Abstract
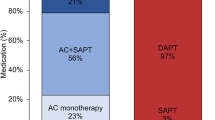
The relation of device related thrombosis (DRT) and major bleeding after left atrial appendage closure (LAAC) to laboratory thrombosis and hemostasis markers has not been studied. We performed a prospective case control study to identify clinical characteristics and laboratory markers in patients who developed DRT and major bleeding following WATCHMAN LAAC. Thromboelastography, platelet aggregation (PA), urinary 11-dehydrothromboxane B2 (UTX), fibrinogen, d-dimer, thrombin time and von Willebrand factor activity were determined at baseline, immediately following, and at 45 and 180 days post-LAAC (n = 32) and outcomes were followed for 1 year. Baseline characteristics and thrombogenic profiles of patients with and without DRT and/or BARC bleeding were compared. Mean age was 76 ± 8 years and CHADS2 VASc score was 4.4 ± 1.4. There were 3 DRTs (2 within 6 months, and 1 at 12 months), 4 Type 3A BARC bleeds, and 2 non-cardiac deaths. Patients with DRT had higher baseline thrombin-induced platelet–fibrin clot strength (68.0 ± 1.8 vs. 62.7 ± 4.7 mm, p = 0.06); FCS (35.6 ± 6.0 vs. 24.4 ± 6.6 mm, p = 0.009); and d-dimer (1712 ± 2330 vs. 283 ± 213 ng/mL, p = 0.001). At baseline, 5 patients had all 3 factors associated with high thrombotic risk and 2 experienced a DRT within 6 months. Patients with Type 3A BARC bleeding had lower baseline collagen-induced and 45-day ADP-induced PA (p < 0.01 for both). DRT following LAAC was associated with a baseline prothrombogenic profile whereas bleeding was associated with low platelet reactivity. These preliminary findings warrant further validation and have future implications on patient selection and adjunctive antithrombotic therapy following LAAC.
Clinical Trial Registration: https://clinicaltrials.gov/ct2/show/NCT03040622.





Similar content being viewed by others
Abbreviations
- ADP:
-
Adenosine diphosphate
- AF:
-
Atrial fibrillation
- BARC:
-
Major bleeding using the Academic Research Consortium
- DRT:
-
Device related thrombosis
- FCS:
-
Fibrin clot strength
- HPR:
-
High platelet reactivity
- INR:
-
International normalized ratio
- LAAC:
-
Left atrial appendage closure
- NOAC:
-
Novel oral anticoagulant
- PA:
-
Platelet aggregation
- TEE:
-
Transesophageal echocardiography
- TEG:
-
Thrombelastography
- TT:
-
Thrombin time
- TIP-FCS:
-
Thrombin induced platelet–fibrin clot strength
- TRAP:
-
Thrombin receptor-activating peptide
- UTX:
-
Urinary 11-dehydrothromboxane B2
- ULN:
-
Upper limits normal
- vWF:
-
Von Willebrand factor
References
Reddy VY, Doshi SK, Kar S, Gibson DN, Price MJ, Huber K, Horton RP, Buchbinder M, Neuzil P, Gordon NT, Holmes DR Jr, Prevail IPA (2017) 5-Year outcomes after left atrial appendage closure: from the PREVAIL and PROTECT AF trials. J Am Coll Cardiol 70(24):2964–2975. https://doi.org/10.1016/j.jacc.2017.10.021
Holmes DR Jr, Kar S, Price MJ, Whisenant B, Sievert H, Doshi SK, Huber K, Reddy VY (2014) Prospective randomized evaluation of the Watchman left atrial appendage closure device in patients with atrial fibrillation versus long-term warfarin therapy: the PREVAIL trial. J Am Coll Cardiol 64(1):1–12. https://doi.org/10.1016/j.jacc.2014.04.029
Belgaid DR, Khan Z, Zaidi M, Hobbs A (2016) Prospective randomized evaluation of the Watchman left atrial appendage closure device in patients with atrial fibrillation versus long-term warfarin therapy: the PREVAIL trial. Int J Cardiol 219:177–179. https://doi.org/10.1016/j.ijcard.2016.06.041
