29] and heart rate (HR) (FT1 heart rate monitor, Polar Electro, OY, Finland) was recorded during the last 5 s of each minute of the test, at maximum exercise and during the recovery period. Together with verbal encouragement to volitional exhaustion, \(\dot{V}{\text{O}}_{2\hbox{max} }\) was attained by participants achieving at least two of the following criteria: \(\dot{V}{\text{O}}_{2}\) plateau as determined by a failure of \(\dot{V}{\text{O}}_{2}\) increase by 150 ml min−1 with further increases in workload analysed by breath-by-breath gas exchange data averaged over 15 s [30], respiratory exchange ratio (RER) > 1.10, achieve > 85% age predicated HRmax and a RPE > 17 on the 6–20 Borg scale [27]. \(\dot{V}{\text{O}}_{2}\) at VAT was defined using the ‘V slope’ method [31] and verified using ventilatory equivalents. Peak power output (PPO) (watts) and HRmax were defined as the highest value achieved during the CPET with maximum \(\dot{V}{\text{O}}_{2}\)/HR determined by the ratio of \(\dot{V}{\text{O}}_{2\hbox{max} }\) and HRmax.
Training interventions
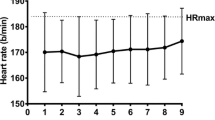
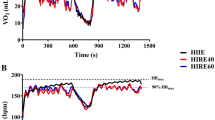
The HIIT group was asked to perform ten 1-min HIIT intervals, each followed by 1 min of active recovery (AR) (total exercise time 20 min). Resulting from the CPET, HIIT was set at > 85% HRmax with a specific HR designated for this criterion. Active recovery was set at a load corresponding to 25–50 W. Sessions were performed on a Wattbike trainer (Wattbike Ltd, Nottingham, UK). The CT group completed a practical seven-station mixed-modality exercise circuit (cycle ergometer, rower, treadmill, sit to stand/squats, knee to elbow and leg kickback with bicep curl) at an intensity of 60–80% HRmax (calculated from CPET). No resistance equipment was involved, only body weight. Participants initially performed 20 min of CT with duration increased by 5 min per week until the desired 40 min. Each station was occupied for 3–6 minutes depending on session duration, moving from one station to the next with minimal rest. During both interventions, HR was measured in last 5 s of each station/interval using a FT1 polar heart rate monitor (Polar Electro, OY, Finland) with each CT session timed using a stop watch (Axprod S.L, Guipuzcoa, Spain). Intensity for both interventions was adjusted throughout by the investigator to ensure an appropriate HR range and successful completion of the protocol. Participants were made aware of their HR ranges and verbal encouragement was given by the physiologist to help achieve and maintain these thresholds. Energy expenditure between HIIT and CT was not matched.
To assess the validity of the exercise interventions, participant fidelity to the desired exercise intensity was determined using cut points of > 85% HRmax and 60–80% HRmax for HIIT and CT, respectively, and reported using previous examples [32, 33]. These values were calculated using the participants’ mean heart rate for each individual interval or station over the 16 sessions and was expressed as a percentage of HRmax as determined by CPET at visit 1. Specific fidelity thresholds were consulted to determine low (< 50%), moderate (50–70%), and high (> 70%) compliance [34]. Adherence was determined as a percentage of completed sessions, with 14 (> 85%) being the threshold for completion.
Statistical analysis
Statistical analysis was conducted using SPSS version 24 (IBM, New York, USA). An independent t test was used to identify group differences at baseline. Assumptions of normality were verified using the Shapiro–Wilk test. Skewness and kurtosis of distribution were visually examined. Non-normally distributed data were presented as median and interquartile range (IQR). A two-way (condition × time) repeated-measures analysis of variance (ANOVA) was used to compare CRF pre-and post-training. Post-hoc analysis for the main effects and interactions was assessed using a Bonferroni adjustment. Group differences were compared using independent t tests. Variables were displayed as mean with 95% confidence intervals (95% CI) or standard deviation (±) where specified. Partial eta squared (η 2p ) effect sizes were also calculated with 0.01, 0.06 and 0.14 representing small, medium, and large effect sizes, respectively [35].
