Abstract
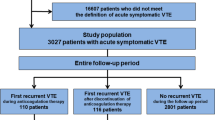
Limited evidence exists regarding management of recurrent venous thromboembolism (VTE) that occurs during anticoagulant therapy. We aimed to describe patient characteristics, drug therapy management, and outcomes of patients with VTE recurrence during anticoagulant therapy. We identified 30 relevant episodes of VTE recurrence. Mean age was 48.9 (15.9) years, 56.7% were male, and 93.3% were White. Common VTE risk factors included cancer (46.6%), recent surgery (33.3%), and prolonged immobility (30.0%). At the time of recurrent VTE, 40.0% were receiving enoxaparin, 30.0% warfarin, and 23.3% direct oral anticoagulants. Potential causes for VTE recurrence included indwelling venous catheters (40.0%), cancer (33.3%), subtherapeutic anticoagulation (26.7%), and nonadherence (23.3%). Recurrent VTE management strategies included switching anticoagulants (26.7%), increasing anticoagulant dose (20.0%), temporarily adding enoxaparin or unfractionated heparin to oral anticoagulation therapy (13.3%), or no change in anticoagulation therapy (43.3%). Only four adverse 90-day outcomes occurred among 17 patients who received anticoagulant therapy changes in response to VTE recurrence, whereas eight adverse outcomes occurred in the 13 patients who received no change in anticoagulation therapy in response to a recurrent VTE episode (P value 0.04). Regardless of the potential etiology of recurrent VTE during anticoagulant therapy; switching anticoagulants, temporarily adding injectable anticoagulants, or increasing anticoagulant intensity appears preferable to continuing current anticoagulant therapy unchanged.
Similar content being viewed by others
References
Heit JA, Spencer FA, White RH (2016) The epidemiology of venous thromboembolism. J Thromb Thrombolysis 41(1):3–14
Kearon C, Akl EA, Ornelas J et al (2016) Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest 149(2):315–352
Prandoni P, Lensing AW, Piccioli A et al (2002) Recurrent venous thromboembolism and bleeding complications during anticoagulant treatment in patients with cancer and venous thrombosis. Blood 100(10):3484–3488
Carrier M, Le Gal G, Cho R, Tierney S, Rodger M, Lee AY (2009) Dose escalation of low molecular weight heparin to manage recurrent venous thromboembolic events despite systemic anticoagulation in cancer patients. J Thromb Haemost 7(5):760–765
Casciano JP, Dotiwala Z, Kemp R, Li C, Cai J, Preblick R (2015) Economic burden of recurrent venous thromboembolism: analysis from a U.S. hospital perspective. Am J Health Syst Pharm 72(4):291–300
Schulman S (2017) How I treat recurrent venous thromboembolism in patients receiving anticoagulant therapy. Blood 129(25):3285–3293
Rodger MA, Miranda S, Delluc A, Carrier M (2019) Management of suspected and confirmed recurrent venous thrombosis while on anticoagulant therapy. What next? Thromb Res 180:105–109
Schulman S, Zondag M, Linkins L et al (2015) Recurrent venous thromboembolism in anticoagulated patients with cancer: management and short-term prognosis. J Thromb Haemost 13(6):1010–1018
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381
Harris PA, Taylor R, Minor BL et al (2019) The REDCap consortium: building an international community of software platform partners. J Biomed Inform 95:103208
Schulman S, Kearon C, Subcommittee on Control of Anticoagulation of the Scientific Standardization Committee of the International Society on Thrombosis and Haemostasis (2005) Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost 3(4):692–694
Kaatz S, Ahmad D, Spyropoulos AC, Schulman S, Subcommittee on Control of Anticoagulation Therapy (2015) Definition of clinically relevant non-major bleeding in studies of anticoagulants in atrial fibrillation and venous thromboembolic disease in non-surgical patients: communication from the SSC of the ISTH. J Thromb Haemost 13(11):2119–2126
Wall C, Moore J, Thachil J (2016) Catheter-related thrombosis: a practical approach. J Intensive Care Soc 17(2):160–167
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lai, N., Jones, A.E., Johnson, S.A. et al. Anticoagulant therapy management of venous thromboembolism recurrence occurring during anticoagulant therapy: a descriptive study. J Thromb Thrombolysis 52, 414–418 (2021). https://doi.org/10.1007/s11239-021-02377-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-021-02377-8