Abstract
Purpose
To identify HIV clinicians’ needs for the clinical use of a new patient-reported outcome measure (PRO) on barriers to antiretroviral therapy (ART) adherence.
Methods
In 2015, five focus groups with 31 clinicians from France were transcribed, coded with Atlas.ti, and submitted to a typological analysis.
Results
The analysis identified seven patient profiles, each tied to distinct barriers to adherence and to specific needs for the PRO’s content, data collection and transmission. Clinicians preferred, for the patient who is: (1) ‘passive,’ that the PRO collect information on ART knowledge, to ensure that the prescription’s instructions are being respected; (2) ‘misleading,’ that it be able to detect adherence to ART and socially desirable responses; (3) ‘stoic,’ that questions challenge the patient to recognize treatment-specific side effects; (4) ‘hedonistic,’ that the PRO contains content on lifestyle and risk-taking; (5) ‘obsessive,’ that the PRO captures quality of life and stressful life events; (6) ‘overburdened,’ that the PRO provides information on the person’s home environment, socioeconomic status and cultural constraints. For all or most patient profiles, the clinicians wished that the PRO be completed, minimally, prior to the medical consultation and to receive alerts, under varying conditions, when problematic scores were detected. Depending on the profile, there was preference for the inclusion of open-ended questions and transmission of cross-sectional, periodic or longitudinal PRO data.
Conclusion
Overall, this study’s findings suggest that to support the clinical management of ART adherence, our PRO must meet the needs of a wide variety of patients and must perform multiple functions.
Similar content being viewed by others
References
Ammassari, A., Trotta, M. P., Shalev, N., Marconi, P., & Antinori, A. (2012). Beyond virological suppression: The role of adherence in the late HAART era. Antiviral Therapy, 17(5), 785–792. doi:10.3851/IMP2084.
Lima, V. D., Harrigan, R., Bangsberg, D. R., Hogg, R. S., Gross, R., Yip, B., et al. (2009). The combined effect of modern highly active antiretroviral therapy regimens and adherence on mortality over time. Journal of Acquired Immune Deficiency Syndromes, 50(5), 529–536. doi:10.1097/QAI.0b013e31819675e9.
Laws, M., Beach, M. C., & Lee, Y. (2012). Provider-patient adherence dialogue in HIV care: results of a multisite study. AIDS and Behavior, 17(1), 148–159.
Robert, K. (2000). Physician beliefs about antiretroviral adherence communication. AIDS Patient Care and STDs, 14(9), 477–484.
Katz, I. T., Ryu, A. E., Onuegbu, A. G., Psaros, C., Weiser, S. D., Bangsberg, D. R., et al. (2013). Impact of HIV-related stigma on treatment adherence: Systematic review and meta-synthesis. Journal of the International AIDS Society, 16(3 Suppl 2), 18640. doi:10.7448/IAS.16.3.18640.
Bolsewicz, K., Debattista, J., Vallely, A., Whittaker, A., & Fitzgerald, L. (2015). Factors associated with antiretroviral treatment uptake and adherence: a review. Perspectives from Australia, Canada, and the United Kingdom. AIDS Care, 27(12), 1429–1438. doi:10.1080/09540121.2015.1114992.
Kozak, M. S., Mugavero, M. J., Ye, J., Aban, I., Lawrence, S. T., Nevin, C. R., et al. (2012). Patient reported outcomes in routine care: advancing data capture for HIV cohort research. Clinical Infectious Diseases, 54(1), 141–147. doi:10.1093/cid/cir727.
Simpson, K. N., Hanson, K. A., Harding, G., Haider, S., Tawadrous, M., Khachatryan, A., et al. (2013). Patient reported outcome instruments used in clinical trials of HIV-infected adults on NNRTI-based therapy: a 10-year review. Health and Quality of Life Outcomes, 11, 164. doi:10.1186/1477-7525-11-164.
Engler, K., Lessard, D., & Lebouche, B. (2017). A review of HIV-specific patient-reported outcome measures. Patient, 10(2), 187–202. doi:10.1007/s40271-016-0195-7.
de Wit, M. P., Kvien, T. K., & Gossec, L. (2015). Patient participation as an integral part of patient-reported outcomes development ensures the representation of the patient voice: a case study from the field of rheumatology. RMD Open, 1(1), e000129. doi:10.1136/rmdopen-2015-000129.
Hagell, P., Reimer, J., & Nyberg, P. (2009). Whose quality of life? Ethical implications in patient-reported health outcome measurement. Value in Health, 12(4), 613–617. doi:10.1111/j.1524-4733.2008.00488.x.
