Abstract
Purpose
To evaluate patient outcomes in a contemporary cohort of patients undergoing partial nephrectomy (PN) or radical nephrectomy (RN).
Methods
The NSQIP database was used to identify patients undergoing PN or RN for renal neoplasms between 2010 and 2018. The SEER database was also queried to assess changes in tumor staging during the study period. Logistic regression was used to assess the independent relationship between surgery year and approach on postoperative complications.
Results
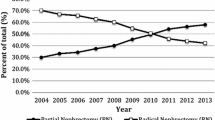
Between 2010 and 2018, NSQIP captured 58,020 cases, including 26,745 (46%) PN and 31,275 (54%) RN. The proportion of PN increased annually, from 39.8% in 2010 to 48.7% in 2018. This rise in PN coincided with a decrease in the proportion of patients experiencing complications, irrespective of surgical approach (20.4% of total cases to 14.2% of total cases). While limited by a lack of information on tumor characteristics, multivariable analysis controlling for patient characteristics demonstrated that RN was associated with an increased risk of complications, OR 1.42 (95% CI 1.35–1.49).
Conclusion
Here, we report an 8.9% increase in the proportion of patients undergoing PN between 2010 and 2018, with no associated increase in perioperative morbidity/mortality. Given that there was no concurrent shift in stage or size of kidney tumors undergoing resection during the study period, these data therefore suggest markedly improved surgical technique and perioperative management nationally. Furthermore, the relative burden of complications has shifted from patients undergoing PN to those undergoing RN. Therefore PN, when technically feasible, should be increasingly considered.



Similar content being viewed by others
Abbreviations
- ACS:
-
American College of Surgeons
- ARF:
-
Acute Renal Failure
- ASA:
-
American Society of Anesthesiologists
- AUA:
-
American Urological Association
- BMI:
-
Body Mass Index
- CCI:
-
Charlson Comorbidity Index
- CHF:
-
Congestive Heart Failure
- CKD:
-
Chronic Kidney Disease
- COPD:
-
Chronic obstructive pulmonary disease
- CPT:
-
Current Procedural Terminology
- DM:
-
Diabetes Mellitus
- HTN:
-
Hypertension
- MI:
-
Myocardial Infarction
- NSQIP:
-
National Surgical Quality Improvement Program (NSQIP)
- PE:
-
Pulmonary embolism
- PN:
-
Partial Nephrectomy
- PNA:
-
Pneumonia
- RN:
-
Radical Nephrectomy
- SEER:
-
Surveillance, Epidemiology and End Results
- SRM:
-
Small Renal Mass
- UTI:
-
Urinary Tract infection
References
American Cancer Society. Cancer Statistics Center. http://cancerstatisticscenter.cancer.org; 2020 Accessed 10 September 2020.
Akdogan B, Gudeloglu A, Inci K et al (2012) Prevalence and predictors of benign lesions in renal masses smaller than 7 cm presumed to be renal cell carcinoma. ClinGenitourin Cancer 10(2):121–125. https://doi.org/10.1016/j.clgc.2012.01.005
Campbell S, Uzzo RG, Allaf ME et al (2017) Renal mass and localized renal cancer: AUA guideline. J Urol 198:520–529
Gill IS, Aron M, Gervais DA, Jewett MA (2010) Clinical practice. Small renal mass. N Engl J Med 362:624e34. https://doi.org/10.1056/NEJMcp0910041
Volpe A, Cadeddu JA, Cestari A et al (2011) Contemporary management of small renal masses. EurUrol 60:501–515. https://doi.org/10.1016/j.eururo.2011.05.044
Touijer K, Jacqmin D, Kavoussi LR et al (2010) The expanding role of partial nephrectomy: a critical analysis of indications, results, and complications. EurUrol 57(2):214–222. https://doi.org/10.1016/j.eururo.2009.10.019
Leibovich BC, Blute ML, Cheville JC et al (2004) Nephron sparing surgery for appropriately selected renal cell carcinoma between 4 and 7 cm results in outcome similar to radical nephrectomy. J Urol 171(3):1066–1070. https://doi.org/10.1097/01.ju.0000113274.40885.db
Dash A, Vickers AJ, Schachter LR et al (2006) Comparison of outcomes in elective partial vs radical nephrectomy for clear cell renal cell carcinoma of 4–7 cm. BJU Int 97(5):939–945. https://doi.org/10.1111/j.1464-410X.2006.06060.x
Semerjian A, Zettervall SL, Amdur R et al (2015) 30 Day morbidity and mortality outcomes of prolonged minimally invasive kidney procedures compared with shorter open procedures: national surgical quality improvement program analysis. J Endourol 29:830–837. https://doi.org/10.1089/end.2014.0795
