Abstract
Purpose
Complications following upper gastrointestinal (UGI) surgery are common. Symptom-monitoring following discharge is not standardized. An electronic patient-reported outcome (ePRO) system providing feedback to patients and clinicians could support patients and improve outcomes. Little is known about patients’ experiences of using such systems. This qualitative sub-study explored patients’ perspectives of the benefits of using a novel ePRO system, developed as part of the mixed methods eRAPID pilot study, to support recovery following discharge after UGI surgery.
Methods
Patients completed the online ePRO symptom-report system post-discharge. Weekly interviews explored patients’ experiences of using ePRO, the acceptability of feedback generated and its value for supporting their recovery. Interviews were audio-recorded and targeted transcriptions were thematically analysed.
Results
Thirty-five interviews with 16 participants (11 men, mean age 63 years) were analysed. Two main themes were identified: (1) reassurance and (2) empowerment. Feelings of isolation were common; many patients felt uninformed regarding their expectations of recovery and whether their symptoms warranted clinical investigation. Participants were reassured by tailored feedback advising them to contact their care team, alleviating their anxiety. Patients reported feeling empowered by the ePRO system and in control of their symptoms and recovery.
Conclusion
Patients recovering at home following major cancer surgery regarded electronic symptom-monitoring and feedback as acceptable and beneficial. Patients perceived that the system enhanced information provision and provided a direct link to their care team. Patients felt that the system provided reassurance at a time of uncertainty and isolation, enabling them to feel in control of their symptoms and recovery.
Similar content being viewed by others
Introduction
Recovery from upper gastrointestinal (UGI) cancer surgery is associated with distressing and difficult symptoms that can occur for up to six months after hospital discharge [1–3]. Up to 50% of patients experience complications within one month of surgery [3–5], frequently after they have left hospital [6, 7]. Symptoms and complications during the initial recovery period can have negative impacts on health-related quality of life (HRQL) for up to 5 years post-surgery [5] and can range from pain, fatigue and nausea [8] to respiratory failure, sepsis and wound infections [9–12].
Patients are increasingly being discharged from hospital earlier following surgery, with an increased emphasis on recovery at home [13, 14]. Although earlier discharge can be feasible and safe [15, 16], patients’ symptoms are not usually routinely monitored post-discharge [17]. Evidence to support early discharge tends to focus on clinical outcomes rather than patient experiences [18]. Research suggests that patients find it difficult to obtain symptom management advice once they are at home [18]. Relevant verbal or written information is usually provided to patients pre-operatively or prior to discharge [19]. However, the shift towards earlier discharge may mean that current methods of pre-discharge education are no longer sufficient for effective patient self-management of symptoms [13]. Furthermore, incomplete understanding of patterns of recovery after discharge can cause patients to experience uncertainty and concern about how to recognise and respond to symptoms [13]. Uncertainty and a feeling of “going it alone” during recovery can have a significant detrimental impact on patients’ experience of recovery. Recent research shows, for example, that patients often report feelings of confusion and abandonment following discharge [20].
Electronic platforms to collect patient-reported outcome measures offer an efficient means for patients to report symptom data once they have left hospital. Monitoring of symptoms through the routine collection of electronic patient-reported outcome measures has been shown to enhance the detection of complications in cancer patients during treatment [21, 22]. Emerging evidence indicates that personalised electronic patient-reported outcome interventions providing tailored information post-discharge may lead to a quicker return to normal activities after surgery [23], improved HRQL and survival in cancer patients [24, 25]. However, there has been little qualitative research focusing on patients’ experiences of using such systems to support symptom management.
As part of the eRAPID project we have developed a novel electronic patient-reported outcome (ePRO) symptom-report and feedback system to improve recovery in patients who have been discharged from hospital following UGI cancer-related surgery. The development of the eRAPID system for use by breast cancer chemotherapy and pelvic radiotherapy patients has been described previously [26–28]. A prospective mixed methods pilot study has established the feasibility of the UGI surgery specific ePRO system, demonstrating that it is acceptable to patients and clinicians [26, 29]. Here we report the findings from the qualitative work that formed part of this pilot study, the aim of which was to understand participants’ experiences and perceptions of using the ePRO system after hospital discharge following UGI cancer-related surgery to support their symptom management.
Methods
The ePRO system
The IT elements include a patient-facing website incorporating a symptom-report questionnaire and enables secure transfer of data to EHR, allowing clinicians to view symptom reports [27]. All questionnaire items were selected from relevant EORTC modules. The development of symptom severity threshold algorithms and generation of feedback is described in detail elsewhere [26]. Briefly, scoring thresholds were developed and iteratively refined with input from clinicians (Cancer Nurse Specialists, Dietitians and Surgeons) and patients, and with data from qualitative interviews with Cancer Nurse Specialist and quantitative data from completed patient self-report questionnaires. The ePRO system provides tailored feedback to patients based on the severity of their reported symptoms to the online symptom-report questionnaire. Feedback is dependent on symptom severity and includes symptom self-management advice appropriate to their stage of recovery or advice to contact health care professionals (HCP) if symptoms are clinically concerning. The system is integrated into hospital electronic records, enabling clinicians to access real-time individual symptom reports and graphs. When concerning symptoms are reported, clinicians receive an automated alert email instructing them to review symptom reports and contact the participant. Participants are provided with graphs illustrating how their individual symptoms change over time. The types of feedback generated by the ePRO system are illustrated in Table 1.
