Abstract
To review the use of the direct oral anticoagulant (DOAC) agents in inherited thrombophilia based on the literature. MEDLINE, International Pharmaceutical Abstracts, and Google Scholar searches (1970–May 2016) were conducted for case reports, case series, retrospective cohorts, or clinical trials using the key words: protein C deficiency, protein S deficiency, antithrombin deficiency, activated protein C resistance, Factor V Leiden, hypercoagulable, NOACs, dabigatran, apixaban, rivaroxaban, betrixaban, edoxaban, Xa inhibitor, direct thrombin inhibitor. Results were limited to English-only articles. Clinical studies evaluating the use of DOACs for hypercoagulable states related to inherited thrombophilia were selected and evaluated. Thrombophilia, a predisposition to thrombosis, manifests predominantly as venous thromboembolism. Causes of inherited thrombophilia include antithrombin deficiency, deficiencies of proteins C and S, and Factor V Leiden mutation. Many patients with thrombophilia receive anticoagulant therapy for primary or secondary prevention of VTE, historically either warfarin or a heparin product. DOAC’s have been considered as potential alternatives to traditional agents based on their pharmacologic activity. Case reports and a post-hoc analysis of a clinical trial have indicated positive results in patients with inherited thrombophilia and VTE. Positive results have been reported for the use of DOACs in inherited thrombophilia. Further robust studies are needed for definitive decision making by clinicians.
Similar content being viewed by others
References
Rosendaal FR (1999) Venous thrombosis: a multicausal disease. The Lancet 353(9159):1167–1173
Couturaud F, Leroyer C, Julian JA et al (2009) Factors that predict risk of thrombosis in relatives of patients with unprovoked venous thromboembolism. Chest J 136(6):1537–1545
Tait RC, Walker ID, Perry DJ, Islam SI, Daly ME, McCall F, Conkie JA, Carrell RW (1994) Prevalence of antithrombin deficiency in the healthy population. Br J Haematol 87(1):106–112
Koster T, Rosendaal FR, de Ronde H, Briet E, Vandenbroucke JP, Bertina RM (1993) Venous thrombosis due to poor anticoagulant response to activated protein C: Leiden Thrombophilia Study. Lancet 342:1503–1506
Ridker PM, Miletich JP, Hennekens CH, Buring JE (1997) Ethnic distribution of factor V Leiden in 4047 men and women. Implications for venous thromboembolism screening. JAMA 277:1305–1307
Stefano VD, Finazzi G, Mannucci PM (1996) Inherited thrombophilia: pathogenesis, clinical syndrome, and management. Blood 87(9):3531–3544
Dykes AC, Walker ID, Mcmahon AD, Islam SI, Tait RC (2001) A study of Protein S antigen levels in 3788 healthy volunteers: influence of age, sex and hormone use, and estimate for prevalence of deficiency state. Br J Haematol 113(3):636–641
Khan S, Dickerman JD (2006) Hereditary thrombophilia. Thromb J 4:15
Cohoon KP, Heit JA (2014) Inherited and secondary thrombophilia: clinician update. Circulation 129(2):254–257
Heit JA (2007) Thrombophilia: common questions on laboratory assessment and management. Hematol Am Soc Hematol Educ Progr 2007:127–35
Kearon C et al (2016) Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest J 149(2):315–352
Kearon C et al (2012) Antithrombotic therapy for VTE Disease: antithrombotic therapy and prevention of thrombosis: American College of Chest Physicians evidence-based clinical practice guidelines. Chest J 141(2 suppl):e419S–e494S
Schulman S, Kearon C, Kakkar AK et al (2009) Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med 361(24):2342–2352
Bauersachs R, Berkowitz SD, Brenner B et al (2010) Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med 363(26):2499–2510
Buller HR, Decousus H, Hokusai- VTE Investigators et al (2013) Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. N Engl J Med 369(15):1406–1415
Schulman S, Kakkar AK, Goldhaber SZ et al (2014) Treatment of acute venous thromboembolism with dabigatran or warfarin and pooled analysis. Circulation 129(7):764–772
