Abstract
Venous thromboembolism (VTE) is an important cause of morbidity and mortality in Western countries. The incidence rate of VTE is estimated at 1–2 cases per 1000 annually. This study was a population-based cohort study of previously treatment naïve patients with a first occurrence of venous thromboembolism (VTE), using data from the administrative health data register of the Stockholm Region 2011–2018. Data on anticoagulant treatment was taken from the Swedish Prescribed Drug Register. We also analyzed all VTE events between 2011 and 2018. Altogether 14,849 naïve incident VTE cases were identified. In 2011 the majority of patients with a first episode of VTE were prescribed warfarin versus non-vitamin K antagonist oral anticoagulants (NOACs), 1144 versus 5. In contrast in 2018, the majority of patients were treated with NOACs, 1049 versus 59 treated with warfarin. Treatment with low molecular weight heparin only decreased from 814 to 683 patients. The frequency of all VTE events in the population increased over time from 1.88/1000 to 1.93/1000 (p = 0.072), and PE diagnoses increased from 0.69/1000 to 0.76/1000 (p = 0.003). In conclusion, during 2011–2018 there has been a shift of prescription of warfarin to a clear predominance of NOACs in the treatment of VTE in the Stockholm Region, in line with current recommendations. In the clinical situation, treatment has been simplified as monitoring of warfarin has decreased substantially. PE events increased during the time period in the population even if the increase was rather modest, while all VTE events did not increase significantly.
Similar content being viewed by others
Highlights
-
Venous thromboembolism (VTE) is an important cause of morbidity and mortality
-
Population-based cohort study from Stockholm Region of patients with VTE 2011-2018
-
Anticoagulant treatment has shifted from warfarin to NOACs during the period
-
Pulmonary embolism has increased during the period
-
Further studies especially on the association to cancer are warranted
Introduction
Venous thromboembolism (VTE) is an important cause of morbidity and mortality in Western countries, with an incidence rate of 1–2 cases per 1000 and year [1,2,3,4,5,6,7]. In Sweden, the incidence of deep venous thrombosis (DVT) is estimated at 1.67 per 1000 per year, with pulmonary embolism (PE) 0.8 per 1000 per year [8].
Both acquired and genetic risk factors contribute to the risk of VTE [9, 10]. A large proportion of VTE develop after previous hospitalizations and surgical procedures [11]. Important acquired risk factors for VTE include [9,10,11]: age, major surgery, trauma, immobilization, malignancy, prior VTE, presence of central venous lines, chronic heart failure, estrogen therapy, pregnancy and the post-partum period. Age is a major risk factor for VTE independent of gender [2]. A recently published large study with 1.1 million participants from 76 different cohorts, found that older age, smoking, and adiposity were consistently associated with higher VTE risk [12].
There have been different and somewhat contradictory results in studies regarding incidence of VTE, with a review concluding, that “the occurrence of VTE seems to be relatively constant, or even increasing” [7]. One study from the US showed an increased incidence [6], while a French study found a decreased incidence [3]. The latter study found different trends as regards DVT and PE, with a decreased incidence of DVT but not of PE.
The aim of the present study was to explore the anticoagulant treatment and incidence of VTE in Region Stockholm especially regarding time trends.
Method
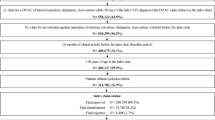
This study was a population-based cohort study of previously treatment naïve patients with a first occurrence of venous thromboembolism (VTE; for ICD-10 codes see Supplementary Table 1) using data from the administrative health data register of Region Stockholm (Vårdanalysdatabasen, VAL), i.e., the regional healthcare data warehouse [13,14,15,16]. It contains anonymized data regarding diagnoses, age, sex, prescription claims, hospitalizations and other healthcare consultations, migration and death for all individuals in the region (2.3 million inhabitants). Data regarding diagnoses from primary care is available since 2003, and for secondary care (outpatient visits and hospitalization) since 1993. VAL also contains individual level data on all prescription drugs dispensed anywhere in Sweden to inhabitants in the region since July 2010: amounts, expenditures and reimbursement, the age and gender of the patient, co-payments and prescriber category. This information is derived from the Swedish Prescribed Drug Register (National Board of Health and Welfare) [17, 18]. The study was approved by the Regional Ethical Review Board in Stockholm (EPN Dnr: 4-1/2018).