Kwan, B. M., Sills, M. R., Graham, D., Hamer, M. K., Fairclough, D. L., Hammermeister, K. E., et al. (2016). Stakeholder engagement in a patient-reported outcomes (pro) measure implementation: A report from the SAFTINet practice-based research network (PBRN). Journal of The American Board of Family Medicine, 29(1), 102–115. doi:10.3122/jabfm.2016.01.150141.
Valderas, J. M., Kotzeva, A., Espallargues, M., Guyatt, G., Ferrans, C. E., Halyard, M. Y., et al. (2008). The impact of measuring patient-reported outcomes in clinical practice: a systematic review of the literature. Quality of Life Research : An International Journal of Quality of Life Aspects of Treatment, Care And Rehabilitation, 17(2), 179–193.
Batty, M. J., Moldavsky, M., Foroushani, P. S., Pass, S., Marriott, M., Sayal, K., et al. (2013). Implementing routine outcome measures in child and adolescent mental health services: from present to future practice. Child and Adolescent Mental Health, 18(2), 82–87.
Greenhalgh, J. (2009). The applications of PROs in clinical practice: what are they, do they work, and why? Quality of Life Research, 18(1), 115–123. doi:10.1007/s11136-008-9430-6.
Boyce, M. B., Browne, J. P., & Greenhalgh, J. (2014). The experiences of professionals with using information from patient-reported outcome measures to improve the quality of healthcare: a systematic review of qualitative research. BMJ Quality & Safety, 23, 508–518.
Engler, K., Lessard, D., Toupin, I., Lènàrt, A., & Lebouché, B. (2017). Engaging stakeholders into an electronic patient-reported outcome development study: on making an HIV-specific e-PRO patient-centered. Health Policy and Technology, 6(1), 59–66.
Toupin, I., Engler, K., Lessard, D., Wong, L., Lènàrt, A., Raffi, F., et al. (2016). Developing a patient reported outcome measure (PRO) for HIV care on perceived barriers to antiretroviral adherence: Assessing the needs of HIV clinicians through typological analysis. Paper presented at the Poster presented at HIV Drug Therapy, Glasgow.
Toupin, I., Engler, K., Lessard, D., Wong, L., Lènàrt, A., Raffi, F., et al. (2017). Patient profiles as organizing HIV clinicians’ ART adherence management: a qualitative analysis. AIDS Care. doi:10.1080/09540121.2017.1360995.
Van der Maren, J. M. (2006). Méthodes de recherche pour l’éducation (2ed.). Montreal: Presses de l’Université de Montréal et de Boeck.
Marchand, J., & Giroux, C. (2010). L’utilisation des groupes de discussion en marketing commercial et social. Recheches Qualitatives, 29(1), 99–109.
Kitzinger, J. (1995). Qualitative research. Introducing focus groups. BMJ (Clinical Research ed.), 311(7000), 299–302.
Engler, K., Lènàrt, A., Lessard, D., Toupin, I., & Lebouché, B. (2017). A synthesis of qualitative research with adults living with HIV on barriers to ART adherence (Abstract #118). Paper presented at the 12th International Conference on HIV Treatment and Prevention Adherence, Miami, USA, June 4–6.
Poupart, J. (1997). L’entretien de type qualitatif: considérations épistémologiques, théoriques et méthodologiques. In J. Poupart, L.-H. Deslauriers, J.-P. Groulx, A. Laperrière, R. Mayer & A. P. Pires (Eds.), La recherche qualitative. Enjeux épistémologiques et méthodologiques. Montréal: Gaëtan Morin.
Baribeau, C. (2009). Analyse des données des entretiens de groupe. Recheches Qualitatives, 28(1), 133–148.
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101.
Charmaz, K. (2000). Grounded theory: Objectivist and constructivist methods. In N. K. Denzin & Y. S. Lincoln (Eds.), Handbook of qualitative research (2 ed., pp. 509–535). Californie: Sage Publications.
Schnapper, D. (2005). La compréhension sociologique. Démarche de l’analyse typologique. Paris: Presses de l’Université de France.
Harding, R., Liu, L., Catalan, J., & Sherr, L. (2011). What is the evidence for effectiveness of interventions to enhance coping among people living with HIV disease? A systematic review. Psychology Health and Medicine, 16(5), 564–587.