Agnelli G, Buller HR, Cohen A et al (2013) Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med 369(9):799–808
Buller HR, Prins MH, EINSTEIN- EP Investigators et al (2012) Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med 366(14):1287–1297
van Es N, Coppens M, Schulman S, Middeldorp S, Buller HR (2014) Direct oral anticoagulants compared with vitamin K antagonists for acute venous thromboembolism: evidence from phase 3 trials. Blood 124(12):1968–1975
Holster IL, Valkhoff VE, Kuipers EJ, Tjwa ET (2013) New oral anticoagulants increase risk for gastrointestinal bleeding: a systematic review and meta-analysis. Gastroenterology 145(1):105–112
Gomez-Outes A, Terleira-Fernandez AI, Lecumberri R, Suarez-Gea ML, Vargas-Castrillon E (2014) Direct oral anticoagulants in the treatment of acute venous thromboembolism: a systematic review and meta-analysis. Thromb Res 134(4):774–782
Fox BD, Kahn SR, Langleben D, Eisenberg MJ, Shimony A (2012) Efficacy and safety of novel oral anticoagulants for treatment of acute venous thromboembolism: direct and adjusted indirect meta-analysis of randomised controlled trials. BMJ 345:e7498
van der Hulle T, Kooiman J, den Exter PL, Dekkers OM, Klok FA, Huisman MV (2014) Effectiveness and safety of novel oral anticoagulants as compared with vitamin K antagonists in the treatment of acute symptomatic venous thromboembolism: a systematic review and meta-analysis. J Thromb Haemost 12(3):320–328
Mantha S, Ansell J (2015) Indirect comparison of dabigatran, rivaroxaban, apixaban and edoxaban for the treatment of acute venous thromboembolism. J Thromb Thrombolysis 39(2):155–165
Chai-Adisaksopha C, Crowther M, IsayamaT (2014) Lim W The impact of bleeding complications in patients receiving target-specific oral anticoagulants: a systematic review and meta-analysis. Blood 124(15):2450–2458
Wu C, Alotaibi GS, Alsaleh K, Linkins LA (2015) Sean McMurtry M Case-fatality of recurrent venous thromboembolism and major bleeding associated with aspirin, warfarin, and direct oral anticoagulants for secondary prevention. Thromb Res 135(2):243–248
Castellucci LA, Cameron C, Le Gal G et al (2014) Clinical and safety outcomes associated with treatment of acute venous thromboembolism: a systematic review and meta-analysis. JAMA 312(11):1122–1135
Arachchillage DJ, Cohen H (2013) Use of new oral anticoagulants in antiphospholipid syndrome. Curr Rheumatol Rep 15:331–340
Signorelli F, Nogueira F, Domingues V, Mariz HA, Levy RA (2015) Thrombotic events in patients with antiphospholipid syndrome treated with rivaroxaban: a series of eight cases. Clin Rheumatol. http://link.springer.com/article/10.1007%2Fs10067-015-3030-y. Accessed 6 Sept 2016
Win K, Rodgers GM (2014) New oral anticoagulants may not be effective to prevent venous thromboembolism in patients with antiphospholipid syndrome. Am J Hematol 89:1017
Schaefer JK, McBane RD, Black DF, Williams LN, Moder KG, Wysokinski WE (2014) Failure of dabigatran and rivaroxaban to prevent thromboembolism in antiphospholipid syndrome: a case series of three patients. Thromb Haemost 112:947–950
Son M, Wypasek E, Celinska-Lowenhoff M, Undas A (2015) The use of rivaroxaban in patients with antiphospholipid syndrome: a series of 12 cases. Thromb Res 135:1035–1036
Mavrakanas T, Bounameaux H (2011) The potential role of new oral anticoagulants in the prevention and treatment of thromboembolism. Pharmacol Ther 130(1):46–58
Chan NC, Bhagirath V, Eikelboom JW (2015) Profile of betrixaban and its potential in the prevention and treatment of venous thromboembolism. Vasc Health Risk Manag 11:343–351
Hermans C, Eeckhoudt S (2012) Lambert, C Dabigatran etexilate (Pradaxa®) for preventing warfarin-induced skin necrosis in a patient with severe protein C deficiency. Thromb Haemost 107:1189–1191
Wypasek E, Potaczek, DP, Alhenc-Gelas M, Undas A (2014) PROS1 mutations associated with protein S deficiency in Polish patients with residual vein obstruction on rivaroxaban therapy. Thromb Res 134:199–201