Results
Of the 78 CPETs, (pre and post) 95% of participants achieved a plateau in \(\dot{V}{\text{O}}_{2}\) with all achieving at least two of the desired criteria for maximum effort. Three participants dropped out; one from the HIIT group and two from the CT group (work commitments and an injury unrelated to exercise). The mean training intensities for HIIT were 94 ± 4% HRmax and 76 ± 3% HRmax for CT. The mean exercise duration for the CT group was 32 ± 4 min (P < 0.001 versus HIIT) which corresponded to 60% greater training duration. The proportion of intervals/stations achieving the desired intensity criterion was 90% (IQR 10%) for the LV-HIIT group and 86% (IQR 28.5%) for CT (Fig. 1). Overall adherence for HIIT and CT was 95.2% and 90.5%, respectively, with 32 participants having 100% attendance. No adverse events occurred during the exercise sessions.
Low-volume HIIT versus circuit training
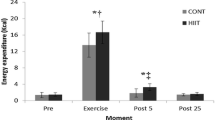
There was a significant main effect for time for \(\dot{V}{\text{O}}_{2\hbox{max} }\) (mean difference 2.4 ml kg−1 min−1; 95% CI: 1.7–3.2; P < 0.001; η 2p = 0.554) and interaction effect (P < 0.001; η 2p = 0.302). \(\dot{V}{\text{O}}_{2\hbox{max} }\) significantly increased (Fig. 2a) in the HIIT group by 12% (mean difference 3.9 ml kg−1 min−1; 95% CI: 2.8–4.9; P < 0.001; η 2p = 0.600) but not in the CT group (3% increase; mean difference 1.0 ml kg−1 min−1; 95% CI: − 0.4 to 2.0; P = 0.060; η 2p = 0.092). HIIT significantly increased \(\dot{V}{\text{O}}_{2\hbox{max} }\) to greater extent than CT (mean difference 2.9 ml kg−1 min−1; 95% CI: 1.4–4.3; P < 0.001).
Maximal oxygen consumption (\(\dot{V}{\text{O}}_{2\hbox{max} }\)) (a) and VAT (b) Δ after 8 weeks of HIIT (n = 20) and CT (n = 19). Black lines correspond to individual responses. \(\dot{V}{\text{O}}_{2}\) oxygen uptake, VAT ventilatory anaerobic threshold, HIIT low-volume high-intensity interval training, CT circuit training. *P < 0.001 versus baseline
There was a significant main effect for time for \(\dot{V}{\text{O}}_{2}\) at VAT (mean difference 1.5 ml kg−1 min−1; 95% CI: 1.0–2.1; P < 0.001; η 2p = 0.474) and interaction effect (P < 0.05; η 2p = 0.222). \(\dot{V}{\text{O}}_{2}\) at VAT significantly increased (Fig. 2b) by 16% after HIIT (mean difference 2.4 ml kg−1 min−1; 95% CI: 1.6–3.1; P < 0.001; η 2p = 0.531) with no notable changes observed in the CT group (4% increase; mean difference 0.7 ml kg−1 min−1; 95% CI: − 0.1 to 1.4; P = 0.085; η 2p = 0.078).
There was a significant main effect for time for maximum \(\dot{V}{\text{O}}_{2}\)/HR (mean difference 0.8 ml beat−1; 95% CI: 0.5–1.2; P < 0.001; η 2p = 0.342) and interaction effect (P < 0.05; η 2p = 0.189). Maximum \(\dot{V}{\text{O}}_{2}\)/HR significantly increased in the HIIT group by 11% (mean difference 1.4 ml beat−1; 95% CI: 0.9–2.0; P < 0.001; η 2p = 0.428) but not in CT (1% increase; mean difference 0.3 ml beat−1; 95% CI: − 0.3 to 0.8; P = 0.318; η 2p = 0.027). Both groups increased PPO, HITT by 14% (mean difference 27 watts; 95% CI: 19.2–34.3; P < 0.001; η 2p = 0.601) and CT by 6% (mean difference 11.7 W; 95% CI: 4.2–19.2; P < 0.01; η 2p = 0.213). HRmax and BMI were unaffected.
