Abstract
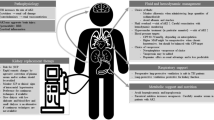
Cerebral edema and elevated intracranial pressure (ICP) are common complications of acute brain injury. Hypertonic solutions are routinely used in acute brain injury as effective osmotic agents to lower ICP by increasing the extracellular fluid tonicity. Acute kidney injury in a patient with traumatic brain injury and elevated ICP requiring renal replacement therapy represents a significant therapeutic challenge due to an increased risk of cerebral edema associated with intermittent conventional hemodialysis. Therefore, continuous renal replacement therapy (CRRT) has emerged as the preferred modality of therapy in this patient population. We present our current treatment approach, with demonstrative case vignette illustrations, utilizing hypertonic saline protocols (3% sodium-chloride or, with coexisting severe combined metabolic and respiratory acidosis, with 4.2% sodium-bicarbonate) in conjunction with the CRRT platform, to induce controlled hypernatremia of approximately 155 mEq/L in hemodynamically unstable patients with acute kidney injury and elevated ICP due to acute brain injury. Rationale, mechanism of activation, benefits and potential pitfalls of the therapy are reviewed. The impact of hypertonic citrate solution during regional citrate anticoagulation is specifically discussed. Maintaining plasma hypertonicity in the setting of increased ICP and acute kidney injury could prevent the worsening of ICP during renal replacement therapy by minimizing the osmotic gradient across the blood-brain barrier and maximizing cardiovascular stability.

Similar content being viewed by others
Change history
06 May 2019
The authors would like to report an error in the formula describing the correction factor for the protein content in the serum/plasma.
Abbreviations
- ABI:
-
acute brain injury
- AKI:
-
acute kidney injury
- BUN:
-
blood urea nitrogen
- CRRT:
-
continuous renal replacement therapy
- ICP:
-
intracranial pressure
- ICU:
-
intensive care unit
- Na+ :
-
sodium
- RRT:
-
Renal replacement therapy
- CRRT:
-
Continuous renal replacement therapy
References
Fülöp T, Abdul Salim S, Zsom L. Regional citrate anticoagulation for continuous renal replacement therapy without post-filter monitoring of ionized calcium. J Renal Inj Prev. 2018;7(3):139–43.
Grant IS, Andrews PJ. ABC of intensive care: neurological support. Br Med J. 1999;319(7202):110–3.
White H, Cook D, Venkatesh B. The use of hypertonic saline for treating intracranial hypertension after traumatic brain injury. Anesth Analg. 2006;102(6):1836–46.
Vialet R, Albanèse J, Thomachot L, Antonini F, Bourgouin A, Alliez B, et al. Isovolume hypertonic solutes (sodium chloride or mannitol) in the treatment of refractory posttraumatic intracranial hypertension: 2 mL/kg 7.5% saline is more effective than 2 mL/kg 20% mannitol. Crit Care Med. 2003;31(6):1683–7.
Koenig MA, Bryan M, Lewin JL 3rd, Mirski MA, Geocadin RG, Stevens RD. Reversal of transtentorial herniation with hypertonic saline. Neurology. 2008;70(13):1023–9.
Bertrand Y, Hermant A, Mahieu P, Roels J. Intracranial pressure changes in patients with head trauma during haemodialysis. Intensive Care Med. 1983;9(6):321–3.
Trachtman H, Futterweit S, Tonidandel W, Gullans SR. The role of organic osmolytes in the cerebral cell volume regulatory response to acute and chronic renal failure. J Am Soc Nephrol. 1993;3(12):1913–9.
Lin C-M, Lin J-W, Tsai J-T, Ko C, Hung K-S, Hung CC, et al. Intracranial pressure fluctuation during hemodialysis in renal failure patients with intracranial hemorrhage. Reconstructive Neurosurgery: Springer; 2008. p. 141–4.
Goldsmith DJ, Forni LG, Hilton PJ. Bicarbonate therapy and intracellular acidosis. Clin Sci (Lond). 1997;93(6):593–8.
Davenport A, Will EJ, Losowsky MS. Rebound surges of intracranial pressure as a consequence of forced ultrafiltration used to control intracranial pressure in patients with severe hepatorenal failure. Am J Kidney Dis. 1989;14(6):516–9.
Davenport A. Renal replacement therapy for the patient with acute traumatic brain injury and severe acute kidney injury. Acute Kidney Inj. 2007;156: Karger Publishers:333–9.