Martinelli I, Mannucci PM, De Stefano V, Taioli E, Rossi V, Crosti F, Paciaroni K, Leone G, Faioni EM (1998) Different risks of thrombosis in four coagulation defects associated with inherited thrombophilia: a study of 150 families. Blood 92(7):2353–2358
Cook RM, Rondina MT, Horton DJ (2014) Rivaroxaban for the long-term treatment of spontaneous ovarian vein thrombosis caused by factor V leiden homozygosity. Ann Pharm 48(8):1055–1060
Plander M, Szendrei T, Bodó I, Iványi JL (2015) Successful treatment with rivaroxaban of an extended superficial vein thrombosis in a patient with acquired antithrombin deficiency due to Peg-asparaginase treatment. Ann Hematol 94:1257–1258
Schulman S, Kearon C, Kakkar AK et al (2013) RE-MEDY Trial Investigators; RE-SONATE Trial Investigators. Extended use of dabigatran, warfarin, or placebo in venous thromboembolism. N Engl J Med 368(8):709–718
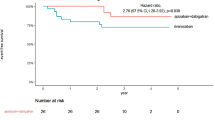
Schulman S, Eriksson H, Goldhaber SZ et al (2014) Influence of Thrombophilia on the efficacy of dabigatran versus warfarin for extended treatment of acute venous thromboembolism in RE-MEDY. Blood 124(21):1544
Hohnloser SH, Oldgren J, Yang S et al (2012) Myocardial ischemic events in patients with atrial fibrillation treated with dabigatran or warfarin in the RE-LY (Randomized Evaluation of Long-Term Anticoagulation Therapy) trial. Circulation 125:669–676
Mak KH (2012) Coronary and mortality risk of novel oral antithrombotic agents: a meta-analysis of large randomised trials. BMJ Open 2:e001592
EINSTEIN Investigators, Bauersachs R, Berkowitz SD, Brenner B, Buller HR, Decousus H et al (2010) Oral rivaroxaban for symptomatic venous thromboembolism (and supplementary appendix). N Engl J Med 363:2499–2510
EINSTEIN- PE Investigators, Büller HR, Prins MH, Lensin AW, Decousus H, Jacobson BF et al (2012) Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med 366:1287–1297
Ruis-Irastorza G, Crowther M, Branch W, Khamashta MA (2010) Antiphospholipid syndrome. The Lancet 376:1498–1509
Fawole A, Daw HA, Crowther MA (2013) Practical management of bleeding due to the anticoagulants dabigatran, rivaroxaban, and apixaban. Cleve Clin J Med 80(7):443–451
Dabigatran Lexi-drugs. Lexicomp. Wolters Kluwer Health, Inc., Hudson. http://online.lexi.com. Accessed 8 Mar 2016
Rivaroxaban Lexi-drugs. Lexicomp. Wolters Kluwer Health, Inc., Hudson. http://online.lexi.com. Accessed 8 Mar 2016
Apixaban Lexi-drugs. Lexicomp. Wolters Kluwer Health, Inc., Hudson. http://online.lexi.com. Accessed 8 Mar 2016.
Edoxaban Lexi-drugs. Lexicomp. Wolters Kluwer Health, Inc., Hudson. http://online.lexi.com. Accessed 8 Mar 2016
Martinuzzo ME, Barrera LH, D’adamo MA, Otaso JC, Gimenez MI, Oyhamburu J (2013) Frequent false-positive results of lupus anticoagulant tests in plasmas of patients receiving the new oral anticoagulants and enoxaparin. Int J Lab Hematol. doi:10.1111/ijlh.12138
Eby C (2013) Novel anticoagulants and laboratory testing. Int J Lab Hematol 35:262–268
Nakashima MO, Rogers HJ (2014) Hypercoagulable states: an algorithmic approach to laboratory testing and update on monitoring of direct oral anticoagulants. Blood Res 49(2):85–94
Rivaroxaban [package insert] (2011) Janssen Pharmaceuticals, Inc., Titusville
Apixaban [package insert] (2012) Bristol-Myers Squibb Company, Princeton
Edoxaban [package insert] (2015) Daiichi Sankyo, Inc., Parsippany
Dabigatran [package insert] (2015) Boehringer Ingelheim Pharmaceuticals, Inc., Ridgefield
January CT, Wann LS, Alpert JS et al (2014) AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 64:e1–e76
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest to disclose amongst the authors.
Rights and permissions
About this article
Cite this article
Skelley, J.W., White, C.W. & Thomason, A.R. The use of direct oral anticoagulants in inherited thrombophilia. J Thromb Thrombolysis 43, 24–30 (2017). https://doi.org/10.1007/s11239-016-1428-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-016-1428-2