Abstract
Purpose
For people with schizophrenia living in the community and receiving outpatient care, the issues of stigma and discrimination and dearth of recovery-oriented services remain barriers to recovery and community integration. The experience of self-stigma and unmet recovery needs can occur regardless of symptom status or disease process, reducing life satisfaction and disrupting overall well-being. The present study examined the mediating role of self-stigma and unmet needs in the relationship between psychiatric symptom severity and subjective quality of life.
Methods
Structural equation modeling and mediation analyses were conducted based on a community sample of 400 mental health consumers with schizophrenia spectrum disorders in Hong Kong.
Results
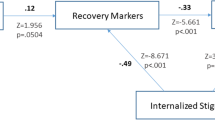
The model of self-stigma and unmet needs as mediators between symptom severity and subjective quality of life had good fit to the data (GFI = .93, CFI = .93, NNFI = .92, RMSEA = .06, χ2/df ratio = 2.62). A higher level of symptom severity was significantly associated with increased self-stigma (R 2 = .24) and a greater number of unmet needs (R 2 = .53). Self-stigma and unmet needs were in turn negatively related to subjective quality of life (R 2 = .45).
Conclusions
It is essential that service providers and administrators make greater efforts to eliminate or reduce self-stigma and unmet recovery needs, which are associated with the betterment of the overall quality of life and long-term recovery. Both incorporating empowerment and advocacy-based interventions into recovery-oriented services and providing community-based, person-centered services to people based on personally defined needs are important directions for future recovery-oriented efforts.

Similar content being viewed by others
References
Silverstein, S. M., & Bellack, A. S. (2008). Scientific agenda for the concept of recovery as it applies to schizophrenia. Clinical Psychology Review, 28, 1108–1124.
Tse, S., Siu, B. W., & Kan, A. (2013). Can recovery-oriented mental health services be created in Hong Kong? Struggles and strategies. Administration and Policy In Mental Health, 40, 155–158.
Substance Abuse and Mental Health Services Administration. (2005). National consensus conference on mental health recovery and systems transformation. Rockville, MD: Department of Health and Human Services, United States Government.
New Freedom Commission on Mental Health. (2003). Achieving the promise: Transforming mental health care in America. Final Report. Rockville, MD: Department of Health and Human Services. Publication SMA-03-3832.
Onken, S. J., Craig, C. M., Ridgway, P., Ralph, R. O., & Cook, J. A. (2007). An analysis of the definitions and elements of recovery: A review of the literature. Psychiatric Rehabilitation Journal, 31, 9–22.
Lloyd, C., King, R., & Moore, L. (2010). Subjective and objective indicators of recovery in severe mental illness: A cross-sectional study. International Journal of Social Psychiatry, 56, 220–229.
Crisp, A. H., Gelder, M. G., Rix, S., Meltzer, H. I., & Rowlands, O. J. (2000). Stigmatisation of people with mental illnesses. British Journal of Psychiatry, 177, 4–7.
World Health Organization. (2008). The global burden of disease: 2004 update. Geneva: World Health Organization.
Mak, W. W. S., Poon, C. Y. M., Pun, L. Y. K., & Cheung, S. F. (2007). Meta-analysis of stigma and mental health. Social Science and Medicine, 65, 245–261.
Wu, C. F. M., Mak, W. W. S., & Wan, D. L. Y. (2007). Quality of life of mental health consumers in Hong Kong: Analysis of service perceptions. Quality of Life Research, 16, 31–40.
Lam, M. M., Pearson, V., Ng, R. M., Chiu, C. P., Law, C. W., & Chen, E. Y. (2011). What does recovery from psychosis mean? Perceptions of young first-episode patients. International Journal of Social Psychiatry, 57, 580–587.
Ng, R. M., Pearson, V., Chen, E. E., & Law, C. W. (2011). What does recovery from schizophrenia mean? Perceptions of medical students and trainee psychiatrists. International Journal of Social Psychiatry, 57, 248–262.
Ng, R. M., Pearson, V., Lam, M., Law, C. W., Chiu, C. P., & Chen, E. Y. (2008). What does recovery from schizophrenia mean? Perceptions of long-term patients. International Journal of Social Psychiatry, 54, 118–130.
Mak, W., Lam, B., & Yan, S. (2010). Recovery knowledge and recovery-oriented services in Hong Kong. Psychiatric Services, 61, 1164.
Mak, W. W. S., Chong, E. S. K., & Wong, C. C. Y. (2014). Beyond attributions—Understanding public stigma of mental illness with the common sense model. American Journal of Orthopsychiatry, 84, 173–181.