Reddy VY, Doshi SK, Sievert H, Buchbinder M, Neuzil P, Huber K, Halperin JL, Holmes D, Investigators PA (2013) Percutaneous left atrial appendage closure for stroke prophylaxis in patients with atrial fibrillation: 2.3-year follow-up of the PROTECT AF (Watchman left atrial appendage system for embolic protection in patients with atrial fibrillation) trial. Circulation 127(6):720–729. https://doi.org/10.1161/CIRCULATIONAHA.112.114389
Boersma LV, Ince H, Kische S, Pokushalov E, Schmitz T, Schmidt B, Gori T, Meincke F, Protopopov AV, Betts T, Mazzone P, Foley D, Grygier M, Sievert H, De Potter T, Vireca E, Stein K, Bergmann MW, following i, institutions participated in the Es (2019) Evaluating real-world clinical outcomes in atrial fibrillation patients receiving the WATCHMAN left atrial appendage closure technology. Circ Arrhythm Electrophysiol 12(4):e006841. https://doi.org/10.1161/CIRCEP.118.006841
Reddy VY, Mobius-Winkler S, Miller MA, Neuzil P, Schuler G, Wiebe J, Sick P, Sievert H (2013) Left atrial appendage closure with the Watchman device in patients with a contraindication for oral anticoagulation: the ASAP study (ASA plavix feasibility study with Watchman left atrial appendage closure technology). J Am Coll Cardiol 61(25):2551–2556. https://doi.org/10.1016/j.jacc.2013.03.035
Price MJ, Reddy VY, Valderrabano M, Halperin JL, Gibson DN, Gordon N, Huber KC, Holmes DR Jr (2015) Bleeding outcomes after left atrial appendage closure compared with long-term warfarin: a pooled, patient-level analysis of the WATCHMAN randomized trial experience. JACC Cardiovasc Interv 8(15):1925–1932. https://doi.org/10.1016/j.jcin.2015.08.035
Holmes DR Jr, Doshi SK, Kar S, Price MJ, Sanchez JM, Sievert H, Valderrabano M, Reddy VY (2015) Left atrial appendage closure as an alternative to warfarin for stroke prevention in atrial fibrillation: a patient-level meta-analysis. J Am Coll Cardiol 65(24):2614–2623. https://doi.org/10.1016/j.jacc.2015.04.025
Holmes DR, Reddy VY, Buchbinder M, Stein K, Elletson M, Bergmann MW, Schmidt B, Saw J (2017) The assessment of the Watchman device in patients unsuitable for oral anticoagulation (ASAP-TOO) trial. Am Heart J 189:68–74. https://doi.org/10.1016/j.ahj.2017.03.007
Romero J, Briceno DF, Di Biase L (2019) NOACs versus VKAs during Watchman implantation in patients with atrial fibrillation: the end of an era. Pacing Clin Electrophysiol 42(10):1310–1311. https://doi.org/10.1111/pace.13797
Gurbel PA, Bliden KP, Tantry US, Monroe AL, Muresan AA, Brunner NE, Lopez-Espina CG, Delmenico PR, Cohen E, Raviv G, Haugen DL, Ereth MH (2016) First report of the point-of-care TEG: a technical validation study of the TEG-6S system. Platelets 27(7):642–649. https://doi.org/10.3109/09537104.2016.1153617
Gurbel PA, Bliden KP, Hiatt BL, O'Connor CM (2003) Clopidogrel for coronary stenting: response variability, drug resistance, and the effect of pretreatment platelet reactivity. Circulation 107(23):2908–2913. https://doi.org/10.1161/01.CIR.0000072771.11429.83
Bliden KP, Singla A, Gesheff MG, Toth PP, Tabrizchi A, Ens G, Guyer K, Singh M, Franzese CJ, Stapleton D, Tantry US, Gurbel PA (2014) Statin therapy and thromboxane generation in patients with coronary artery disease treated with high-dose aspirin. Thromb Haemost 112(2):323–331. https://doi.org/10.1160/TH14-01-0094
Milos M, Herak D, Kuric L, Horvat I, Zadro R (2009) Evaluation and performance characteristics of the coagulation system: ACL TOP analyzer—HemosIL reagents. Int J Lab Hematol 31(1):26–35. https://doi.org/10.1111/j.1751-553x.2007.00999.x
Bliden KP, DiChiara J, Tantry US, Bassi AK, Chaganti SK, Gurbel PA (2007) Increased risk in patients with high platelet aggregation receiving chronic clopidogrel therapy undergoing percutaneous coronary intervention: is the current antiplatelet therapy adequate? J Am Coll Cardiol 49(6):657–666. https://doi.org/10.1016/j.jacc.2006.10.050