The index date of individuals with a first occurrence of VTE (See Supplementary Table 1) in secondary care from 2011 to 2018 was identified. Patients with an index date during the period January 1st 2011 until December 31st 2018 and a first claim of either an oral anticoagulant (OAC) or low-molecular weight heparin (LMWH) within ± 30 days of the index date were included. The wash-out period to define a new introduction of an OAC or LMWH was 6 months. The individuals were considered treated with OAC when both an OAC and LMWH were claimed. Individuals with a previous VTE diagnosis earlier than 2011 were excluded, as well as patients with VTE during pregnancy or post-partum period (ICD-10 codes O22.2, O22.3, O22.5, O22.9, and O87).
Age at index date was used for further analyses. Co-morbidity was defined as at least one registration of each diagnosis (ICD-code) as either a main or a secondary diagnosis in either primary or secondary care (outpatient visits and hospitalization) during 5 years up until the index date. Other drugs at baseline were included if they were claimed during 6 months prior up until the index date of the OAC of inclusion. See Supplementary Table 1 for definitions of co-morbidity diagnoses (with ICD-10 codes) and Supplementary Table for drug treatments (with ATC codes).
Statistical analysis
Baseline data were registered, with means and standard deviations or numbers and frequencies for men and women. Use of anticoagulant medications were registered, with warfarin, low molecular weight heparin or NOACs, both for all treatment naïve VTE cases as well as for cases with a previous registered cancer. Type of previous cancer was also noted.
We also calculated the incidence rate of all diagnoses of VTE and PE, with or without a claim of either an oral anticoagulant (OAC) or low-molecular weight heparin (LMWH) within ± 30 days of the index date during the time period regardless of earlier treatment, using direct age standardization in the population at risk. Time trend for registered diagnoses over time were estimated by linear regression models.
Results
In Table 1 the identified cases of VTE among men and women in Region Stockholm 2011–2018 are shown, with age profile and registered comorbidity (comorbidity ICD-10 codes in Supplementary Table 1). The mean age in this study was 69.0 years for women and in men 65.0 years and the majority of patients were older than 60 years. Few cases of VTE were diagnosed in children. Data regarding comorbidities showed high proportions; i.e. 68.0% of the patients suffered from hypertension, 24.8% of the patients had cancer, 20.2% diabetes mellitus, 18.7% stroke, 17.5% heart failure, and finally 16.8% had atrial fibrillation.
The distribution of the identified newly diagnosed VTE cases by year, and anticoagulant treatment, is shown in Table 2 (ATC codes in Supplementary Table 2). Treatment shifted markedly over time, with a decreased use of warfarin and an increased use of NOACs. Patients with a previous cancer registered were more often treated by LMVH compared to all VTE cases, 65.7% versus 39.9%. Numbers and frequencies of associated cancer cases are shown in Supplementary Table 3. The highest proportions of registered cancers exceeding 10% were skin cancer (19.5%), prostate cancer (18.4%), breast cancer (14.6%), and metastatic cancers (metastatic lymph node 13.9%, metastasis in lung, thorax, liver or other gastrointestinal organs 13.8%, and other sites of metastasis 10.5%).
All registered VTE diagnoses categorized according to age group during the time period are shown in Table 3. When using age-standardized data, the total number was 31,219, i.e., around three times as many as the registered new cases, with 12,027 PE diagnoses. The frequency of VTE diagnoses increased from 1.88/1000 to 1.93/1000 (p value for linear trend = 0.072), with a mean frequency of 1.90 (SD 0.021); and of PE diagnoses from 0.69/1000 to 0.76/1000 (p-value for linear trend 0.003), with a mean frequency of 0.73 (SD 0.034). When also using a claim of either an oral anticoagulant (OAC) or low-molecular weight heparin (LMWH) within ± 30 days of the index date, the frequency of VTE diagnoses remained on the same level, i.e., 1.61/1000 (p-value for linear trend 0.39), with a mean over the years of 1.60/1000 (SD 0.026); and of PE diagnoses 0.60/1000 to 0.65/1000 (p-value for linear trend 0.007), with a mean over the years of 0.63/1000 (SD 0.028).