Participants
This mixed methods prospective pilot study was conducted at Bristol Royal Infirmary University Hospitals Bristol NHS Foundation Trust. Consecutive patients who had undergone UGI surgery between August 2017 and March 2018 were screened for eligibility from inpatient clinic lists by a hospital research nurse. Eligibility criteria included patients who had undergone UGI cancer-related surgery, had access to a computer/mobile device and the internet at home, were ready for hospital discharge to their home, were over 18 and were fluent in English. Participants were eligible for inclusion if they had undergone oesophageal gastric (e.g. oesophagectomy, gastrectomy) or hepato-pancreato-biliary (e.g. Whipples, hepatectomy) surgeries. These criteria were established based on developmental work that identified similar patient recovery and clinical care pathways for these patient groups [26].
Data collection
The data for this qualitative study were collected as part of a wider mixed methods pilot study. Patients were approached by a research nurse when they were ready for discharge. Eligible patients were given a participant information leaflet and the opportunity to ask questions, and those wishing to participate provided written informed consent. Participants were asked to complete the ePRO system questionnaire twice in the first week and weekly for eight weeks post-discharge and all were asked to take part in telephone interviews at these timepoints. All interviews were conducted by HR and/or AP. HR is an experienced mixed methods Senior Research Associate and AP is a Research Nurse and Cancer Nurse Specialist. Quantitative data relating to ePRO system response rates, symptom data and clinical outcomes were collected and are reported elsewhere [29].
Weekly telephone interviews
Semi-structured telephone interviews were conducted weekly for eight weeks to coincide with completions of the ePRO system. All participants were interviewed regarding their use of the ePRO system and, in accordance with the principles of targeted transcription [32], only those interviews in which participants discussed using the ePRO system within the context of symptom management were transcribed for qualitative analysis. For example, data from weekly interviews where participants had not experienced symptoms or where only yes/no responses were obtained were not transcribed (see “Data analysis” section). Telephone interviews generally took place when the participant was at home and all participants consented to audio recording.
Interviews focussed on participants’ experiences of using the ePRO system and the type of feedback they had received. The interview guides were adapted from pilot work relating to the development of the ePRO system [26] and is provided in Online Appendix 1. Participants were asked about how suitable they found the advice they had received. For example, when participants had received a prompt to contact an HCP, they were asked whether (and reasons why) they had or had not made contact and what the outcome of any contact had been. AP and/or HR made notes during telephone interviews, and this data was used to contextualise the interview transcripts during coding. Weekly interviews were generally 5–20 min in duration.
End-of-study interviews
A subset of approximately 10% of participants were invited to a face-to-face interview once they had completed the 8-week follow-up period. Participants were selected in order to represent a range of patient experiences of using the system, including those who had fully or partially engaged with the system, and those who had and had not experienced post-discharge complications. These interviews were conducted and audio-recorded in the participant’s homes by HR and AP. End-of-study interviews were of 1–1.5 h in duration.
Data analysis
Thematic analysis was conducted in accordance with Braun & Clarke’s guidelines [30]. Thematic analysis is a flexible and widely used method for analysing qualitative data, by which underlying themes and concepts are identified, derived and interpreted within the wider context of the data. Thematic analysis was chosen because the research question focused on patients’ perceptions and experiences of using the ePRO system within the context of their symptom management at home, as well as within established clinical care pathways. Thematic analysis provides a theoretically flexible approach useful for such pragmatic situations where it is necessary to contextualise findings, within both the experiential and interpretative realities of the participant, and the more positivist scope of an existing healthcare system [31]. All end-of-study interviews were transcribed verbatim. Audio recordings of all weekly interviews were reviewed several times by HR and AP. While it was not feasible to transcribe all of these interview transcripts verbatim, only those weekly interviews in which participants discussed data of relevance to the research question (i.e. received symptom management advice from the ePRO system) were transcribed verbatim. This form of targeted transcription is recognised as a pragmatic means of analysing large numbers of interviews by focusing on data most relevant to the research question [32]. HR and AP discussed and identified interviews relevant for verbatim transcription. HR was familiarised with the data by re-reading transcripts multiple times. Descriptive codes were identified within the data and organised using NVivo 12 software. Codes were examined and interpreted to identify overarching themes which were reviewed within the context of the data using methods of constant comparison. HR coded all the data and themes were reviewed by KA for coherency and consistency with the data. Regular meetings were held with the core study team (HR, AP & KA) to discuss emerging findings. Analysis was conducted until thematic saturation was reached and no new themes were emergent from codes [33]. As this was a pragmatic feasibility study and the qualitative data were collected as part of a wider mixed methods study it was not feasible to invite participants to comment on findings.