Lee, S., Lee, M. T. Y., Chiu, M. Y. L., & Kleinman, A. (2005). Experience of social stigma by people with schizophrenia in Hong Kong. British Journal of Psychiatry, 186, 153–157.
Tsang, H. W. H., Angell, B., Corrigan, P. W., Lee, Y.-T., Shi, K., Lam, C. S., et al. (2007). A cross-cultural study of employers’ concerns about hiring people with psychotic disorder: Implications for recovery. Social Psychiatry and Psychiatric Epidemiology, 42, 723–733.
Tsang, H. W. H., Tam, P. K. C., Chan, F., & Cheung, W. M. (2003). Stigmatizing attitudes towards individuals with mental illness in Hong Kong: Implications for their recovery. Journal of Community Psychology, 31, 383–396.
Corrigan, P. W., & Watson, A. C. (2002). The paradox of self-stigma and mental illness. Clinical Psychology: Science and Practice, 9, 35–53.
Mak, W. W. S., & Cheung, R. Y. M. (2010). Self-stigma among concealable minorities in Hong Kong: Conceptualization and unified measurement. American Journal of Orthopsychiatry, 80, 263–277.
Lysaker, P. H., Roe, D., & Yanos, P. T. (2007). Toward understanding the insight paradox: Internalized stigma moderates the association between insight and social functioning, hope, and self-esteem among people with schizophrenia spectrum disorders. Schizophrenia Bulletin, 33, 192–199.
Ritsher, J. B., Otilingam, P. G., & Grajales, M. (2003). Internalized stigma of mental illness: Psychometric properties of a new measure. Psychiatry Research, 121, 31–49.
Vauth, R., Kleim, B., Wirtz, M., & Corrigan, P. (2007). Self-efficacy and empowerment as outcomes of self-stigmatizing and coping schizophrenia. Psychiatry Research, 150, 71–80.
Yanos, P. T., Roe, D., Markus, K., & Lysaker, P. H. (2008). Pathways between internalised stigma and outcomes related to recovery in schizophrenia spectrum disorders. Psychiatric Services, 59, 1437–1442.
Gunnmo, P., & Fatouros Bergman, H. (2011). What do individuals with schizophrenia need to increase their well-being. International Journal of Qualitative Studies on Health and Well-Being, 6, 5412.
Minnes, P., Carlson, P., McColl, M. A., Nolte, M. L., Johnston, J., & Buell, K. (2003). Community integration: A useful construct, but what does it really mean? Brain Injury, 17, 149–159.
Hansson, L., Sandlund, M., Bengtsson-Tops, A., Bjarnason, O., Karlsson, H., Mackeprang, T., et al. (2003). The relationship of needs and quality of life in persons with schizophrenia living in the community. A Nordic multi-center study. Nordic Journal of Psychiatry, 57, 5–11.
Grinshpoon, A., & Ponizovsky, A. M. (2008). The relationships between need profiles, clinical symptoms, functioning and the well-being of inpatients with severe mental disorders. Journal of Evaluation in Clinical Practice, 14, 218–225.
Chiu, M. Y., Ho, W. W., Lo, W. T., & Yiu, M. G. (2010). Operationalization of the SAMHSA model of recovery: A quality of life perspective. Quality of Life Research, 19, 1–13.
Davidson, L., & Roe, D. (2007). Recovery from versus recovery in serious mental illness: One strategy for lessening the confusion plaguing recovery. Journal of Mental Health, 16, 459–470.
Roe, D., Mashiach-Eizenberg, M., & Lysaker, P. H. (2011). The relation between objective and subjective domains of recovery among persons with schizophrenia-related disorders. Schizophrenia Research, 131, 133–138.
Lambert, M., Naber, D., Eich, F. X., Schacht, M., Linden, M., & Schimmelmann, B. G. (2007). Remission of severely impaired subjective wellbeing in 727 patients with schizophrenia treated with amisulpride. Acta Psychiatrica Scandinavica, 115, 106–113.
Lieberman, J. A., Drake, R. E., Sederer, L. I., Belger, A., Keefe, R., Perkins, D., et al. (2008). Science and recovery in schizophrenia. Psychiatric Services, 59, 487–496.
Angermeyer, M. C., & Kilian, R. (1997). Theoretical models of quality of life for mental disorders. In N. Sartorius (Ed.), Quality of life in mental disorders (pp. 19–30). Chichester: Wiley.
Lambert, M., Schimmelmann, B. G., Schacht, A., Karow, A., Wagner, T., Wehmeier, P. M., et al. (2009). Long-term patterns of subjective wellbeing in schizophrenia: Cluster, predictors of cluster affiliation, and their relation to recovery criteria in 2842 patients followed over 3 years. Schizophrenia Research, 107, 165–172.
