Abstract
Purpose
Lymphocele (LC) is the most common adverse sequela of pelvic lymphadenectomy (PLND) during radical prostatectomy for prostate cancer. Current evidence on comparison between robotic (RARP) and open retropubic prostatectomy (RRP) in terms of the development of symptomatic LCs (SLCs) is conflicting. Moreover, no single-center assessment has illuminated the impact of the anterior vs. posterior approach of RARP on the rate of SLCs yet. We aimed to compare RRP and transperitoneal RARP for the SLC development and associated clinical risk factors.
Methods
Patients treated with RRP or transperitoneal RARP (both with standard PLND) were included. Univariate comparisons and multivariate logistic regression analysis were utilized to compare the cohorts and define independent predictive variables for the development of SLCs.
Results
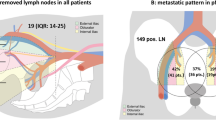
Five hundred and ninety-five consecutive PCa patients underwent RRP and 277 ones RARP (76 anterior and 201 posterior approaches). The incidence of SLCs did not differ between both cohorts. Age and lymph node yield were independent predictors for the development of SLCs after RRP. There was a trend for a longer median time to development of SLCs after RARP as compared to RRP. Median duration of percutaneous drainage tended to be higher after RRP then after RARP. Failure rate of lymphocele drainage was comparable between both techniques.
Conclusions
RRP and RARP are associated with the same risk for the development of a SLC. Posterior approach does not reduce the SLC formation compared to the anterior technique. Patients’ age and LN yield are predictive for the SLC occurrence in patients treated with RRP.
Similar content being viewed by others

References
Anheuser P, Treiyer A, Stark E, Haben B, Steffens JA (2010) Lymphoceles after radical retropubic prostatectomy. A treatment algorithm. Urol A 49(7):832–836. https://doi.org/10.1007/s00120-010-2318-4
Ploussard G, Briganti A, de la Taille A, Haese A, Heidenreich A, Menon M, Sulser T, Tewari AK, Eastham JA (2014) Pelvic lymph node dissection during robot-assisted radical prostatectomy: efficacy, limitations, and complications-a systematic review of the literature. Eur Urol 65(1):7–16. https://doi.org/10.1016/j.eururo.2013.03.057
Solberg A, Angelsen A, Bergan U, Haugen OA, Viset T, Klepp O (2003) Frequency of lymphoceles after open and laparoscopic pelvic lymph node dissection in patients with prostate cancer. Scand J Urol Nephrol 37(3):218–221
Zorn KC, Katz MH, Bernstein A, Shikanov SA, Brendler CB, Zagaja GP, Shalhav AL (2009) Pelvic lymphadenectomy during robot-assisted radical prostatectomy: assessing nodal yield, perioperative outcomes, and complications. Urology 74(2):296–302. https://doi.org/10.1016/j.urology.2009.01.077
Capitanio U, Pellucchi F, Gallina A, Briganti A, Suardi N, Salonia A, Abdollah F, Di Trapani E, Jeldres C, Cestari A, Karakiewicz PI, Montorsi F (2011) How can we predict lymphorrhoea and clinically significant lymphocoeles after radical prostatectomy and pelvic lymphadenectomy? Clinical implications. BJU Int 107(7):1095–1101. https://doi.org/10.1111/j.1464-410X.2010.09580.x
Liss MA, Skarecky D, Morales B, Osann K, Eichel L, Ahlering TE (2013) Preventing perioperative complications of robotic-assisted radical prostatectomy. Urology 81(2):319–323. https://doi.org/10.1016/j.urology.2012.09.033
Naselli A, Andreatta R, Introini C, Fontana V, Puppo P (2010) Predictors of symptomatic lymphocele after lymph node excision and radical prostatectomy. Urology 75(3):630–635. https://doi.org/10.1016/j.urology.2009.03.011
Orvieto MA, Coelho RF, Chauhan S, Palmer KJ, Rocco B, Patel VR (2011) Incidence of lymphoceles after robot-assisted pelvic lymph node dissection. BJU Int 108(7):1185–1190. https://doi.org/10.1111/j.1464-410X.2011.10094.x