Gharaibeh KA, Brewer JM, Agarwal M, Fulop T. Risk factors, complication and measures to prevent or reverse catastrophic sodium overcorrection in chronic hyponatremia. Am J Med Sci. 2015;349(2):170–5.
Nguyen MK, Kurtz I. Determinants of plasma water sodium concentration as reflected in the Edelman equation: role of osmotic and Gibbs-Donnan equilibrium. Am J Physiol-Renal Physiol. 2004;286(5):F828–F37.
Nguyen MK, Kurtz I. Quantitative interrelationship between Gibbs-Donnan equilibrium, osmolality of body fluid compartments, and plasma water sodium concentration. J Appl Physiol 2017.
Petitclerc T, Goux N, Reynier AL, Bene B. A model for non-invasive estimation of in vivo dialyzer performances and patient's conductivity during hemodialysis. Int J Artif Organs. 1993;16(8):585–91.
Keep R, Andjelkovic A, Xi G. Cytotoxic and Vasogenic Brain Edema. Primer on Cerebrovascular Diseases (Second Edition): Elsevier; 2017. p. 145–9.
Donkin JJ, Vink R. Mechanisms of cerebral edema in traumatic brain injury: therapeutic developments. Curr Opin Neurol. 2010;23(3):293–9.
Saw MM, Chamberlain J, Barr M, Morgan MP, Burnett JR, Ho KM. Differential disruption of blood–brain barrier in severe traumatic brain injury. Neurocrit Care. 2014;20(2):209–16.
Oertel M, Kelly DF, Lee JH, McArthur DL, Glenn TC, Vespa P, et al. Efficacy of hyperventilation, blood pressure elevation, and metabolic suppression therapy in controlling intracranial pressure after head injury. J Neurosurg. 2002;97(5):1045–53.
Brain Trauma Foundation: Guidelines for the management of traumatic brain injury. J Neurotrauma. 2007;24((Suppl 1)):S1–106.
Miller JD, Leech P. Effects of mannitol and steroid therapy on intracranial volume-pressure relationships in patients. J Neurosurg. 1975;42(3):274–81.
Worthley LI, Cooper DJ, Jones N. Treatment of resistant intracranial hypertension with hypertonic saline. Report of two cases. J Neurosurg. 1988;68(3):478–81.
Bayr H, Clark RS, Kochanek PM. Promising strategies to minimize secondary brain injury after head trauma. Crit Care Med. 2003;31(1):S112–S7.
Sakellaridis N, Pavlou E, Karatzas S, Chroni D, Vlachos K, Chatzopoulos K, et al. Comparison of mannitol and hypertonic saline in the treatment of severe brain injuries. J Neurosurg. 2011;114(2):545–8.
Jagannatha AT, Sriganesh K, Devi BI, Rao GS. An equiosmolar study on early intracranial physiology and long term outcome in severe traumatic brain injury comparing mannitol and hypertonic saline. J Clin Neurosci. 2016;27:68–73.
Li M, Chen T, Chen SD, Cai J, Hu YH. Comparison of equimolar doses of mannitol and hypertonic saline for the treatment of elevated intracranial pressure after traumatic brain injury: a systematic review and meta-analysis. Medicine (Baltimore). 2015;94(17):e736.
Gu J, Huang H, Huang Y, Sun H, Xu H. Hypertonic saline or mannitol for treating elevated intracranial pressure in traumatic brain injury: a meta-analysis of randomized controlled trials. Neurosurg Rev. 2018:1–11.
Dorman HR, Sondheimer JH, Cadnapaphornchai P. Mannitol-induced acute renal failure. Medicine. 1990;69(3):153–9.
Fang L, You H, Chen B, Xu Z, Gao L, Liu J, et al. Mannitol is an independent risk factor of acute kidney injury after cerebral trauma: a case–control study. Ren Fail. 2010;32(6):673–9.
Kaufmann AM, Cardoso ER. Aggravation of vasogenic cerebral edema by multiple-dose mannitol. J Neurosurg. 1992;77(4):584–9.
Murphy N, Auzinger G, Bernel W, Wendon J. The effect of hypertonic sodium chloride on intracranial pressure in patients with acute liver failure. Hepatology. 2004;39(2):464–70.
Qureshi AI, Suarez JI. Use of hypertonic saline solutions in treatment of cerebral edema and intracranial hypertension. Crit Care Med. 2000;28(9):3301–13.
Himmelseher S. Hypertonic saline solutions for treatment of intracranial hypertension. Curr Opin Anaesthesiol. 2007;20(5):414–26.