Discussion
The present investigation has evaluated the effects of HIIT and CT in apparently healthy middle-aged adults. Our results show that HIIT performed at 94% HRmax elicited a greater increase in \(\dot{V}{\text{O}}_{2\hbox{max} }\), \(\dot{V}{\text{O}}_{2}\) at VAT and \(\dot{V}{\text{O}}_{2}\)/HR when compared to CT (76% HRmax), despite 60% less training duration. Further, intervention fidelity was high in both interventions demonstrating excellent delivery of HIIT and CT, as well as its receipt and enactment by the participants.
Our results support previous research highlighting a greater increase in \(\dot{V}{\text{O}}_{2\hbox{max} }\) following 1:1 work/rest ratio HIIT, even when performed at lower weekly doses compared to existing literature [14, 16, 36]. As such the results highlight the role of intensity as an important factor to induce CRF adaptation [9]. In contrast, previous studies and meta-analyses have shown that low-volume HIIT is not superior than MICT in improving \(\dot{V}{\text{O}}_{2\hbox{max} }\), eliciting similar changes [13, 15, 22, 37, 38]. However, these findings may be explained by the heterogeneous nature of the study populations and HIIT protocols prescribed. Our results are in agreement with previous studies which indicate a total of 64 min per week of MICT may be insufficient to provoke adaptions [39]. However, previous findings have shown increases in \(\dot{V}{\text{O}}_{2\hbox{max} }\) following CT when performed at higher doses [8, 20]. Thus, the trivial improvement in \(\dot{V}{\text{O}}_{2\hbox{max} }\) in the CT group may be due to the small volume of CT prescribed.
The increase in \(\dot{V}{\text{O}}_{2\hbox{max} }\) may be of clinical relevance given that \(\dot{V}{\text{O}}_{2\hbox{max} }\) is a strong prognostic marker of all-cause and cardiovascular mortality and improving \(\dot{V}{\text{O}}_{2\hbox{max} }\) is associated with a reduction in mortality and cardiometabolic risk [3, 40]. Indeed, for every 3.5 ml kg−1 min−1 increase in \(\dot{V}{\text{O}}_{2\hbox{max} }\) there has been shown an 8–35% reduction in all-cause mortality and cardiovascular disease risk [3, 41]. As such, our findings suggest that HIIT may be a time-efficient and efficacious approach at inducing clinical meaningful benefits when compared to other popular training methods.
The present study showed that HIIT alone, significantly increased \(\dot{V}{\text{O}}_{2}\) at VAT, which is in agreement with previous studies [18]. In contrast, CT has been shown to increase the lactate threshold [17] when performed at higher doses, while a similar low-volume HIIT protocol to the current study reported improvements in \(\dot{V}{\text{O}}_{2}\) at VAT following both HIIT and MICT [37]. While this was time efficient, the relative training intensities of both groups were similar. Thus, the improvements in \(\dot{V}{\text{O}}_{2}\) at VAT in the present study are likely due to the greater stimulus provided by HIIT. As such, HIIT consisting of two weekly sessions may be sufficient at inducing metabolic adaptations in skeletal muscle, enabling higher doses of exercise to be performed before lactate accumulation, thus becoming ‘physiologically efficient’ [42].