Results
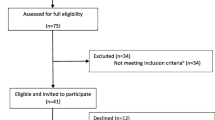
In total 109 patients were screened for eligibility, of which 41 (38%) were eligible and invited to participate, and 29 (71%) consented (mean age 64 years, standard deviation (SD) 9 years, range 43–81, 19 men). All 29 participants were interviewed at least once following discharge. Seven participants withdrew from the study because they felt too tired or unwell to continue (n = 6) or due to a prolonged hospital readmission (n = 1). An additional six participants took part in telephone interviews but did not provide data relevant for analysis. As such these interviews were not included in the analysis. The analysis reported here focuses on data collected from 35 weekly and three end-of-study interviews carried out with the remaining 16 study participants. Fifteen participants received ePRO advice to contact an HCP relating to concerning symptoms and three were readmitted to hospital following discharge due to adverse events. The frequency of reported symptoms, ePRO system actions, hospital readmissions and clinical outcome data for the full pilot study are reported elsewhere [29]. Participant demographics and clinical details are reported in Table 2.
Participants described the ePRO system to be quick, easy and straightforward to use, confirming the findings from the pilot study [26]. All participants described the ePRO system as a positive adjunct to their recovery. Although the ePRO measure was developed from a widely used and validated questionnaire [26], some participants discussed factors commonly associated with questionnaires, such as the inflexibility of response options, the repetitive nature of answering questions repeatedly and receiving the same outcome/advice multiple times. Despite these observations, participants felt that these were unavoidable issues for all questionnaires that did not adversely impact on their experiences of using the system.
Two overarching themes were identified from the thematic analysis: Reassurance and Empowerment. Figure 1 provides an overview of interrelated and independent themes and sub-themes. Table 3 provides examples of patient quotations supporting the identified themes.
Theme 1: Reassurance
Participants described the ePRO system as reassuring for several reasons relating to uncertainties about the clinical significance of symptoms, isolation experienced following hospital discharge, and providing a means of tracking the progress of their recovery. These sub-themes are detailed below.
Isolation and uncertainty after discharge
By providing advice to contact their care teams, the ePRO system acted as a link to HCPs. Some participants felt that they were “on their own” once they were at home. This was confounded by patients’ uncertainties regarding the causes, meaning and significance of the symptoms they were experiencing, and at what point they should contact HCPs. In this context, ePRO reassured them that contacting HCPs was an appropriate decision.
PT 1224 “So [ePRO system] makes you feel not cut off…Because otherwise I think the issue can be you get all this attention in hospital, and then suddenly that’s it – you’re off on your own.”
Some participants felt uncertain about what symptoms they were likely to experience and what to expect during their recovery. Many attributed these feelings to a lack of information provision prior to discharge.
PT 1209 “When I first came home, I was a bit surprised by the fact that I wasn’t really given much in the way of guidance. As to what to expect, in terms of…the symptoms I might experience when I came home, and what I should or shouldn’t do…”
For some, this led to anxiety regarding whether their symptoms were ‘normal’ for their stage of recovery, leading them to question how well they were managing. In these instances, the ePRO self-management advice reassured participants that their symptoms were typical.
PT 1208 “[The ePRO system] confirms that in the [tailored feedback] that that’s normal for this period of time in your development so I find that, the [tailored symptom advice] at the end quite reassuring.”
ePRO system advice to contact HCP
Participants reported barriers to contacting HCPs, including uncertainties regarding whether their symptoms were clinically concerning. Many described the ePRO system prompts as reassuring by supporting them to overcome these barriers. Some participants were confident about recognising severe symptoms (e.g. fevers and infections) but were unsure if they should contact HCPs regarding more ambiguous symptoms such as pain, fatigue and wound problems. Although participants were aware of how to contact HCPs, ePRO system prompts gave them confidence that their symptoms warranted contacting their care team.
PT 1219 “I spoke to the [cancer nurse specialist] and she put me in touch with the dietitian. But that all followed on from my completing a questionnaire, so it prompted me to do it I think.”
While ePRO system feedback acted as a prompt to contact HCPs, data from weekly interviews with Cancer Nurse Specialists (reported elsewhere, Richards [29]) suggests that it did not result in participants making additional unnecessary calls to their care teams. When participants were already in contact with HCPs and felt that their symptoms were being appropriately managed, or had upcoming clinical appointments, many reported that they did not make additional calls to clinicians.
PT 1224 “Well as I had an appointment…this morning…I didn’t see any need to call anybody.”
When participants did contact HCPs following ePRO system feedback, this often resulted in clinical interventions such as additional appointments or new prescriptions, or additional reassurance and advice.