Ndrepepa G, Schuster T, Hadamitzky M, Byrne RA, Mehilli J, Neumann FJ, Richardt G, Schulz S, Laugwitz KL, Massberg S, Schomig A, Kastrati A (2012) Validation of the Bleeding Academic Research Consortium definition of bleeding in patients with coronary artery disease undergoing percutaneous coronary intervention. Circulation 125(11):1424–1431. https://doi.org/10.1161/CIRCULATIONAHA.111.060871
Dukkipati SR, Kar S, Holmes DR, Doshi SK, Swarup V, Gibson DN, Maini B, Gordon NT, Main ML, Reddy VY (2018) Device-related thrombus after left atrial appendage closure. Circulation 138(9):874–885. https://doi.org/10.1161/CIRCULATIONAHA.118.035090
Pracon R, Bangalore S, Dzielinska Z, Konka M, Kepka C, Kruk M, Kaczmarska-Dyrda E, Petryka-Mazurkiewicz J, Bujak S, Solecki M, Pskit A, Dabrowska A, Sieradzki B, Plonski A, Ruzyllo W, Witkowski A, Demkow M (2018) Device thrombosis after percutaneous left atrial appendage occlusion is related to patient and procedural characteristics but not to duration of postimplantation dual antiplatelet therapy. Circ Cardiovasc Interv 11(3):e005997. https://doi.org/10.1161/CIRCINTERVENTIONS.117.005997
Fauchier L, Cinaud A, Brigadeau F, Lepillier A, Pierre B, Abbey S, Fatemi M, Franceschi F, Guedeney P, Jacon P, Paziaud O, Venier S, Deharo JC, Gras D, Klug D, Mansourati J, Montalescot G, Piot O, Defaye P (2018) Device-related thrombosis after percutaneous left atrial appendage occlusion for atrial fibrillation. J Am Coll Cardiol 71(14):1528–1536. https://doi.org/10.1016/j.jacc.2018.01.076
Lempereur M, Aminian A, Freixa X, Gafoor S, Kefer J, Tzikas A, Legrand V, Saw J (2017) Device-associated thrombus formation after left atrial appendage occlusion: a systematic review of events reported with the Watchman, the Amplatzer Cardiac Plug and the Amulet. Catheter Cardiovasc Interv 90(5):E111–E121. https://doi.org/10.1002/ccd.26903
Gurbel PA, Bliden KP, Guyer K, Cho PW, Zaman KA, Kreutz RP, Bassi AK, Tantry US (2005) Platelet reactivity in patients and recurrent events post-stenting: results of the PREPARE POST-STENTING Study. J Am Coll Cardiol 46(10):1820–1826. https://doi.org/10.1016/j.jacc.2005.07.041
Stone GW, Witzenbichler B, Weisz G, Rinaldi MJ, Neumann FJ, Metzger DC, Henry TD, Cox DA, Duffy PL, Mazzaferri E, Gurbel PA, Xu K, Parise H, Kirtane AJ, Brodie BR, Mehran R, Stuckey TD, Investigators A-D (2013) Platelet reactivity and clinical outcomes after coronary artery implantation of drug-eluting stents (ADAPT-DES): a prospective multicentre registry study. Lancet 382(9892):614–623. https://doi.org/10.1016/S0140-6736(13)61170-8
Meus R, Son M, Sobczyk D, Undas A (2016) Prothrombotic state in patients with a left atrial appendage thrombus of unknown origin and cerebrovascular events. Stroke 47(7):1872–1878. https://doi.org/10.1161/STROKEAHA.116.012856
Johnson ED, Schell JC, Rodgers GM (2019) The d-dimer assay. Am J Hematol 94(7):833–839. https://doi.org/10.1002/ajh.25482
Bliden KP, Chaudhary R, Navarese EP, Sharma T, Kaza H, Tantry US, Gurbel PA (2018) Thrombogenicity and central pulse pressure to enhance prediction of ischemic event occurrence in patients with established coronary artery disease: the MAGMA-ischemia score. Atherosclerosis 268:55–62. https://doi.org/10.1016/j.atherosclerosis.2017.11.018
Bliden KP, Raviv G, Tantry US, Chaudhary R, Cochran JW, Navarese EP, Brannan T, Vyas A, Gurbel PA (2019) "Blueprinting" thrombogenicity and antithrombotic drug response at the bedside in patients presenting emergently with symptoms of acute stroke. J Thromb Thrombolysis 47(2):192–199. https://doi.org/10.1007/s11239-019-01813-0