Tan SK, Kolmodin L, Sekhon MS, Qiao L, Zou J, Henderson WR, et al. The effect of continuous hypertonic saline infusion and hypernatremia on mortality in patients with severe traumatic brain injury: a retrospective cohort study. Can J Anaesth. 2016;63(6):664–73.
Rhee H, Jang KS, Shin MJ, Lee JW, Kim IY, Song SH, et al. Use of multifrequency bioimpedance analysis in male patients with acute kidney injury who are undergoing continuous veno-venous hemodiafiltration. PLoS One. 2015;10(7):e0133199.
Arieff AI, Guisado R, Massry SG, Lazarowitz VC. Central nervous system pH in uremia and the effects of hemodialysis. J Clin Invest. 1976;58(2):306–11.
Rao CPV, Bershad EM, Calvillo E, Maldonado N, Damani R, Mandayam S, et al. Real-time noninvasive monitoring of intracranial fluid shifts during Dialysis using volumetric integral phase-shift spectroscopy (VIPS): a proof-of-concept study. Neurocrit Care. 2018;28(1):117–26.
Silver SM, Sterns RH, Halperin ML. Brain swelling after dialysis: old urea or new osmoles? Am J Kidney Dis. 1996;28(1):1–13.
Ronco C, Bellomo R, Brendolan A, Pinna V, La Greca G. Brain density changes during renal replacement in critically ill patients with acute renal failure. Continuous hemofiltration versus intermittent hemodialysis. J Nephrol. 1999;12(3):173–8.
Trinh-Trang-Tan MM, Cartron JP, Bankir L. Molecular basis for the dialysis disequilibrium syndrome: altered aquaporin and urea transporter expression in the brain. Nephrol Dial Transplant. 2005;20(9):1984–8.
Davenport A. Renal replacement therapy in the patient with acute brain injury. Am J Kidney Dis. 2001;37(3):457–66.
Osgood M, Compton R, Carandang R, Hall W, Kershaw G, Muehlschlegel S. Rapid unexpected brain herniation in association with renal replacement therapy in acute brain injury: caution in the neurocritical care unit. Neurocrit Care. 2015;22(2):176–83.
Kumar A, Cage A, Dhar R. Dialysis-induced worsening of cerebral edema in intracranial hemorrhage: a case series and clinical perspective. Neurocrit Care. 2015;22(2):283–7.
Fülöp T, Zsom L, Tapolyai MB, Molnar MZ, Rosivall L. Volume-related weight gain as an independent indication for renal replacement therapy in the intensive care units. J Renal Inj Prev. 2017;6(1):35–42.
Tolwani AJ, Wille KM. The clinical application of CRRT—current status: anticoagulation for continuous renal replacement therapy. Semin Dial. 2009;22(2):141–5.
Fletcher JJ, Bergman K, Carlson G, Feucht EC, Blostein PA. Continuous renal replacement therapy for refractory intracranial hypertension? J Trauma. 2010;68(6):1506–9.
Rifkin SI, Malek AR, Behrouz R. Use of hypertonic continuous Venovenous Hemodiafiltration to control intracranial hypertension in an end-stage renal disease patient. Int J Nephrol. 2010;2010:1–2.
Lund A, Damholt MB, Strange DG, Kelsen J, Moller-Sorensen H, Moller K. Increased intracranial pressure during hemodialysis in a patient with anoxic brain injury. Case Rep Crit Care. 2017;2017:5378928.
Medow JE, Sanghvi SR, Hofmann RM. Use of high-flow continuous renal replacement therapy with citrate anticoagulation to control intracranial pressure by maintaining hypernatremia in a patient with acute brain injury and renal failure. Clin Med Res. 2015;13(2):89–93.
Meier-Kriesche HU, Gitomer J, Finkel K, DuBose T. Increased total to ionized calcium ratio during continuous venovenous hemodialysis with regional citrate anticoagulation. Crit Care Med. 2001;29(4):748–52.
e Silva, VTC, Caires RA, Bezerra JS, Costalonga EC, Oliveira APL, de Oliveira Coelho F, et al. Use of regional citrate anticoagulation for continuous venovenous hemodialysis in critically ill cancer patients with acute kidney injury. J Crit Care. 2018.
Maguigan KL, Dennis BM, Hamblin SE, Guillamondegui OD. Method of hypertonic saline administration: effects on osmolality in traumatic brain injury patients. J Clin Neurosci. 2017;39:147–50.
van den Ancker W, Haagen IA, van der Voort PH. Direct sodium measurement prevents underestimation of hyponatremia in critically ill patients. Intensive Care Med. 2015;41(3):553–4.