Mulkins, A. L., Ibanez-Carrasco, F., Boyack, D., & Verhoef, M. J. (2014). The Living Well Lab: A community-based HIV/AIDS research initiative. Journal of Complementary and Integrative Medicine, 11(3), 213–222. doi:10.1515/jcim-2013-0057.
Panel on Antiretroviral Guidelines for Adults and Adolescents (2016). Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. In Health & Human Services (Eds.), (pp. 1–139).
Mosack, K. E., & Wendorf, A. R. (2011). Health care provider perspectives on informal supporters’ involvement in HIV care. Qualitative Health Research, 21(11), 1554–1566. doi:10.1177/1049732311413783.
Orchard, T., Salters, K., Palmer, A., Michelow, W., Lepik, K. J., & Hogg, R. (2015). Vets, denialists and rememberers: Social typologies of patient adherence and non-adherence to HAART from the perspective of HIV care providers. AIDS Care, 27(6), 758–761. doi:10.1080/09540121.2015.1005003.
Bogart, L. M., Catz, S. L., Kelly, J. A., & Benotsch, E. G. (2001). Factors influencing physicians’ judgments of adherence and treatment decisions for patients with HIV disease. Medical Decision Making: An International Journal of the Society for Medical Decision Making, 21(1), 28–36.
Phillips, L. A., Leventhal, E. A., & Leventhal, H. (2011). Factors associated with the accuracy of physicians’ predictions of patient adherence. Patient Education and Counseling, 85(3), 461–467. doi:10.1016/j.pec.2011.03.012.
Chesney, M. A. (2000). Factors affecting adherence to antiretroviral therapy. Clinical Infectious Diseases, 30 (Suppl 2), 171–176. doi:10.1086/313849.
Langebeek, N., Gisolf, E. H., Reiss, P., Vervoort, S. C., Hafsteinsdottir, T. B., Richter, C., et al. (2014). Predictors and correlates of adherence to combination antiretroviral therapy (ART) for chronic HIV infection: a meta-analysis. BMC Medicine, 12, 142. doi:10.1186/PREACCEPT-1453408941291432.
O’Connor, J. L., Gardner, E. M., Mannheimer, S. B., Lifson, A. R., Esser, S., Telzak, E. E., et al. (2013). Factors associated with adherence amongst 5295 people receiving antiretroviral therapy as part of an international trial. Journal of Infectious Diseases, 208(1), 40–49. doi:10.1093/infdis/jis731.
Marewski, J. N., & Gigerenzer, G. (2012). Heuristic decision making in medicine. Dialogues in Clinical Neuroscience, 14(1), 77–89.
Blair, I. V., Steiner, J. F., & Havranek, E. P. (2011). Unconscious (implicit) bias and health disparities: Where do we go from here? The Permanente Journal, 15(2), 71–78.
Jacoby, A. (1994). Felt versus enacted stigma: a concept revisited. evidence from a study of people with epilepsy in remission. Social Science & Medicine, 38(2), 269–274.
Phelan, S. M., Burgess, D. J., Yeazel, M. W., Hellerstedt, W. L., Griffin, J. M., & van Ryn, M. (2015). Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obesity Reviews : An Official Journal of The International Association for the Study of Obesity International Association for the Study of Obesity, 16(4), 319–326. doi:10.1111/obr.12266.
Barfod, T. S., Hecht, F. M., Rubow, C., & Gerstoft, J. (2006). Physicians communication with patients about adherence to HIV medication in San Francisco and Copenhagen: a qualitative study using Grounded Theory. BMC Health Services Research, 6, 154. doi:10.1186/1472-6963-6-154.
Poppa, A., Davidson, O., Deutsch, J., Godfrey, D., Fisher, M., Head, S., et al. (2004). British HIV Association (BHIVA)/British Association for Sexual Health and HIV (BASHH) guidelines on provision of adherence support to individuals receiving antiretroviral therapy (2003). HIV Medicine, 5(Suppl 2), 46–60. doi:10.1111/j.1468-1293.2004.00215.x.
McKenna, S. P. (2011). Measuring patient-reported outcomes: Moving beyond misplaced common sense to hard science. BMC Medicine, 9, 86. doi:10.1186/1741-7015-9-86.
Meadows, K. A. (2003). So you want to do research? 5: Questionnaire design. British Journal of Community Nursing, 8(12), 562–570. doi:10.12968/bjcn.2003.8.12.11854.
Lagu, T., Goff, S. L., Hannon, N. S., Shatz, A., & Lindenauer, P. K. (2013). A mixed-methods analysis of patient reviews of hospital care in England: implications for public reporting of health care quality data in the United States. The Joint Commission Journal on Quality and Patient Safety, 39(1), 7–15.