PT 1213 “[The cancer nurse specialist] said I’m going to ring your GP…and they rang me back and said we’ll do a blood test.”
Progress
For many participants, using the ePRO system enabled them to see recovery as a process instead of focussing on the individual experiences of distressing symptoms. The system provided relevant and useful advice for managing their symptoms, and a means of monitoring their progress during recovery. Participants reported that the individual symptom graphs generated by the ePRO system accurately reflected their experiences and described these as beneficial for tracking recovery. Graphs confirmed that they were improving and provided a means of acknowledging how their symptoms had changed since hospital discharge, enabling them to observe patterns and understand their symptoms in context.
PT 1226 “You don’t see them in isolation as one week, you see [graphs of symptom reports] as a pattern of progress and that’s the way to look at them…when I look along the row from where I was to begin with to now where most [symptoms] are at zero I’m pleased.”
Theme 2: Empowerment
The ePRO system enabled participants to appropriately manage their symptoms and feel more in control of their recovery and health. In this way, reassurance provided by the ePRO system empowered participants’ in their recovery, providing advice relevant to their symptoms that reflected their experiences. Participants talked about following the advice (e.g. food portion size, pain management and activity pacing), and how this helped them better manage their symptoms and recovery.
PT 1224 “[When] you’re having a bit of difficulty you can then look at the suggested actions [and tailored advice] you can take to alleviate those symptoms.”
The advice confirmed whether participants’ symptoms were typical, eased their anxiety and increased their confidence in their ability to manage their recovery.
PT 1226 “I go through the questionnaire and by the time I’ve finished…I’m comfortable in my own mind, and therefore I don’t need to go searching elsewhere [online for information about symptoms]…I actually don’t worry unnecessarily…[the tailored advice] just showed me that it was exactly the right thing to do…Because I think it helps towards recovery, rather than just dealing with it myself.”
The usefulness of the ePRO system advice was underpinned by participants’ feelings that it was tailored specifically for their symptoms. Participants felt like it was “aimed” at them, and that the advice was appropriate and achievable.
PT 1208 “At the end it all sort of comes together and it gives you advice…It works well…and aimed at me specifically.”
The ePRO system enhanced information provision by ensuring participants had instant access to relevant symptom self-management advice. For many participants, the ePRO system advice prompted them to recall information they had received from clinicians earlier on in their recovery, but which they had subsequently forgotten. This was the case for symptom management strategies, and for prescribed medications.
PT 1242 “I must have read it [patient information leaflet] in the first week or so and I’d forgotten all about it. Yeah…[I’ll] try to follow that [ePRO system] advice…It’s reminded me and [I’ve] thought I have got some medication for that, I should be taking it.”
Discussion
This study explored patients’ experiences and perceptions of using an electronic symptom-report and feedback system to improve recovery following UGI cancer-related surgery. The ePRO system provides tailored self-management feedback depending on the severity of reported symptoms. Participants reported that the ePRO system enhanced their recovery at home by providing reassuring advice regarding their symptoms and when to contact HCPs, thereby empowering patients to manage their recovery.
A key theme was the reassuring role of the advice to contact HCPs in participants’ decision-making. Some participants were unsure about whether they should contact HCPs, often because of uncertainties relating to the relative severity of their symptoms and an unwillingness to “bother” clinicians. Uncertainties about contacting HCPs outside of routine appointments has been associated with delays in help seeking [34] which can lead to delays in the detection of AEs following surgery [35]. Although participants in this study knew how to contact their care team, being prompted by the ePRO system encouraged them to do so. Other studies have demonstrated that uncertainties about what to expect post-discharge can result in patients and carers expressing a constant need for reassurance from HCPs [13]. However, by providing relevant and reassuring guidance to participants about when it was appropriate to contact HCPs, or when symptoms could instead be self-managed, the ePRO system enabled participants to make informed decisions. Similar themes of reassurance and increasing confidence in decision-making have been reported by participants using the eRAPID system during chemotherapy treatment [36].
Consistent with previous research, participants felt that they lacked information about symptoms management necessary to support them during their recovery [18, 37], and experienced uncertainties and isolation following discharge from hospital [13, 20]. Doubts regarding how to obtain advice during recovery can result in feelings of vulnerability and anxiety [18]. In this study, feelings of isolation were buffered to some extent by engagement with the ePRO system, with participants describing it as a link to HCPs and to relevant symptom management advice. The tailored advice enabled participants to gain more understanding of what to expect from their symptoms and during recovery. Accurate expectations of recovery after major cancer surgery have been shown to have a positive impact on patients, and can reduce worry and negative thoughts [38]. Surgery patients have reported anxieties regarding what they perceived to be insufficient information provision and preparation prior to hospital discharge [13]. Indeed, it is well documented that patients are often unable to recall medical information provided to them by clinicians [39–43]. This effect is confounded in surgical patients by the cognitive impairments associated with anaesthesia, intensive care treatment [44] and symptoms such as fatigue, pain and sleep deprivation [45], all of which can negatively affect information retention and accurate recall. Electronic methods of delivering personalised, real-time self-management education for surgical patients can overcome some of these barriers [45], improve shared decision-making [46] and improve post-operative health outcomes [47].