In agreement with previous research [16] our results showed that HIIT increased maximum \(\dot{V}{\text{O}}_{2}\)/HR to a greater extent than CT, a surrogate marker of stroke volume (SV) and arteriovenous O2 difference. This is in contrast to recent findings [15]. Increases in maximum \(\dot{V}{\text{O}}_{2}\)/HR are strongly correlated to an increase in SV [43]. While we did not directly measure SV or analyse muscle tissue our findings may support previous data which indicated low-volume HIIT to be an optimal approach for inducing cardiovascular adaptations [44]. Studies adopting a similar low-volume HIIT protocol to the current study have shown increases in mitochondrial oxidative capacity [45, 46], while lower and higher volumes of HIIT have shown to be superior or comparable to MICT at increasing cardiac output and SV [47, 48]. While this is a positive finding from our results, further studies are required to confirm the mechanisms associated with an improvement in \(\dot{V}{\text{O}}_{2\hbox{max} }\) following a low-volume HIIT protocol consisting of a 1:1 work/rest ratio.
As well as reporting the attendance and mean exercise data, assessing if participants have performed the exercise training as intended is crucial when evaluating exercise interventions. Indeed, in the absence of evaluating intervention fidelity, incorrect conclusions, positive or negative, may be drawn about the effect of HIIT on a given outcome [49]. Using the pre-specified cut points for exercise intensity, 90% of the HIIT intervals and 86% of the CT stations met the criterion, indicating high fidelity to the interventions. Previous HIIT studies have reported low-to-moderate fidelity with compliance ranging between 23 and 63% [32, 34, 50]. The high levels of fidelity in the present study may be attributed to a number of factors. Firstly, the participants were healthy adults, they were made aware of their target HR each session and were given verbal encouragement to reach these targets. Secondly, the chosen HIIT protocol in the present study may be more practical and less physically demanding [51]. High-volume HIIT protocols, or low-volume HIIT protocols involving ‘all out’ maximal effort (sprint interval training) may cause psychobiological stress, meaning that high levels of motivation are required to complete the protocol [52].
The failure to report fidelity, and the general inadequate reporting of exercise interventions is a major concern. With exercise intensity typically reported as a ranged based or as a general mean, this has inherent limitations. The authors strongly advocate that the CERT checklist [24] be adopted for future exercise studies as it provides reporting standards that ensures quality and transparency. As a result, exercise interventions may be clearly interpreted, translated, and implemented into practice.
There are a number of limitations that should be considered regarding this study. Not all participants achieved a \(\dot{V}{\text{O}}_{2}\) plateau during CPET as such secondary criteria was used which has established limitations. In addition, participants were not habituated to the CPET or the exercise sessions prior to starting the interventions. This may be relevant to novice or nervous participants in which familiarisation may be beneficial to obtain accurate measures. However, the use of strict criteria (i.e., a \(\dot{V}{\text{O}}_{2}\) plateau and heart rate) was met. Furthermore, laboratory-based studies investigating HIIT and MICT typically adopt the same modality of exercise and a similar or higher volume of training. While this is relevant regarding specificity of training, our aim was to assess two different low-volume training methods.
Finally, for safety and accuracy of exercise prescription a maximal CPET was performed by all participants. However, access to specialised equipment may not always be feasible which may limit HIIT prescription in a “real world” setting. However, the present HIIT protocol appears well tolerated and safe, therefore further studies are required to evaluate the feasibility to adopt this protocol without a prior maximal CPET in healthy adults.
Conclusion
Our study demonstrated that HIIT is superior to CT, inducing larger improvements in CRF in apparently healthy middle-aged adults. Moreover, the present data provide evidence that 40 min per week of HIIT is sufficient to elicit clinical meaningful increases in \(\dot{V}{\text{O}}_{2}\). Furthermore, 64 min of CT per week appears not to provide sufficient stimulus to evoke CRF adaptation in this population. More broadly, this study provides further indication that HIIT and CT are a practical and effective approach to exercise training in healthy middle-aged adults given the high fidelity.