Khoder WY, Trottmann M, Buchner A, Stuber A, Hoffmann S, Stief CG, Becker AJ (2011) Risk factors for pelvic lymphoceles post-radical prostatectomy. Int J Urol 18(9):638–643. https://doi.org/10.1111/j.1442-2042.2011.02797.x
Lee HJ, Kane CJ (2014) How to minimize lymphoceles and treat clinically symptomatic lymphoceles after radical prostatectomy. Curr Urol Rep 15(10):445. https://doi.org/10.1007/s11934-014-0445-y
Crawford ED, Batuello JT, Snow P, Gamito EJ, McLeod DG, Partin AW, Stone N, Montie J, Stock R, Lynch J, Brandt J (2000) The use of artificial intelligence technology to predict lymph node spread in men with clinically localized prostate carcinoma. Cancer 88(9):2105–2109
Mottet N, Bellmunt J, Bolla M, Briers E, Cumberbatch MG, De Santis M, Fossati N, Gross T, Henry AM, Joniau S, Lam TB, Mason MD, Matveev VB, Moldovan PC, van den Bergh RCN, Van den Broeck T, van der Poel HG, van der Kwast TH, Rouviere O, Schoots IG, Wiegel T, Cornford P (2017) EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol 71(4):618–629. https://doi.org/10.1016/j.eururo.2016.08.003
Yuh B, Artibani W, Heidenreich A, Kimm S, Menon M, Novara G, Tewari A, Touijer K, Wilson T, Zorn KC, Eggener SE (2014) The role of robot-assisted radical prostatectomy and pelvic lymph node dissection in the management of high-risk prostate cancer: a systematic review. Eur Urol 65(5):918–927. https://doi.org/10.1016/j.eururo.2013.05.026
Chang SL, Kibel AS, Brooks JD, Chung BI (2015) The impact of robotic surgery on the surgical management of prostate cancer in the USA. BJU Int 115(6):929–936. https://doi.org/10.1111/bju.12850
Akand M, Erdogru T, Avci E, Ates M (2015) Transperitoneal versus extraperitoneal robot-assisted laparoscopic radical prostatectomy: a prospective single surgeon randomized comparative study. Int J Urol 22(10):916–921. https://doi.org/10.1111/iju.12854
Semerjian A, Pavlovich CP (2017) Extraperitoneal robot-assisted radical prostatectomy: indications, technique and outcomes. Curr Urol Rep 18(6):42. https://doi.org/10.1007/s11934-017-0689-4
Thomas C, van de Plas J, Tsaur I, Neisius A, Bartsch G, Frees S, Borgmann H, Jäger W, Brandt MP, Haferkamp A, Rubenwolf P (2017) Incidence, risk factors and management of symptomatic lymphoceles after radical retropubic prostatectomy. Urol Pract 4(6):493–498. https://doi.org/10.1016/j.urpr.2016.11.003
Gillitzer R, Thuroff JW, Neisius A, Wollner J, Hampel C (2009) Robot-assisted ascending-descending laparoscopic nerve-sparing prostatectomy. BJU Int 104(1):128–153. https://doi.org/10.1111/j.1464-410X.2009.08723.x
Hamada A, Hwang C, Fleisher J, Tuerk I (2017) Microbiological evaluation of infected pelvic lymphocele after robotic prostatectomy: potential predictors for culture positivity and selection of the best empirical antimicrobial therapy. Int Urol Nephrol 49(7):1183–1191. https://doi.org/10.1007/s11255-017-1599-6
Froehner M, Novotny V, Koch R, Leike S, Twelker L, Wirth MP (2013) Perioperative complications after radical prostatectomy: open versus robot-assisted laparoscopic approach. Urol Int 90(3):312–315. https://doi.org/10.1159/000345323
Grande P, Di Pierro GB, Mordasini L, Ferrari M, Wurnschimmel C, Danuser H, Mattei A (2017) Prospective randomized trial comparing titanium clips to bipolar coagulation in sealing lymphatic vessels during pelvic lymph node dissection at the time of robot-assisted radical prostatectomy. Eur Urol 71(2):155–158. https://doi.org/10.1016/j.eururo.2016.08.006
Stolzenburg JU, Kyriazis I, Liatsikos E (2017) Postoperative lymphocele formation after pelvic lymph node dissection at the time of radical prostatectomy should not be considered an inevitable consequence of the approach. Eur Urol 71(2):159–160. https://doi.org/10.1016/j.eururo.2016.08.046