Patient empowerment can be described as “the patients’ subjective sense of control over their own disease and treatment management” [48]. Participants in this study described the ePRO system advice as helping them to maintain a sense of control over their recovery. This reassurance enabled them to acknowledge improvements in their symptoms over time and reduced their anxiety about identifying ‘normal’ symptoms for their stage of recovery. Similarly, improvements in HRQL have been associated with patients’ perceived ability to take control of their recovery instead of feeling that their symptoms are controlling their lives [38]. Participants’ reported that, by providing tailored and reassuring advice about self-management strategies and guidance on when to contact HCPs, the ePRO system empowered them, helping them to address feelings of isolation and uncertainty often experienced by surgical patients after leaving hospital.[18, 20, 38].
This study has several limitations that should be considered when interpreting the results. This was a single centre study of a specific patient group, which may potentially limit the transferability of these findings to other groups. In this cohort, incidence of post-operative severe AEs was relatively low. This may indicate that these participants had more favourable experiences of recovery. Although interview data from three participants who had been readmitted to hospital due to adverse events were included in this analysis, it was not possible to obtain qualitative data from all participants who became very unwell or were readmitted due to e.g. participant withdrawal or prolonged readmissions. Future work should focus on this group of patients to determine the extent to which such electronic symptom reporting systems are feasible for patients who develop severe complications. Targeted transcription is a cost and time-effective approach to analysing qualitative data; however, it does introduce a risk that not all relevant data were analysed. To reduce this risk, several team members reviewed audio files to ensure all pertinent data was transcribed. In addition, it is important to note that only data from participants who received feedback from the ePRO system and those who completed the study were analysed. Understanding the views of those who withdraw or did not fully engage with the ePRO system could have provided some additional insights, which may have differed from those reported here. Additionally, all electronic systems pose a potential barrier for engagement amongst patients due to language, literacy and access to electronic devices. As eligibility criteria for this study included fluency in English and home internet access, findings are not transferable to groups outside of these criteria.
These findings have implications for clinicians and policy makers in terms of enhancing the provision of symptom management information for patients and empowering them to feel more in control of their recovery at home. The ePRO system was found to be feasible and useful for patients. A multicentre RCT is planned to examine to effectiveness of the ePRO system in UGI cancer-related surgery patients.
Conclusion
Upper gastrointestinal cancer-related surgery patients found the ePRO symptom-monitoring and feedback system to be acceptable and reassuring during their recovery at home. Participants’ reported that, by providing self-management advice tailored to individual symptoms, the ePRO system addressed their anxieties and uncertainties relating to their recovery. Patients described feeling more in control of their recovery while using the ePRO system and experienced it as a link to their care teams. Participants’ felt that the ePRO system enhanced patient information provision relating to management of symptoms, by providing real-time access to advice and improving recall of guidance provided to them while in hospital.
References
Scarpa, M., Valente, S., Alfieri, R., Cagol, M., Diamantis, G., Ancona, E., et al. (2011). Systematic review of health-related quality of life after esophagectomy for esophageal cancer. World Journal of Gastroenterology, 17(42), 4660–4674. https://doi.org/10.3748/wjg.v17.i42.4660.
Trudel, J. G., Sulman, J., Atenafu, E. G., Kidane, B., & Darling, G. E. (2016). Longitudinal evaluation of trial outcome index scores in patients with esophageal cancer. Annals of Thoracic Surgery, 102(1), 269–275. https://doi.org/10.1016/j.athoracsur.2016.01.091.
Viklund, P., Wengstrom, Y., Rouvelas, I., Lindblad, M., & Lagergren, J. (2006). Quality of life and persisting symptoms after oesophageal cancer surgery. European Journal of Cancer, 42(10), 1407–1414. https://doi.org/10.1016/j.ejca.2006.02.005.
Daly, J. M., Fry, W. A., Little, A. G., Winchester, D. P., McKee, R. F., Stewart, A. K., et al. (2000). Esophageal cancer: Results of an American College of Surgeons Patient Care Evaluation Study. The Journal of the American College of Surgeons, 190(5), 562–572; discussion 572–563. https://doi.org/10.1016/s1072-7515(00)00238-6.
Derogar, M., Orsini, N., Sadr-Azodi, O., & Lagergren, P. (2012). Influence of major postoperative complications on health-related quality of life among long-term survivors of esophageal cancer surgery. Journal of Clinical Oncology, 30(14), 1615–1619. https://doi.org/10.1200/JCO.2011.40.3568.