Most cases of VTE occurred in the age-group 60–79 years, 45.1%, followed by the age-group 40–59 years, 24.7%, and the age-group 80–99 years, 19.6% (data without age standardization, Supplementary Table 4). Most of the PE cases also occurred in the age-group 60–79 years, 49.5%, followed by the age-group 80–99 years, 22.7%, and the age-group 40–59 years, 20.1% (data without age standardization, Supplementary Table 5). The total population in Region Stockholm over the years 2011–2018 are given in Supplementary Table 6.
Discussion
The main findings of this study was a clear shift in treatment of VTE during 2011–2018 from predominantly warfarin in the beginning of the time period to predominantly NOACs at the end of the time period. We also found a trend with an increasing rate of PE events during the time period 2011–2018, while not of all VTE events.
Regarding the time trend for VTE and PE diagnoses, earlier studies have observed conflicting results, with an increased incidence in a US study [6], and a decreased incidence in a French study [3]. We found an incidence of all VTE cases of around 1.9 per 1000 inhabitants, compared to 0.66 per 1000 inhabitants in the study of the city of Malmö in southern Sweden [19]. The incidence of PE cases was approximately 0.7 per 1000 inhabitants, compared to 0.2 per 1000 in the Malmö study. In an earlier study the incidence of DVT in the city of Malmö was 1.9 per 1000 inhabitants [1], i.e., higher than in the study by Isma et al. [19], and also higher than in the present study, i.e., around 1.2 cases of DVT per 1000 inhabitants. The incidence of DVT in a US study was close to that in the study by Nordström et al. i.e., 1.9 per 1000 inhabitants [20].
This register study included 14,189 cases from Region Stockholm with a first episode of VTE during 2011–2018. To our knowledge this is one of the largest studies in this field. Age distribution and distribution between sexes is in accordance with other studies. The number of children with VTE was low which also is in accordance with other published results. Cancer is a well-known risk-factor for VTE as shown by our data. Other cardiovascular co-morbidities were also common, especially hypertension.
The observed shift in anticoagulant treatment pattern, with a strongly decreased use of warfarin and an increased use of NOACs has already been shown for treatment in atrial fibrillation during the same time period [21, 22]. Recommendations for treatment with anticoagulation of VTE is available on the so called Wise List [23], which is an official recommendations which strongly affects prescription patterns in Region Stockholm [24]. The first recommendation for NOAC for treatment of VTE was official in December 2014 and influenced prescription pattern for VTE thereafter.
A review and meta-analysis of NOACs versus warfarin in patients with VTE or atrial fibrillation concluded, that the risk of major bleeding events decreased by between 32 and 69% for dabigatran, rivaroxaban, and apixaban compared with vitamin K antagonists, based on 7 RCTs [25]. Furthermore, the risk of intracranial bleedings decreased by between 61 and 86% of NOACs with the exception of dabigatran. According to a review, PE incidence rates seem to increase over time, “possibly due to increased monitoring, improved diagnosis and an aging population” [26]. Furthermore, in the same review was concluded, that NOACs seem to exert advantages over warfarin, especially in some subgroups, such as elderly, fragile patients, and also patients at high risk of recurrent VTE events, or patients with high risk of bleeding complications.
The age distribution pattern differed between all VTE cases and PE cases, with the peak in higher ages for PE cases.
This study has some limitations. This is an observational study, why causal associations could not be claimed. Data are taken from registers, without access to other clinical data, such as smoking, BMI, blood pressure or laboratory values. Misclassification is reported to be relatively common in VTE, especially in DVT [27]. In a recent publication from Sweden 2450 VTE diagnoses was validated manually [28]. Misclassification of VTE diagnosis was reported to occur in 16.4% of DVT-cases and in 1.1% of PE-cases. Thus, data on DVT should be interpreted with some caution. However, we also used treatment data, which give our result further strength [29], and we had also access to all registered VTE and PE diagnoses during the time period.