Liu JJ, Leppert JT, Maxwell BG et al (2014) Trends and perioperative outcomes for laparoscopic and robotic nephrectomy using the national surgical quality improvement program (NSQIP) database. Urologic Oncology 32(34):473–479. https://doi.org/10.1016/j.urolonc.2013.09.012
Hutter MM, Roswell KS, Devaney LA et al (2006) Identification of surgical complications and deaths: an assessment of the traditional surgical morbidity and mortality conference compared with the American college of surgeons-national surgical quality improvement program. J Am CollSurg 203:618–624. https://doi.org/10.1016/j.jamcollsurg.2006.07.010
Shiloach M, Frencher SK, Steeger JE et al (2010) Toward robust information: data quality and inter-rater reliability in the American college of surgeons national surgical quality improvement program. J Am CollSurg 210:6–16. https://doi.org/10.1016/j.jamcollsurg.2009.09.031
Fuchshuber PR, Greif W, Tidwell CR et al (2012) The power of the national surgical quality improvement program–achieving a zero-pneumonia rate in general surgery patients. Perm J 16(1):39–45. https://doi.org/10.7812/tpp/11-127
Yu H, Hevelone ND, Lipsitz SR et al (2012) Use, costs and comparative effectiveness of robotic assisted, laparoscopic and open urological surgery. J Urol 187:1392–1398. https://doi.org/10.1016/j.juro.2011.11.089
Thompson RH, Kaag M, Vickers A et al (2009) Contemporary use of partial nephrectomy at a tertiary care center in the United States. J Urol 181:993–997. https://doi.org/10.1016/j.juro.2008.11.017
Van Poppel H, Da Pozzo L, Albrecht W et al (2007) A prospective randomized EORTC intergroup hase 3 study comparing the complications of elective nephron-sparing surgery and radical nephrectomy for low-stage renal cell carcinoma. EurUrol 51:1606–1615. https://doi.org/10.1016/j.eururo.2010.12.013
Laycock WS, Siewers AE, Birkmeyer CM et al (2000) Variation in the use of laparoscopic cholecystectomy for elderly patients with acute cholecystitis. Arch Surg 135(4):457–462. https://doi.org/10.1001/archsurg.135.4.457
Lane BR, Campbell SC, Gill IS (2013) 10 Year oncologic outcomes after laparoscopic and open partial nephrectomy. J Urol 190(1):44–49. https://doi.org/10.1016/j.juro.2012.12.102
Lane BR, Fergany AF, Weight CJ, Campbell SC (2010) Renal functional outcomes after partial nephrectomy with extended ischemic intervals are better than after radical nephrectomy. J Urol 184(4):1286–1290. https://doi.org/10.1016/j.juro.2010.06.011
Funding
None of the authors has a financial interest in any of the products, devices, or drugs mentioned in this manuscript. There are no funding sources to disclose.
Author information
Authors and Affiliations
Contributions
KG: protocol/project development, data collection, data analysis, manuscript writing/editing. DO-L: protocol/project development, data collection, data analysis, manuscript writing/editing. DS: Manuscript editing. JS: Protocol/project development, manuscript editing. KG and DO-L authors share first authorship with equal contribution to the current study.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no significant conflicts of interest with any companies or organization whose products or services may be discussed in this article.
Research involving human participants and/or animals
Neither human nor animal participants were recruited for this study. The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) is a nationally validated, risk-adjusted, outcomes-based database used to measure and improve the quality of surgical care. Data are retrospective de-identified variables regarding surgical procedures and outcomes. Therefore, the University Hospitals Cleveland Medical Center (UH CMC) Institutional Review Board granted an exemption for this study. The IRB exemption protocol was approved on August 26, 2020.
Informed Consent
Informed consent was not required for this study given the utilization of retrospective de-identified variables. The University Hospitals Cleveland Medical Center (UH CMC) Institutional Review Board granted an exemption for this study on August 26, 2020.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gupta, K., Omil-Lima, D., Sheyn, D. et al. Temporal improvements in renal surgery outcomes across surgical approaches. Int Urol Nephrol 53, 1311–1316 (2021). https://doi.org/10.1007/s11255-021-02811-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-021-02811-z