Adam, U., Makowiec, F., Riediger, H., Schareck, W. D., Benz, S., & Hopt, U. T. (2004). Risk factors for complications after pancreatic head resection. American Journal of Surgery, 187(2), 201–208. https://doi.org/10.1016/j.amjsurg.2003.11.004.
DeOliveira, M. L., Winter, J. M., Schafer, M., Cunningham, S. C., Cameron, J. L., Yeo, C. J., et al. (2006). Assessment of complications after pancreatic surgery: A novel grading system applied to 633 patients undergoing pancreaticoduodenectomy. Annals of Surgery, 244(6), 931–937; discussion 937–939. https://doi.org/10.1097/01.sla.0000246856.03918.9a.
Audit, N. O.-G. C. (2017). An audit of the care received by people with Oesophago-Gastric Cancer in England and Wales 2017 Annual Report. National Oesophago-Gastric Cancer Audit.
Balentine, C. J., Naik, A. D., Robinson, C. N., Petersen, N. J., Chen, G. J., Berger, D. H., et al. (2014). Association of high-volume hospitals with greater likelihood of discharge to home following colorectal surgery. JAMA Surg, 149(3), 244–251. https://doi.org/10.1001/jamasurg.2013.3838.
Li, L. T., Barden, G. M., Balentine, C. J., Orcutt, S. T., Naik, A. D., Artinyan, A., et al. (2015). Postoperative transitional care needs in the elderly an outcome of recovery associated with worse long-term survival. Annals of Surgery, 261(4), 695–701. https://doi.org/10.1097/Sla.0000000000000673.
Lightner, A. M., Glasgow, R. E., Jordan, T. H., Krassner, A. D., Way, L. W., Mulvihill, S. J., et al. (2004). Pancreatic resection in the elderly. Journal of the American College of Surgeons, 198(5), 697–706. https://doi.org/10.1016/j.jamcollsurg.2003.12.023.
Sacks, G. D., Lawson, E. H., Dawes, A. J., Gibbons, M. M., Zingmond, D. S., & Ko, C. Y. (2015). Which patients require more care after hospital discharge? An analysis of post-acute care use among elderly patients undergoing elective surgery. The Journal of the American College of Surgeons, 220(6), 1113–1121. https://doi.org/10.1016/j.jamcollsurg.2015.02.029.
Boughton, M., & Halliday, L. (2009). Home alone: patient and carer uncertainty surrounding discharge with continuing clinical care needs. Contemporary Nurse, 33(1), 30–40.
Mitchell, A. P., Hirsch, B. R., & Abernethy, A. P. (2014). Lack of timely accrual information in oncology clinical trials: A cross-sectional analysis. Trials, 15, 92. https://doi.org/10.1186/1745-6215-15-92.
Giacopuzzi, S., Weindelmayer, J., Treppiedi, E., Bencivenga, M., Ceola, M., Priolo, S., et al. (2017). Enhanced recovery after surgery protocol in patients undergoing esophagectomy for cancer: A single center experience. Diseases of the Esophagus, 30(4), 1–6. https://doi.org/10.1093/dote/dow024.
Pisarska, M., Malczak, P., Major, P., Wysocki, M., Budzynski, A., & Pedziwiatr, M. (2017). Enhanced recovery after surgery protocol in oesophageal cancer surgery: Systematic review and meta-analysis. PLoS ONE, 12(3), e0174382. https://doi.org/10.1371/journal.pone.0174382.
Francis, N. K., Mason, J., Salib, E., Allanby, L., Messenger, D., Allison, A. S., et al. (2015). Factors predicting 30-day readmission after laparoscopic colorectal cancer surgery within an enhanced recovery programme. Colorectal Disease, 17(7), O148–154. https://doi.org/10.1111/codi.13002.
Blazeby, J. M., Soulsby, M., Winstone, K., King, P. M., Bulley, S., & Kennedy, R. H. (2010). A qualitative evaluation of patients' experiences of an enhanced recovery programme for colorectal cancer. Colorectal Disease, 12(10), e236–e242. https://doi.org/10.1111/j.1463-1318.2009.02104.x.
Allvin, R., Ehnfors, M., Rawal, N., & Idvall, E. (2008). Experiences of the postoperative recovery process: an interview study. Open Nursing Journal, 2, 1–7. https://doi.org/10.2174/1874434600802010001.
Bull, J., Oster, C., Flight, I., Wilson, C., Koczwara, B., Watson, D. I., et al. (2019). The role of rehabilitation in patients undergoing oesophagectomy for cancer and pre-malignant disease: A qualitative exploration of the views of patients, carers and healthcare providers. European Journal of Cancer Care (England), 28(2), e12996. https://doi.org/10.1111/ecc.12996.
Kotronoulas, G., Kearney, N., Maguire, R., Harrow, A., Di Domenico, D., Croy, S., et al. (2014). What is the value of the routine use of patient-reported outcome measures toward improvement of patient outcomes, processes of care, and health service outcomes in cancer care? A systematic review of controlled trials. Journal of Clinical Oncology, 32(14), 1480–1501. https://doi.org/10.1200/JCO.2013.53.5948.