Davis JW, Shah JB, Achim M (2011) Robot-assisted extended pelvic lymph node dissection (PLND) at the time of radical prostatectomy (RP): a video-based illustration of technique, results, and unmet patient selection needs. BJU Int 108(6 Pt 2):993–998. https://doi.org/10.1111/j.1464-410X.2011.10454.x
Palapattu GS, Allaf ME, Trock BJ, Epstein JI, Walsh PC (2004) Prostate specific antigen progression in men with lymph node metastases following radical prostatectomy: results of long-term followup. J Urol 172(5 Pt 1):1860–1864
Daneshmand S, Quek ML, Stein JP, Lieskovsky G, Cai J, Pinski J, Skinner EC, Skinner DG (2004) Prognosis of patients with lymph node positive prostate cancer following radical prostatectomy: long-term results. J Urol 172(6 Pt 1):2252–2255
Cooperberg MR, Kane CJ, Cowan JE, Carroll PR (2010) Adequacy of lymphadenectomy among men undergoing robot-assisted laparoscopic radical prostatectomy. BJU Int 105(1):88–92. https://doi.org/10.1111/j.1464-410X.2009.08699.x
Polcari AJ, Hugen CM, Sivarajan G, Woods ME, Paner GP, Flanigan RC, Quek ML (2009) Comparison of open and robot-assisted pelvic lymphadenectomy for prostate cancer. J Endourol 23(8):1313–1317. https://doi.org/10.1089/end.2009.0109
Truesdale MD, Lee DJ, Cheetham PJ, Hruby GW, Turk AT, Badani KK (2010) Assessment of lymph node yield after pelvic lymph node dissection in men with prostate cancer: a comparison between robot-assisted radical prostatectomy and open radical prostatectomy in the modern era. J Endourol 24(7):1055–1060. https://doi.org/10.1089/end.2010.0128
Gandaglia G, Trinh QD, Hu JC, Schiffmann J, Becker A, Roghmann F, Popa I, Tian Z, Perrotte P, Montorsi F, Briganti A, Karakiewicz PI, Sun M, Abdollah F (2014) The impact of robot-assisted radical prostatectomy on the use and extent of pelvic lymph node dissection in the “post-dissemination” period. Eur J Surg Oncol 40(9):1080–1086. https://doi.org/10.1016/j.ejso.2013.12.016
Suardi N, Larcher A, Haese A, Ficarra V, Govorov A, Buffi NM, Walz J, Rocco B, Borghesi M, Steuber T, Pini G, Briganti A, Mottrie AM, Guazzoni G, Montorsi F, Pushkar D, Van Der Poel H (2014) Indication for and extension of pelvic lymph node dissection during robot-assisted radical prostatectomy: an analysis of five European institutions. Eur Urol 66(4):635–643. https://doi.org/10.1016/j.eururo.2013.12.059
Keskin MS, Argun OB, Obek C, Tufek I, Tuna MB, Mourmouris P, Erdogan S, Kural AR (2016) The incidence and sequela of lymphocele formation after robot-assisted extended pelvic lymph node dissection. BJU Int 118(1):127–131. https://doi.org/10.1111/bju.13425
Weingartner K, Ramaswamy A, Bittinger A, Gerharz EW, Voge D, Riedmiller H (1996) Anatomical basis for pelvic lymphadenectomy in prostate cancer: results of an autopsy study and implications for the clinic. J Urol 156(6):1969–1971
Bochner BH, Cho D, Herr HW, Donat M, Kattan MW, Dalbagni G (2004) Prospectively packaged lymph node dissections with radical cystectomy: evaluation of node count variability and node mapping. J Urol 172(4 Pt 1):1286–1290
Acknowledgements
We thank Jeroen van de Plas for data acquisition. This study is part of the doctoral thesis of Stefanie Ziewers.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Thomas, C., Ziewers, S., Thomas, A. et al. Development of symptomatic lymphoceles after radical prostatectomy and pelvic lymph node dissection is independent of surgical approach: a single-center analysis. Int Urol Nephrol 51, 633–640 (2019). https://doi.org/10.1007/s11255-019-02103-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-019-02103-7