Abbreviations
- \(\dot{V}{\text{O}}_{2\hbox{max} }\) :
-
Maximal oxygen uptake
- CPET:
-
Cardiopulmonary exercise test
- HIIT:
-
High-intensity interval training
- HRmax :
-
Heart rate maximum
- MICT:
-
Moderate-intensity continuous training
- CRF:
-
Cardiorespiratory fitness
- ECG:
-
Electrocardiogram
- VAT:
-
Ventilatory anaerobic threshold
- BMI:
-
Body mass index
- RER:
-
Respiratory exchange ratio
- \(\dot{V}{\text{O}}_{2}\)/HR:
-
Oxygen pulse
- HR:
-
Heart rate
- ±:
-
Standard deviation
- CERT:
-
Consensus on exercise reporting template
- RPE:
-
Rating of perceived exertion
- ANOVA:
-
Analysis of variance
- 95% CI:
-
95% confidence intervals
- η 2p :
-
Partial eta squared
- SV:
-
Stroke volume
- PPO:
-
Peak power output
- IQR:
-
Interquartile range
- AT:
-
Anaerobic threshold
References
Blair SN, Morris JN (2009) Healthy hearts—and the universal benefits of being physically active: physical activity and health. Ann Epidemiol 19(4):253–256. https://doi.org/10.1016/j.annepidem.2009.01.019
Blair SN, Kohl HW 3rd, Paffenbarger RS Jr, Clark DG, Cooper KH, Gibbons LW (1989) Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA 262(17):2395–2401
Ross R, Blair SN, Arena R, Church TS, Despres JP, Franklin BA, Haskell WL, Kaminsky LA, Levine BD, Lavie CJ, Myers J, Niebauer J, Sallis R, Sawada SS, Sui X, Wisloff U (2016) Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the american heart association. Circulation 134(24):e653–e699. https://doi.org/10.1161/cir.0000000000000461
Lee D-C, Artero EG, Sui X, Blair SN (2010) Mortality trends in the general population: the importance of cardiorespiratory fitness. J Psychopharmacol 24(4_supplement):27–35. https://doi.org/10.1177/1359786810382057 (Oxford, England)
Kaminsky LA, Arena R, Beckie TM, Brubaker PH, Church TS, Forman DE, Franklin BA, Gulati M, Lavie CJ, Myers J, Patel MJ, Pina IL, Weintraub WS, Williams MA (2013) The importance of cardiorespiratory fitness in the United States: the need for a national registry: a policy statement from the American Heart Association. Circulation 127(5):652–662. https://doi.org/10.1161/CIR.0b013e31827ee100
Thompson WR (2018) Worldwide survey of fitness trends for 2019. ACSM’s Health Fit J 22(6):10–17. https://doi.org/10.1249/fit.0000000000000438
Paoli A, Pacelli F, Bargossi AM, Marcolin G, Guzzinati S, Neri M, Bianco A, Palma A (2010) Effects of three distinct protocols of fitness training on body composition, strength and blood lactate. J Sports Med Phys Fit 50(1):43–51
Myers TR, Schneider MG, Schmale MS, Hazell TJ (2015) Whole-body aerobic resistance training circuit improves aerobic fitness and muscle strength in sedentary young females. J Strength Cond Res 29(6):1592–1600. https://doi.org/10.1519/jsc.0000000000000790
Gibala MJ, Little JP, Macdonald MJ, Hawley JA (2012) Physiological adaptations to low-volume, high-intensity interval training in health and disease. J Physiol 590(Pt 5):1077–1084. https://doi.org/10.1113/jphysiol.2011.224725
Weston KS, Wisløff U, Coombes JS (2014) High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: a systematic review and meta-analysis. Br J Sports Med 48(16):1227–1234. https://doi.org/10.1136/bjsports-2013-092576
Paoli A, Pacelli QF, Moro T, Marcolin G, Neri M, Battaglia G, Sergi G, Bolzetta F, Bianco A (2013) Effects of high-intensity circuit training, low-intensity circuit training and endurance training on blood pressure and lipoproteins in middle-aged overweight men. Lipids Health Dis 12(1):131. https://doi.org/10.1186/1476-511x-12-131