Velikova, G. (2004). Use of electronic quality of life applications in cancer research and clinical practice. Expert Review of Pharmacoeconomics & Outcomes Research, 4(4), 403–411. https://doi.org/10.1586/14737167.4.4.403.
van der Meij, E., Anema, J. R., Leclercq, W. K. G., Bongers, M. Y., Consten, E. C. J., Koops, S. E. S., et al. (2018). Personalised perioperative care by e-health after intermediate-grade abdominal surgery: A multicentre, single-blind, randomised, placebo-controlled trial. The Lancet, 392(10141), 51–59. https://doi.org/10.1016/S0140-6736(18)31113-9.
Andikyan, V., Rezk, Y., Einstein, M. H., Gualtiere, G., Leitao, M. M., Jr., Sonoda, Y., et al. (2012). A prospective study of the feasibility and acceptability of a web-based, electronic patient-reported outcome system in assessing patient recovery after major gynecologic cancer surgery. Gynecologic Oncology, 127(2), 273–277. https://doi.org/10.1016/j.ygyno.2012.07.124.
Basch, E., Deal, A. M., Kris, M. G., Scher, H. I., Hudis, C. A., Sabbatini, P., et al. (2016). Symptom monitoring with patient-reported outcomes during routine cancer treatment: A randomized controlled trial. Journal of Clinical Oncology, 34(6), 557–565. https://doi.org/10.1200/JCO.2015.63.0830.
Avery, K. N. L., Richards, H. S., Portal, A., Reed, T., Harding, R., Carter, R., et al. (2019). Developing a real-time electronic symptom monitoring system for patients after discharge following cancer-related surgery. BMC Cancer, 19(1), 463. https://doi.org/10.1186/s12885-019-5657-6.
Holch, P., Pini, S., Henry, A. M., Davidson, S., Routledge, J., Brown, J., et al. (2018). eRAPID electronic patient self-reporting of adverse-events: Patient Information and aDvice: a pilot study protocol in pelvic radiotherapy. Pilot and Feasibility Studies, 4, 110. https://doi.org/10.1186/s40814-018-0304-6.
Holch, P., Warrington, L., Bamforth, L. C. A., Keding, A., Ziegler, L. E., Absolom, K., et al. (2017). Development of an integrated electronic platform for patient self-report and management of adverse events during cancer treatment. Annals of Oncology, 28(9), 2305–2311. https://doi.org/10.1093/annonc/mdx317.
Richards, H. S., Blazeby, J. M., Portal, A., Harding, R., Reed, T., Lander, T., Chalmers, K. A., Carter, R., Singhal, R., Absolom, K., Velikova, G. & Avery, K. N. L. (2019) A real-time electronic symptom monitoring system for patients after discharge following surgery: a pilot study in cancer-related surgery. BMC Cancer. (In Press).
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. https://doi.org/10.1191/1478088706qp063oa.
Braun, V., & Clarke, V. (2014). What can “thematic analysis” offer health and wellbeing researchers? International Journal of Qualitative Studies on Health and Well-Being, 9, 26152. https://doi.org/10.3402/qhw.v9.26152.
Bourgeault, I., Dingwall, R., & De Vrices, R. (2010). The SAGE handbook of qualitative methods in health research. London: SAGE.
Green, J. T., & N., (2004). Qualitative methods for health research. London: Sage.
Warrington, L., Holch, P., Kenyon, L., Hector, C., Kozlowska, K., Kenny, A. M., et al. (2016). An audit of acute oncology services: Patient experiences of admission procedures and staff utilisation of a new telephone triage system. Supportive Care in Cancer, 24(12), 5041–5048. https://doi.org/10.1007/s00520-016-3370-4.
Khuri, S. F., Henderson, W. G., DePalma, R. G., Mosca, C., Healey, N. A., Kumbhani, D. J., et al. (2005). Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. The Annals of Surgery, 242(3), 326–341; discussion 341–323.
Warrington, L., Absolom, K., Holch, P., Gibson, A., Clayton, B., & Velikova, G. (2019). Online tool for monitoring adverse events in patients with cancer during treatment (eRAPID): Field testing in a clinical setting. British Medical Journal Open, 9(1), e025185. https://doi.org/10.1136/bmjopen-2018-025185.
Driscoll, A. (2000). Managing post-discharge care at home: an analysis of patients’ and their carers’ perceptions of information received during their stay in hospital. Journal of Advanced Nursing, 31(5), 1165–1173. https://doi.org/10.1046/j.1365-2648.2000.01372.x.