Kyte, D., Ives, J., Draper, H., & Calvert, M. (2016). Management of patient-reported outcome (PRO) alerts in clinical trials: A cross sectional survey. PLoS ONE, 11(1), e0144658. doi:10.1371/journal.pone.0144658.
Kyte, D., Draper, H., & Calvert, M. (2013). Patient-reported outcome alerts: Ethical and logistical considerations in clinical trials. JAMA: The Journal of The American Medical Association, 310(12), 1229–1230. doi:10.1001/jama.2013.277222.
Fowler, F. J. (1996). Jr. Data collection methods. In B. Spilker (Ed.), Quality of Life and Pharmacoeconomics in Clinical Trials (2 ed.). Philadelphia: Lippincott-Raven.
Naughton, M. J., Shumaker, S. A., Anderson, R. T., & Czajkowski, S. M. (1996). Psychological aspects of health-related quality of life measurement: tests and scales. In B. Spilker (Ed.), Quality of life and pharmacoeconomics in clinical trials (2 ed.). Philadelphia: Lippincott-Raven.
Van Vliet, L. M., Harding, R., Bausewein, C., Payne, S., Higginson, I. J., & EUROIMPACT (2015). How should we manage information needs, family anxiety, depression and breathlessness for those affected by advanced disease: development of a clinical decision support tool using a Delphi design. BMC Medicine, 13, 263. doi:10.1186/s12916-015-0449-6.
Snyder, C. F., Jensen, R., Courtin, S. O., & Wu, A. W. & Website for Outpatient, Q. O. L. A. R. N. (2009). Patient viewpoint: a website for patient-reported outcomes assessment. Quality of Life Research, 18(7), 793–800. doi:10.1007/s11136-009-9497-8.
Aaronson, N. K., Elliott, T. E., Greenhalgh, J., Halyard, M. Y., Hess, R., Miller, D. M., et al. (2015) User’s guide to implementing patient-reported outcomes assessment in clinical practice. International Society for Quality of Life Research, Version.
Fredericksen, R. J., Tufano, J., Ralston, J., McReynolds, J., Stewart, M., Lober, W. B., et al. (2016). Provider perceptions of the value of same-day, electronic patient-reported measures for use in clinical HIV care. AIDS Care, 28(11), 1428–1433. doi:10.1080/09540121.2016.1189501.
Segal, C., Holve, E., & Sabharwal, R. (2013). Collecting and using patient-reported outcomes (pro) for comparative effectiveness research (CER) and patient-centered outcomes research (pcor): Challenges and opportunities. Issue Briefs and Reports. Paper 10.
Pourtois, J. & Desmet, H. (1997). Épistemologie et instumentation en sciences humaines (2nd ed.). Sprimont: Margada Editeur.
Acknowledgements
We would like to thank the participants of this study for their valuable input. We also thank Chantal Burelle for her administrative support and Roy Nitulescu for his feedback on the manuscript’s results.
Funding
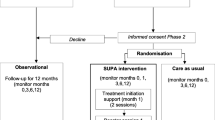
IT, DL and AL are the recipients of a Mitacs Accelerate Postdoctoral Internship award (#05857). BL is supported by a Research Scholar award of the FRQS (Quebec Health Research Funds) and holds a Strategy for Patient-Oriented Research (SPOR) Mentorship Chair in Innovative Clinical Trials awarded by the Canadian Institutes of Health Research (http://www.cihr-irsc.gc.ca; CIHR: #383427). This study was conducted as a part of a larger study (The I-Score Study, clinicaltrials.gov identifier: NCT02586584) which is supported in part by both the CIHR’s HIV Clinical Trials Network (CTN 283) and by a research Grant from the Investigator Initiated Studies Program of Merck Canada Inc. (IISP-53538).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Disclosure
The opinions expressed in this manuscript are those of the authors and do not necessarily represent those of Merck Canada Inc. or its affiliates or related companies.
Ethical approval
Ethical approval was granted by the Biomedical Research Ethics Board of the McGill University Health Centre (Study Code 14-229-PSY).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Toupin, I., Engler, K., Lessard, D. et al. Developing a patient-reported outcome measure for HIV care on perceived barriers to antiretroviral adherence: assessing the needs of HIV clinicians through qualitative analysis. Qual Life Res 27, 379–388 (2018). https://doi.org/10.1007/s11136-017-1711-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-017-1711-5