Weston KS, Wisløff U, Coombes JS (2014) High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: a systematic review and meta-analysis. Br J Sports Med 48(16):1227–1234 1228p. https://doi.org/10.1136/bjsports-2013-092576
Sawyer BJ, Tucker WJ, Bhammar DM, Ryder JR, Sweazea KL, Gaesser GA (2016) Effects of high-intensity interval training and moderate-intensity continuous training on endothelial function and cardiometabolic risk markers in obese adults. J Appl Physiol 121(1):279–288. https://doi.org/10.1152/japplphysiol.00024.2016
Esfandiari S, Sasson Z, Goodman JM (2014) Short-term high-intensity interval and continuous moderate-intensity training improve maximal aerobic power and diastolic filling during exercise. Eur J Appl Physiol 114(2):331–343. https://doi.org/10.1007/s00421-013-2773-x
Baekkerud FH, Solberg F, Leinan IM, Wisloff U, Karlsen T, Rognmo O (2016) Comparison of three popular exercise modalities on V O2max in overweight and obese. Med Sci Sports Exerc 48(3):491–498. https://doi.org/10.1249/mss.0000000000000777
Boyd JC, Simpson CA, Jung ME, Gurd BJ (2013) Reducing the intensity and volume of interval training diminishes cardiovascular adaptation but not mitochondrial biogenesis in overweight/obese men. PLoS One 8(7):e68091. https://doi.org/10.1371/journal.pone.0068091
Takeshima N, Rogers ME, Islam MM, Yamauchi T, Watanabe E, Okada A (2004) Effect of concurrent aerobic and resistance circuit exercise training on fitness in older adults. Eur J Appl Physiol 93(1–2):173–182. https://doi.org/10.1007/s00421-004-1193-3
Ziemann E, Grzywacz T, Luszczyk M, Laskowski R, Olek RA, Gibson AL (2011) Aerobic and anaerobic changes with high-intensity interval training in active college-aged men. J Strength Cond Res 25(4):1104–1112. https://doi.org/10.1519/JSC.0b013e3181d09ec9
Matsuo T, Saotome K, Seino S, Eto M, Shimojo N, Matsushita A, Iemitsu M, Ohshima H, Tanaka K, Mukai C (2014) Low-volume, high-intensity, aerobic interval exercise for sedentary adults: $$\dot{V}$$ O, cardiac mass, and heart rate recovery. Eur J Appl Physiol 114(9):1963–1972
McRae G, Payne A, Zelt JGE, Scribbans TD, Jung ME, Little JP, Gurd BJ (2012) Extremely low volume, whole-body aerobic-resistance training improves aerobic fitness and muscular endurance in females. Appl Physiol Nutr Metab 37(6):1124–1131. https://doi.org/10.1139/h2012-093
McGregor G, Nichols S, Hamborg T, Bryning L, Tudor-Edwards R, Markland D, Mercer J, Birkett S, Ennis S, Powell R, Begg B, Haykowsky MJ, Banerjee P, Ingle L, Shave R, Backx K (2016) High-intensity interval training versus moderate-intensity steady-state training in UK cardiac rehabilitation programmes (HIIT or MISS UK): study protocol for a multicentre randomised controlled trial and economic evaluation. BMJ Open 6(11):e012843. https://doi.org/10.1136/bmjopen-2016-012843
Weston M, Taylor K, Batterham A, Hopkins W (2014) Effects of low-volume high-intensity interval training (HIT) on fitness in adults: a meta-analysis of controlled and non-controlled trials. Sports Med 44(7):1005–1017. https://doi.org/10.1007/s40279-014-0180-z
Nordestgaard BG, Chapman MJ, Ray K, Boren J, Andreotti F, Watts GF, Ginsberg H, Amarenco P, Catapano A, Descamps OS, Fisher E, Kovanen PT, Kuivenhoven JA, Lesnik P, Masana L, Reiner Z, Taskinen MR, Tokgozoglu L, Tybjaerg-Hansen A, European Atherosclerosis Society Consensus P (2010) Lipoprotein(a) as a cardiovascular risk factor: current status. Eur Heart J 31(23):2844–2853. https://doi.org/10.1093/eurheartj/ehq386