Aiyagari V, Deibert E, Diringer MN. Hypernatremia in the neurologic intensive care unit: how high is too high? J Crit Care. 2006;21(2):163–72.
Koch CA, Fülöp T. Clinical aspects of changes in water and sodium homeostasis in the elderly. Rev Endocr Metab Disord. 2017;18(1):49–66.
Darmon M, Timsit J-F, Francais A, Nguile-Makao M, Adrie C, Cohen Y, et al. Association between hypernatraemia acquired in the ICU and mortality: a cohort study. Nephrol Dial Transplant. 2010;25(8):2510–5.
Hoffman H, Jalal MS, Chin LS. Effect of hypernatremia on outcomes after severe traumatic brain injury: a Nationwide inpatient sample analysis. World Neurosurg. 2018;118:e880–e6.
Khanna S, Davis D, Peterson B, Fisher B, Tung H, O'quigley J, et al. Use of hypertonic saline in the treatment of severe refractory posttraumatic intracranial hypertension in pediatric traumatic brain injury. Crit Care Med. 2000;28(4):1144–51.
Hirsch KG, Spock T, Koenig MA, Geocadin RG. Treatment of elevated intracranial pressure with hyperosmolar therapy in patients with renal failure. Neurocrit Care. 2012;17(3):388–94.
Maggiore U, Picetti E, Antonucci E, Parenti E, Regolisti G, Mergoni M, et al. The relation between the incidence of hypernatremia and mortality in patients with severe traumatic brain injury. Crit Care. 2009;13(4):R110.
Kumar AB, Shi Y, Shotwell MS, Richards J, Ehrenfeld JM. Hypernatremia is a significant risk factor for acute kidney injury after subarachnoid hemorrhage: a retrospective analysis. Neurocrit Care. 2015;22(2):184–91.
Chang S, Lee TH. Beyond evidence-based medicine. N Engl J Med. 2018;379(21):1983–5.
Koch CA, Fulop T. Case reports: old-timers and evergreens. J Med Case Rep. 2018;12(1):355.
Annoni F, Fontana V, Brimioulle S, Creteur J, Vincent JL, Taccone FS. Early effects of enteral urea on intracranial pressure in patients with acute brain injury and hyponatremia. J Neurosurg Anesthesiol. 2017;29(4):400–5.
Acknowledgements
Parts of this projects has been presented in poster format at the 2018 Annual Dialysis Conference, March 3-6, 2018, Orlando, FL and at the 14th International Conference on Continuous Renal Replacement Therapies, Feb 25-28, 2009, San Diego, CA (Blood Purif 2009; 27:271-305). Case vignette #1 was observed at the University of Mississippi Medical Center, while Drs. Fülöp, Koch, and Zsom were serving on the faculty of the Department of Medicine. Drs. Rafael D. Rodríguez and Jorge O. Chabrier-Rosello are current Nephrology trainee at the Department of Medicine, Medical University of South Carolina, SC (Class of 2019).
We sincerely appreciated the assistance of Mr. Attila Lénárt-Muszka during editing and grammar review.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Dr. Zsom is a current employee of Fresenius Medical Care (FMC) Hungary and Dr. Fülöp is a former employee of FMC Hungary. Dr. Fülöp is a current employee of the United States Veterans Health Administration. However, the views and opinions expressed herewith do not reflect the official views or opinion or endorsed by the FMC Hungary or the United States Veteran Health Administrations. None of the other authors declares a conflict of interest with this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Implication for health policy/practice/research/medical education
Cerebral edema and elevated intracranial pressure represent a significant management challenge in those with co-existing acute brain and kidney injury. When artificial renal support is required, continuous renal replacement therapy is the preferred modality for these critically ill patients. Herewith, we demonstrate our approaches to administer hypertonic saline solution along with commercially available replacement fluid when conducting continuous veno-venous hemofiltration or hemodialysis, to circumvent the development or progression of elevated intracranial pressure in a patient with brain injury requiring renal replacement therapy.
Rights and permissions
About this article
Cite this article
Fülöp, T., Zsom, L., Rodríguez, R.D. et al. Therapeutic hypernatremia management during continuous renal replacement therapy with elevated intracranial pressures and respiratory failure. Rev Endocr Metab Disord 20, 65–75 (2019). https://doi.org/10.1007/s11154-019-09483-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11154-019-09483-2