Our study also has strengths. It is a large study with more than 14,000 cases included in the main study. Overall the Swedish registers are known to be of high quality, including the Swedish Prescribed Drug Register [17, 18]. The VAL register in Region Stockholm includes diagnoses from both hospital care, primary care and other open specialist care, and has been used in several other studies, including atrial fibrillation [15], and studies of other diagnoses [30]. Furthermore, Region Stockholm has a population of 2.3 million inhabitants.
In the clinical situation, treatment has been simplified as monitoring of warfarin has decreased substantially. Besides, treatment with anticoagulants could also be offered to more sub-groups, such as frail, elderly patients, and patients at high risk of recurring VTE events or high risk of bleeding complications, when considering the lower risk of bleeding complications.
In conclusion, we found a shift in treatment from of warfarin to a predominance of NOACs during the last decade. We found a slight increase in rate of PE cases in Region Stockholm. Further follow-up in relation to treatment complications, including bleeding events with different treatments, is warranted. Besides, further analyses of VTE events in relation to different cancers are warranted, especially on the time aspect, i.e., whether a VTE event could be the first sign of a cancer, or if VTE events occur later on after a cancer diagnosis.
References
Nordstrom M, Lindblad B, Bergqvist D, Kjellstrom T (1992) A prospective study of the incidence of deep-vein thrombosis within a defined urban population. J Intern Med 232:155–160
Silverstein MD, Heit JA, Mohr DN, Petterson TM, O’Fallon WM, Melton LJ 3rd (1998) Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch Intern Med 158:585–593
Delluc A, Tromeur C, Le Ven F, Gouillou M, Paleiron N, Bressollette L et al (2016) Current incidence of venous thromboembolism and comparison with 1998: a community-based study in Western France. Thromb Haemost 116:967–974
Oger E (2000) Incidence of venous thromboembolism: a community-based study in Western France. EPI-GETBP Study Group. Groupe d’Etude de la Thrombose de Bretagne Occidentale. Thromb Haemost 83:657–660
Tagalakis V, Patenaude V, Kahn SR, Suissa S (2013) Incidence of and mortality from venous thromboembolism in a real-world population: the Q-VTE Study Cohort. Am J Med 126(832):e13–e21
Huang W, Goldberg RJ, Anderson FA, Kiefe CI, Spencer FA (2014) Secular trends in occurrence of acute venous thromboembolism: the Worcester VTE study (1985-2009). Am J Med 127(829–39):e5
Heit JA, Spencer FA, White RH (2016) The epidemiology of venous thromboembolism. J Thromb Thrombolysis 41:3–14
Johansson M, Johansson L, Lind M (2014) Incidence of venous thromboembolism in northern Sweden (VEINS): a population-based study. Thromb J 12:6
Rosendaal FR (1999) Venous thrombosis: a multicausal disease. Lancet 353:1167–1173
Anderson FA Jr, Spencer FA (2003) Risk factors for venous thromboembolism. Circulation 107:I9–I16
Spencer FA, Emery C, Lessard D, Anderson F, Emani S, Aragam J et al (2006) The worcester venous thromboembolism study: a population-based study of the clinical epidemiology of venous thromboembolism. J Gen Intern Med 21:722–727
Gregson J, Kaptoge S, Bolton T, Pennells L, Willeit P, Burgess S et al (2019) Cardiovascular risk factors associated with venous thromboembolism. JAMA Cardiol 4:163–173
Forslund T, Wettermark B, Andersen M, Hjemdahl P (2017) Stroke and bleeding with non-vitamin K antagonist oral anticoagulant or warfarin treatment in patients with non-valvular atrial fibrillation: a population-based cohort study. Europace 20(3):420–428
Forslund T, Wettermark B, Hjemdahl P (2016) Comparison of treatment persistence with different oral anticoagulants in patients with atrial fibrillation. Eur J Clin Pharmacol 72:329–338
Forslund T, Wettermark B, Wandell P, von Euler M, Hasselstrom J, Hjemdahl P (2013) Risk scoring and thromboprophylactic treatment of patients with atrial fibrillation with and without access to primary healthcare data: experience from the Stockholm health care system. Int J Cardiol 170:208–214