Slade SC, Dionne CE, Underwood M, Buchbinder R (2016) Consensus on exercise reporting template (CERT): explanation and elaboration statement. Br J Sports Med 50:1428–1437
Bolgar MR, Baker CE, Goss FL, Nagle E, Robertson RJ (2010) Effect of exercise intensity on differentiated and undifferentiated ratings of perceived exertion during cycle and treadmill exercise in recreationally active and trained women. J Sports Sci Med 9(4):557–563
Ross RM (2003) ATS/ACCP statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med 167(10):1451. https://doi.org/10.1164/ajrccm.167.10.950 (author reply 1451)
Balady GJ, Arena R, Sietsema K, Myers J, Coke L, Fletcher GF, Forman D, Franklin B, Guazzi M, Gulati M, Keteyian SJ, Lavie CJ, Macko R, Mancini D, Milani RV, American Heart Association Exercise CR, Prevention Committee of the Council on Clinical C, Council on E, Prevention, Council on Peripheral Vascular D, Interdisciplinary Council on Quality of C, Outcomes R (2010) Clinician’s guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation 122(2):191–225. https://doi.org/10.1161/cir.0b013e3181e52e69
Wasserman K, Hansen J, Sue D, Stringer W, Sietsema K, Sun X-G, Whipp B (2011) Principles of exercise testing and interpretation: including pathophysiology and clinical applications, 5th edn. Lippincott Williams & Wilkins, Philadelphia
Borg GA (1982) Psychophysical bases of perceived exertion. Med Sci Sports Exerc 14(5):377–881
Astorino TA (2009) Alterations in VOmax and the VO plateau with manipulation of sampling interval. Clin Physiol Funct Imaging 29(1):60–67. https://doi.org/10.1111/j.1475-097X.2008.00835.x
Beaver WLWK, Whipp BJ (1986) A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol 60:2020–2027
Taylor KL, Weston M, Batterham AM (2015) Evaluating intervention fidelity: an example from a high-intensity interval training study. PLoS One 10(4):e0125166. https://doi.org/10.1371/journal.pone.0125166
Weston M, Batterham AM, Tew GA, Kothmann E, Kerr K, Nawaz S, Yates D, Danjoux G (2017) Patients awaiting surgical repair for large abdominal aortic aneurysms can exercise at moderate to hard intensities with a low risk of adverse events. Front Physiol 7:684. https://doi.org/10.3389/fphys.2016.00684
Hurst C, Weston KL, Weston M (2018) The effect of 12 weeks of combined upper- and lower-body high-intensity interval training on muscular and cardiorespiratory fitness in older adults. Aging Clin Exp Res. https://doi.org/10.1007/s40520-018-1015-9
Richardson JTE (2011) Eta squared and partial eta squared as measures of effect size in educational research. Educ Res Rev 6(2):135–147. https://doi.org/10.1016/j.edurev.2010.12.001
Stavrinou PS, Bogdanis GC, Giannaki CD, Terzis G, Hadjicharalambous M (2018) High-intensity interval training frequency: cardiometabolic effects and quality of life. Int J Sports Med 39(3):210–217. https://doi.org/10.1055/s-0043-125074
Currie KD, Dubberley JB, McKelvie RS, MacDonald MJ (2013) Low-volume, high-intensity interval training in patients with CAD. Med Sci Sports Exerc 45(8):1436–1442. https://doi.org/10.1249/MSS.0b013e31828bbbd4
McKay BR, Paterson DH, Kowalchuk JM (2009) Effect of short-term high-intensity interval training vs continuous training on O2 uptake kinetics, muscle deoxygenation, and exercise performance. J Appl Physiol 107(1):128–138. https://doi.org/10.1152/japplphysiol.90828.2008
Montero D, Lundby C (2017) Refuting the myth of non-response to exercise training: ‘non-responders’ do respond to higher dose of training. J Physiol 595(11):3377–3387. https://doi.org/10.1113/jp273480
