Abstract
Objective
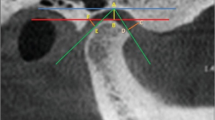
We examined the bone components of the temporomandibular joint (TMJ) in asymptomatic individuals and patients with temporomandibular dysfunction (TMD) using cone-beam computed tomography (CBCT).
Methods
Two hundred asymptomatic individuals and 200 patients with TMD were included in this study. Condyle position, eminence height, eminence inclination, condyle shape, and fossa shape were assessed on CBCT images of the 800 temporomandibular joints.
Results
The eminence inclination (P < 0.05), eminence height (P < 0.0001), mediolateral width of condyle (P < 0.0001), and anterior joint space (P < 0.0001) were significantly greater in male subjects compared with female subjects in both the asymptomatic group and TMD group. Comparisons of the asymptomatic group and TMD group revealed significant differences in the anterior joint space (P < 0.0001), ratio of anterior joint space to posterior joint space (P < 0.001), posterior joint space (P < 0.05), eminence inclination (P < 0.05), eminence height (P < 0.05), condyle shape (P < 0.0001), and fossa shape (P < 0.05).
Conclusions
The present analyses suggest that a steeper articular eminence inclination may be risk factor for TMD. The presence of TMD was associated with the condyle position in the TMJ.



Similar content being viewed by others
Change history
13 March 2018
In the original publication of the article in “Abstract”, the sentence that reads as “The present analyses suggest that a steeper articular eminence inclination may be risk factor” should read as “As a result of our analysis, we concluded that a low eminence angle may be risk factor”.
References
Okeson JP. Management of temporomandibular disorders and occlusion. St Louis: Elsevier Health Sciences; 2014.
Wang X, Zhang J, Gan Y, Zhou Y. Current understanding of pathogenesis and treatment of TMJ osteoarthritis. J Dent Res. 2015;94:666–73.
Laskin DM, Greene CS, Hylander WL. Temporomandibular disorders: an evidence-based approach to diagnosis and treatment. Hanover Park: Quintessence Publishing Company; 2006.
de Senna BR, Marques LS, França JP, Ramos-Jorge ML, Pereira LJ. Condyle-disk-fossa position and relationship to clinical signs and symptoms of temporomandibular disorders in women. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:e117–e24.
Lelis ÉR, Henriques JCG, Tavares M, de Mendonça MR, Neto AJF, de Araújo Almeida G. Cone-beam tomography assessment of the condylar position in asymptomatic and symptomatic young individuals. J Prosthet Dent. 2015;114:420–5.
Sümbüllü MA, Cağlayan F, Akgül HM, Yilmaz AB. Radiological examination of the articular eminence morphology using cone beam CT. Dentomaxillofac Radiol. 2014;41:234–40.
Zhang ZL, Cheng JG, Li G, Zhang JZ, Zhang ZY, Ma XC. Measurement accuracy of temporomandibular joint space in Promax 3-dimensional cone-beam computerized tomography images. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:112–7.
Paknahad M, Shahidi S. Association between mandibular condylar position and clinical dysfunction index. J Craniomaxillofac Surg. 2015;43:432–6.
Wu C-K, Hsu J-T, Shen Y-W, Chen J-H, Shen W-C, Fuh L-J. Assessments of inclinations of the mandibular fossa by computed tomography in an Asian population. Clin Oral Investig. 2012;16:443–50.
Brooks SL, Brand JW, Gibbs SJ, Hollender L, Lurie AG, Omnell K-Å, et al. Imaging of the temporomandibular joint: a position paper of the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:609–18.
Farman AG, Ludlow JB, Davies KL, Tyndall DA. Temporomandibular joint imaging: a comparative study of diagnostic accuracy for the detection of bone change with biplanar multidirectional tomography and panoramic images. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:735–43.
Larheim T, Abrahamsson A, Kristensen M, Arvidsson L. Temporomandibular joint diagnostics using CBCT. Dentomaxillofac Radiol. 2015;44:20140235.
Hintze H, Wiese M, Wenzel A. Cone beam CT and conventional tomography for the detection of morphological temporomandibular joint changes. Dentomaxillofac Radiol. 2007;36:192–7.
Lascala C, Panella J, Marques M. Analysis of the accuracy of linear measurements obtained by cone beam computed tomography (CBCT-NewTom). Dentomaxillofac Radiol. 2004;33:291–4.
Sinha VP, Pradhan H, Gupta H, Mohammad S, Singh R, Mehrotra D, et al. Efficacy of plain radiographs, CT scan, MRI and ultrasonography in temporomandibular joint disorders. Natl. J Maxillofac Surg. 2012;3:2–9.
Hintze H, Wiese M, Wenzel A. Comparison of three radiographic methods for detection of morphological temporomandibular joint changes: panoramic, scanographic and tomographic examination. Dentomaxillofac Radiol. 2009;38:134–40.
Celikoglu M, Ucar FI, Buyuk SK, Celik S, Sekerci AE, Akin M. Evaluation of the mandibular volume and correlating variables in patients affected by unilateral and bilateral cleft lip and palate: a cone-beam computed tomography study. Clin Oral Investig. 2016;20:1741–6.