Malmstrom, M., Ivarsson, B., Johansson, J., & Klefsgard, R. (2013). Long-term experiences after oesophagectomy/gastrectomy for cancer—a focus group study. International Journal of Nursing Studies, 50(1), 44–52. https://doi.org/10.1016/j.ijnurstu.2012.08.011.
den Bakker, C. M., Schaafsma, F. G., van der Meij, E., Meijerink, W. J., van den Heuvel, B., Baan, A. H., et al. (2019). Electronic health program to empower patients in returning to normal activities after general surgical and gynecological procedures: Intervention mapping as a useful method for further development. Journal of Medical Internet Research, 21(2), e9938. https://doi.org/10.2196/jmir.9938.
Godwin, Y. (2000). Do they listen? A review of information retained by patients following consent for reduction mammoplasty. British Journal of Plastic Surgery, 53(2), 121–125. https://doi.org/10.1054/bjps.1999.3220.
Kessels, R. P. (2003). Patients' memory for medical information. Journal of the Royal Society of Medicine, 96(5), 219–222. https://doi.org/10.1258/jrsm.96.5.219.
Pieper, B., Sieggreen, M., Nordstrom, C. K., Freeland, B., Kulwicki, P., Frattaroli, M., et al. (2007). Discharge knowledge and concerns of patients going home with a wound. Journal of Wound, Ostomy and Continence Nursing, 34(3), 245–253; quiz 254–245. https://doi.org/10.1097/01.WON.0000270817.06942.00.
Watson, P. W., & McKinstry, B. (2009). A systematic review of interventions to improve recall of medical advice in healthcare consultations. Journal of the Royal Society of Medicine, 102(6), 235–243. https://doi.org/10.1258/jrsm.2009.090013.
Weinhouse, G. L., Schwab, R. J., Watson, P. L., Patil, N., Vaccaro, B., Pandharipande, P., et al. (2009). Bench-to-bedside review: Delirium in ICU patients—importance of sleep deprivation. Critical Care, 13(6), 234. https://doi.org/10.1186/cc8131.
Cook, D. J., Moradkhani, A., Douglas, K. S., Prinsen, S. K., Fischer, E. N., & Schroeder, D. R. (2014). Patient education self-management during surgical recovery: Combining mobile (iPad) and a content management system. Telemedicine and e-Health, 20(4), 312–317. https://doi.org/10.1089/tmj.2013.0219.
Lee, B. T., Chen, C., Yueh, J. H., Nguyen, M. D., Lin, S. J., & Tobias, A. M. (2010). Computer-based learning module increases shared decision making in breast reconstruction. Annals of Surgical Oncology, 17(3), 738–743. https://doi.org/10.1245/s10434-009-0869-7.
Fredericks, S., Guruge, S., Sidani, S., & Wan, T. (2010). Postoperative patient education: A systematic review. Clinical Nursing Research, 19(2), 144–164. https://doi.org/10.1177/1054773810365994.
Barello, S., Triberti, S., Graffigna, G., Libreri, C., Serino, S., Hibbard, J., et al. (2015). eHealth for patient engagement: A systematic review. Frontiers in Psychology, 6, 2013. https://doi.org/10.3389/fpsyg.2015.02013.
Acknowledgements
The authors would like to thank all the patients who took part in this study, and the members of the Surgical Research Nurse teams, Cancer Nurse Specialist teams and Dietitian team at University Hospital Bristol NHS Foundation Trust.
Funding
This report is independent research funded by the National Institute for Health Research (Programme Grants for Applied Health research, Towards safer delivery and monitoring of cancer treatments. Electronic patient self-Reporting of Adverse events: Patient Information and aDvice (eRAPID) RP-PG-0611-20008). This work was undertaken with the support of the Medical Research Council ConDuCT-II (Collaboration and innovation for Difficult and Complex randomised controlled Trials In Invasive procedures) Hub for Trials Methodology Research (MR/K025643/1) (https://www.bristol.ac.uk/social-community-medicine/centres /conduct2/), Royal College of Surgeons of England Bristol Surgical Trials Centre and National Institute for Health Research (NIHR) Biomedical Research Centre (BRC) at the University Hospitals Bristol NHS Foundation Trust and the University of Bristol. JMB holds an NIHR Senior Investigator award. The views expressed in this publication are those of the author(s) and not necessarily those of the National Institute for Health Research, Department of Health and Social Care or MRC.
Author information
Authors and Affiliations
Contributions
JB and GV conceived the study. KA, JB, HR and GV designed the study; HR conducted day-to-day management of the study; KA, JB and GV oversaw the study; AP and HR collected data and carried out data analyses; KA and HR interpreted data and drafted the manuscript; all authors critically reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethics approval
All procedures performed in studies participants were in accordance with the ethical standards of the institutional and/or national research committee (London Surrey Borders Research Ethics Committee 15/LO/2017) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study, including consent for audio recording of interviews and telephone consultations.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Richards, H.S., Portal, A., Absolom, K. et al. Patient experiences of an electronic PRO tailored feedback system for symptom management following upper gastrointestinal cancer surgery. Qual Life Res 30, 3229–3239 (2021). https://doi.org/10.1007/s11136-020-02539-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02539-w