Aradi D, Gross L, Trenk D, Geisler T, Merkely B, Kiss RG, Komocsi A, Dezsi CA, Ruzsa Z, Ungi I, Rizas KD, May AE, Mugge A, Zeiher AM, Holdt L, Huber K, Neumann FJ, Koltowski L, Huczek Z, Hadamitzky M, Massberg S, Sibbing D (2019) Platelet reactivity and clinical outcomes in acute coronary syndrome patients treated with prasugrel and clopidogrel: a pre-specified exploratory analysis from the TROPICAL-ACS trial. Eur Heart J 40(24):1942–1951. https://doi.org/10.1093/eurheartj/ehz202
Gurbel PA, Bliden KP, DiChiara J, Newcomer J, Weng W, Neerchal NK, Gesheff T, Chaganti SK, Etherington A, Tantry US (2007) Evaluation of dose-related effects ofaspirin on platelet function: results from the Aspirin-Induced Platelet Effect (ASPECT) study. Circulation 115(25):3156–3164.
Olson JD (2015) D-dimer: an overview of hemostasis and fibrinolysis, assays, and clinical applications. Adv Clin Chem 69:1–46.
Shahidi M (2017) Thrombosis and von Willebrand factor. Adv Exp Med Biol 906:285–306.
Kattula S, Byrnes JR, Wolberg AS (2017) Fibrinogen and fibrin in hemostasis and thrombosis. Arterioscler Thromb Vasc Biol 37(3):e13–e21.
Undas A (2017) Determination of fibrinogen and thrombin time (TT). Methods Mol Biol 1646:105–110.
Acknowledgements
We wish to acknowledge Andrea Fitzgerald BSN-RN, MA for her contributions to this study
Funding
This study was funded by Boston Scientific Corporation (300 Boston Scientific Way Marlborough, MA).
Author information
Authors and Affiliations
Contributions
MS: Conceptualization, Methodology, Roles/Writing—original draft; KPB: Conceptualization, Data curation, Formal analysis, Roles/Writing—original draft; LI: Methodology, Project administration, Resources; GV: Supervision, Validation, Visualization; AS: Funding acquisition, Investigation, Methodology, Project administration; SY: Formal analysis, Methodology, Software; RM: Conceptualization, Methodology; HR: Project administration, Resources; EPN: Formal analysis, Writing—review & editing; TP: Data curation, Formal analysis; WB: Software, Investigation, Methodology, Project administration; RC: Validation; Visualization, Writing—review & editing; UST: Conceptualization, Data curation, Writing—review & editing, PAG: Conceptualization, Funding acquisition, Investigation, Writing—review & editing.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Gurbel receives honoraria for lectures, consultations, including service on speakers’ bureaus from Bayer, Merck, Janssen, Medicure, and World Medical; receiving grants from the National Institutes of Health, Janssen, Merck, Bayer, Haemonetics, Instrumentation Labs, and Amgen. Dr. Gurbel is holding stock or stock options in Merck, Medtronic, and Pfizer; and holding patents in the area of personalized antiplatelet therapy and interventional cardiology. Dr. Sherwood receives honoraria from Medtronic. Dr. Navarese reports honoraria and payment for lectures from Astra Zeneca, Daiichi Sankyo/Lilly, Sanofi-Regeneron and Amgen; and receipt of grants from Amgen. Dr. Batchelor reports honoraria from Boston Scientific Corporation. Other authors report no disclosures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sherwood, M., Bliden, K.P., Ilkhanoff, L. et al. Detailed thrombogenicity phenotyping and 1 year outcomes in patients undergoing WATCHMAN implantation: (TARGET-WATCHMAN) a case–control study. J Thromb Thrombolysis 50, 484–498 (2020). https://doi.org/10.1007/s11239-020-02205-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-020-02205-5