Kobayashi K, Shimoda S, Nakagawa Y, Yamamoto A. Accuracy in measurement of distance using limited cone-beam computerized tomography. Int J Oral Maxillofac Implants. 2003;19:228–31.
Katsavrias EG. Changes in articular eminence inclination during the craniofacial growth period. Angle Orthod. 2002;72:258–64.
Keller D, Carano A. Eminence-posterior occlusal plane angle in patients with temporomandibular disorders. Cranio. 1991;9:159–64.
Sülün T, Cemgil T, Duc J-MP, Rammelsberg P, Jäger L, Gernet W. Morphology of the mandibular fossa and inclination of the articular eminence in patients with internal derangement and in symptom-free volunteers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:98–107.
Ozkan A, Altug HA, Sencimen M, Senel B. Evaluation of articular eminence morphology and inclination in TMJ internal derangement patients with MRI. Int. J Morphol. 2012;30:740–4.
Ren Y-F, Isberg A, Westesson P-L. Steepness of the articular eminence in the temporomandibular joint: tomographic comparison between asymptomatic volunteers with normal disk position and patients with disk displacement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:258–66.
İlgüy D, İlgüy M, Fişekçioğlu E, Dölekoğlu S, Ersan N. Articular eminence inclination, height, and condyle morphology on cone beam computed tomography. ScientificWorldJournal. 2014;2014:761714.
Galante G, Paesani D, Tallents R, Hatala M, Katzberg R, Murphy W. Angle of the articular eminence in patients with temporomandibular joint dysfunction and asymptomatic volunteers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:242–9.
Savastano C, Craca R. Inclination of the temporomandibular eminence and craniomandibular disorders. Minerva Stomatol. 1991;40:769–74.
Živko-Babić J, Pandurić J, Jerolimov V, Mioč M, Pižeta I, Jakovac M. Bite force in subjects with complete dentition. Coll Antropol. 2002;26:293–302.
Jasinevicius T, Pyle M, Nelson S, Lalumandier J, Kohrs K, Sawyer D. Relationship of degenerative changes of the temporomandibular joint (TMJ) with the angle of eminentia. J Oral Rehabil. 2006;33:638–45.
Çağlayan F, Sümbüllü MA, Akgül HM. Associations between the articular eminence inclination and condylar bone changes, condylar movements, and condyle and fossa shapes. Oral Radiol. 2014;30:84–91.
Major PW, Kinniburgh RD, Nebbe B, Prasad NG, Glover KE. Tomographic assessment of temporomandibular joint osseous articular surface contour and spatial relationships associated with disc displacement and disc length. Am J Orthod Dentofacial Orthop. 2002;121:152–61.
Katzberg RW, Keith DA, Ten Eick WR, Guralnick WC. Internal derangements of the temporomandibular joint: an assessment of condylar position in centric occlusion. J Prosthet Dent. 1983;49:250–4.
Solberg W, Hansson T, Nordström B. The temporomandibular joint in young adults at autopsy: a morphologic classification and evaluation. Oral Rehabil. 1985;12:303–21.
Al-koshab M, Nambiar P, John J. Assessment of condyle and glenoid fossa morphology using CBCT in South-East Asians. PLoS One. 2015;10:e0121682.
Okur A, Ozkiris M, Kapusuz Z, Karaçavus S, Saydam L. Characteristics of articular fossa and condyle in patients with temporomandibular joint complaint. Eur Rev Med Pharmacol Sci. 2012;16:2131–5.
Kinniburgh RD, Major PW, Nebbe B, West K, Glover KE. Osseous morphology and spatial relationships of the temporomandibular joint: comparisons of normal and anterior disc positions. Angle Orthod. 2000;70:70–80.
Ikeda K, Kawamura A. Assessment of optimal condylar position with limited cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2009;135:495–501.
Yale SH, Allison BD, Hauptfuehrer J. An epidemiological assessment of mandibular condyle morphology. Oral Surg Oral Med Oral Pathol. 1966;21:169–77.
Matsumoto K, Kameoka S, Amemiya T, Yamada H, Araki M, Iwai K, et al. Discrepancy of coronal morphology between mandibular condyle and fossa is related to pathogenesis of anterior disk displacement of the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:626–32.
de Farias JF, Melo SL, Bento PM, Oliveira LS, Campos PS, de Melo DP. Correlation between temporomandibular joint morphology and disc displacement by MRI. Dentomaxillofac Radiol. 2015;44:20150023.
Katsavrias EG. Morphology of the temporomandibular joint in subjects with Class II Division 2 malocclusions. Am J Orthod Dentofacial Orthop. 2006;129:470–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Compliance with Ethical Standards
Conflict of interest
Yasin Yasa and Hayati Murat Akgül declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Research involving human participants and/or animals
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions.
Additional information
A correction to this article is available online at https://doi.org/10.1007/s11282-018-0323-2.
Rights and permissions
About this article
Cite this article
Yasa, Y., Akgül, H.M. Comparative cone-beam computed tomography evaluation of the osseous morphology of the temporomandibular joint in temporomandibular dysfunction patients and asymptomatic individuals. Oral Radiol 34, 31–39 (2018). https://doi.org/10.1007/s11282-017-0279-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11282-017-0279-7