Ingle L, Mellis M, Brodie D, Sandercock GR (2016) Associations between cardiorespiratory fitness and the metabolic syndrome in British men. Heart. https://doi.org/10.1136/heartjnl-2016-310142
Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Asumi M, Sugawara A, Totsuka K, Shimano H, Ohashi Y, Yamada N, Sone H (2009) Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA 301(19):2024–2035. https://doi.org/10.1001/jama.2009.681
Ghosh AK (2004) Anaerobic threshold: its concept and role in endurance sport. Malays J Med Sci 11(1):24–36
Bhambhani Y, Norris S, Bell G (1994) Prediction of stroke volume from oxygen pulse measurements in untrained and trained men. Can J Appl Physiol 19(1):49–59
Daussin FN, Ponsot E, Dufour SP, Lonsdorfer-Wolf E, Doutreleau S, Geny B, Piquard F, Richard R (2007) Improvement of VO2max by cardiac output and oxygen extraction adaptation during intermittent versus continuous endurance training. Eur J Appl Physiol 101(3):377–383. https://doi.org/10.1007/s00421-007-0499-3
Hood MS, Little JP, Tarnopolsky MA, Myslik F, Gibala MJ (2011) Low-volume interval training improves muscle oxidative capacity in sedentary adults. Med Sci Sports Exerc 43(10):1849–1856. https://doi.org/10.1249/MSS.0b013e3182199834
Little JP, Safdar A, Wilkin GP, Tarnopolsky MA, Gibala MJ (2010) A practical model of low-volume high-intensity interval training induces mitochondrial biogenesis in human skeletal muscle: potential mechanisms. J Physiol 588(Pt 6):1011–1022. https://doi.org/10.1113/jphysiol.2009.181743
Astorino TA, Edmunds RM, Clark A, King L, Gallant RM, Namm S, Fischer A, Wood KA (2016) High-intensity interval training increases cardiac output and VO2max. Med Sci Sports Exerc 5:6656. https://doi.org/10.1249/mss.0000000000001099
Helgerud J, Hoydal K, Wang E, Karlsen T, Berg P, Bjerkaas M, Simonsen T, Helgesen C, Hjorth N, Bach R, Hoff J (2007) Aerobic high-intensity intervals improve VO2max more than moderate training. Med Sci Sports Exerc 39(4):665–671. https://doi.org/10.1249/mss.0b013e3180304570
Fortington LV, Donaldson A, Lathlean T, Young WB, Gabbe BJ, Lloyd D, Finch CF (2015) When ‘just doing it’ is not enough: assessing the fidelity of player performance of an injury prevention exercise program. J Sci Med Sport 18(3):272–277. https://doi.org/10.1016/j.jsams.2014.05.001
Weston M, Batterham AM, Tew GA, Kothmann E, Kerr K, Nawaz S, Yates D, Danjoux G (2016) Patients awaiting surgical repair for large abdominal aortic aneurysms can exercise at moderate to hard intensities with a low risk of adverse events. Front Physiol 7:684. https://doi.org/10.3389/fphys.2016.00684
Gibala MJ, Little JP, Macdonald MJ, Hawley JA (2012) Physiological adaptations to low-volume, high-intensity interval training in health and disease. J Physiol 590(5):1077–1084. https://doi.org/10.1113/jphysiol.2011.224725
Hardcastle SJ, Ray H, Beale L, Hagger MS (2014) Why sprint interval training is inappropriate for a largely sedentary population. Front Psychol 5:1505. https://doi.org/10.3389/fpsyg.2014.01505
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
Ethical approval for the study was given by the School of Life Sciences ethics committee at the University of Hull.
Informed consent
Written consent was obtained by all.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Birkett, S.T., Nichols, S., Sawrey, R. et al. The effects of low-volume high-intensity interval training and circuit training on maximal oxygen uptake. Sport Sci Health 15, 443–451 (2019). https://doi.org/10.1007/s11332-019-00552-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11332-019-00552-2