Forslund T, Wettermark B, Wandell P, von Euler M, Hasselstrom J, Hjemdahl P (2014) Risks for stroke and bleeding with warfarin or aspirin treatment in patients with atrial fibrillation at different CHA(2)DS(2)VASc scores: experience from the Stockholm region. Eur J Clin Pharmacol 70:1477–1485
Wallerstedt SM, Wettermark B, Hoffmann M (2016) The first decade with the Swedish Prescribed Drug Register - a systematic review of the output in the scientific literature. Basic Clin Pharmacol Toxicol 119:464–469
Wettermark B, Hammar N, Fored CM, Leimanis A, Otterblad Olausson P, Bergman U et al (2007) The new Swedish Prescribed Drug Register–opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf 16:726–735
Isma N, Svensson PJ, Gottsater A, Lindblad B (2009) Prospective analysis of risk factors and distribution of venous thromboembolism in the population-based Malmo Thrombophilia Study (MATS). Thromb Res 124:663–666
Cushman M, Tsai AW, White RH, Heckbert SR, Rosamond WD, Enright P et al (2004) Deep vein thrombosis and pulmonary embolism in two cohorts: the longitudinal investigation of thromboembolism etiology. Am J Med 117:19–25
Komen J, Forslund T, Hjemdahl P, Andersen M, Wettermark B (2017) Effects of policy interventions on the introduction of novel oral anticoagulants in Stockholm: an interrupted time series analysis. Br J Clin Pharmacol 83:642–652
Komen J, Forslund T, Hjemdahl P, Wettermark B (2017) Factors associated with antithrombotic treatment decisions for stroke prevention in atrial fibrillation in the Stockholm region after the introduction of NOACs. Eur J Clin Pharmacol 73:1315–1322
Gustafsson LL, Wettermark B, Godman B, Andersen-Karlsson E, Bergman U, Hasselstrom J et al (2011) The ‘wise list’- a comprehensive concept to select, communicate and achieve adherence to recommendations of essential drugs in ambulatory care in Stockholm. Basic Clin Pharmacol Toxicol 108:224–233
Eriksen J, Gustafsson LL, Ateva K, Bastholm-Rahmner P, Ovesjo ML, Jirlow M et al (2017) High adherence to the ‘Wise List’ treatment recommendations in Stockholm: a 15-year retrospective review of a multifaceted approach promoting rational use of medicines. BMJ Open 7:e014345
Almutairi AR, Zhou L, Gellad WF, Lee JK, Slack MK, Martin JR et al (2017) Effectiveness and safety of non-vitamin K antagonist oral anticoagulants for atrial fibrillation and venous thromboembolism: a systematic review and meta-analyses. Clin Ther 39(1456–78):e36
Howard LS (2018) Non-vitamin K antagonist oral anticoagulants for pulmonary embolism: who, where and for how long? Expert Rev Respir Med 12:387–402
Casez P, Labarere J, Sevestre MA, Haddouche M, Courtois X, Mercier S et al (2010) ICD-10 hospital discharge diagnosis codes were sensitive for identifying pulmonary embolism but not deep vein thrombosis. J Clin Epidemiol 63:790–797
Ohman L, Johansson M, Jansson JH, Lind M, Johansson L (2018) Positive predictive value and misclassification of diagnosis of pulmonary embolism and deep vein thrombosis in Swedish patient registries. Clin Epidemiol 10:1215–1221
Sanfilippo KM, Wang TF, Gage BF, Liu W, Carson KR (2015) Improving accuracy of international classification of diseases codes for venous thromboembolism in administrative data. Thromb Res 135:616–620
Carlsson AC, Wandell P, Osby U, Zarrinkoub R, Wettermark B, Ljunggren G (2013) High prevalence of diagnosis of diabetes, depression, anxiety, hypertension, asthma and COPD in the total population of Stockholm, Sweden - a challenge for public health. BMC Public Health 13:670
Acknowledgement
Open access funding provided by Karolinska Institute.
Author information
Authors and Affiliations
Contributions
PW, TF and MH designed the study; TF analyzed the data, and all authors participated in the interpretation of data; PW, TF and MH drafted the manuscript and all other authors revised it critically for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Wändell, P., Forslund, T., Danin Mankowitz, H. et al. Venous thromboembolism 2011–2018 in Stockholm: a demographic study. J Thromb Thrombolysis 48, 668–673 (2019). https://doi.org/10.1007/s11239-019-01966-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-019-01966-y