Test, M. A., Greenberg, J. S., Long, J. D., Brekke, J. S., & Burke, S. S. (2005). The construct validity of a measure of subjective satisfaction with life of adults with serious mental illness. Psychiatric Services, 56, 292–300.
Priebe, S., & Fakhoury, W. (2008). Quality of life. In K. Mueser & D. Jeste (Eds.), The clinical handbook of schizophrenia. New York: Guilford.
Andresen, R., Caputi, P., & Oades, L. G. (2010). Do clinical outcome measures assess consumer-defined recovery? Psychiatry Research, 177, 309–317.
Eack, S. M., & Newhill, C. E. (2007). Psychiatric symptoms and quality of life in schizophrenia: A meta-analysis. Schizophrenia Bulletin, 33, 1225–1237.
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders: DSM-IV (4th ed.). Washington, DC: American Psychiatric Association.
Eisen, S. V., Normand, S. L., Belanger, A. J., Spiro, A., & Esch, D. (2004). The revised Behavior and Symptom Identification Scale (BASISR-R): Reliability and validity. Medical Care, 42, 1230–1241.
Phelan, M., Slade, M., Thornicroft, G., Dunn, G., Holloway, F., Wykes, T., et al. (1995). The Camberwell assessment of need: The validity and reliability of an instrument to assess the needs of people with severe mental illness. British Journal of Psychiatry, 167, 589–595.
Chan, K. K. S., & Mak, W. W. S. (2014). The effects of self-stigma content and process on subjective quality of life in people with schizophrenia. Schizophrenia Research, 153 (Suppl 1), S282–S283.
Mak, W. W. S., Pang, I. H. Y., Chung, N. Y. L., Yau, S. S. W., & Tang, J. P. S. (unpublished manuscript). Effectiveness of wellness recovery action planning (WRAP) for Chinese with mental illness in Hong Kong.
Joreskob, K. G., & Sorbom, D. (1981). LISREL V: Analysis of linear structural relationships by the method of maximum likelihood. Chicago: National Educational Resources.
Bentler, P. M. (1990). Comparative fit indices in structural models. Psychological Bulletin, 107, 238–246.
Bentler, P. M., & Bonnett, D. G. (1980). Significance test and goodness of fit in the analysis of covariance structures. Psychological Bulletin, 88, 588–606.
Browne, M. W., & Cudeck, R. (1993). Alternative ways of assessing model fit. In K. A. Bollen & J. S. Long (Eds.), Testing structural equation models (pp. 136–162). Newbury Park, CA: Sage.
Carmines, E. G., & McIver, J. P. (1981). Analyzing models with unobserved variables. In G. M. Bohrnstedt & E. F. Borgatta (Eds.), Social measurement: Current issues (pp. 63–115). Beverly Hills: Sage.
Kline, R. B. (1998). Principles and practice of structural equation modeling. New York: Guilford.
Hoyle, R. H., & Panter, A. T. (1995). Writing about structural equation models. In R. H. Hoyle (Ed.), Structural equation modeling: Concepts, issues, and applications (pp. 158–176). Thousand Oaks, CA: Sage.
Bentler, P. M. (2003). EQS for windows (Version 6.1) [Computer software]. Encino, CA: Multivariate Software.
Lysaker, P. H., Vohs, J. L., & Tsai, J. (2009). Negative symptoms and concordant impairments in attention in schizophrenia: Associations with social functioning, hope, self-esteem and internalized stigma. Schizophrenia Research, 110, 165–172.
Davidson, L. (2003). Living outside mental illness: Qualitative studies of recovery in schizophrenia. New York: New York University Press.
Roe, D., & Ben-Yishai, A. (1999). Exploring the relationship between the person and the disorder among individuals hospitalized for psychosis. Psychiatry, 62, 370–380.
Deegan, P. (1997). Recovery and empowerment for people with psychiatric disabilities. Social Work in Health Care, 25, 11–24.
Copeland, M. E. (2002). Wellness Recovery Action Plan: A system for monitoring, reducing and eliminating uncomfortable or dangerous physical symptoms and emotional feelings. Occupational Therapy in Mental Health, 17, 127–150.
Hogan, M. F. (2003). New freedom commission report: The President’s new freedom commission: Recommendations to transform mental health care in America. Psychiatric Services, 54, 1467–1474.
Ritsher, J. B., & Phelan, J. C. (2004). Internalized stigma predicts erosion of morale among psychiatric outpatients. Psychiatry Research, 129, 257–265.
Holzinger, A., Dietrich, S., Heitmann, S., & Angermeyer, M. C. (2008). Evaluation zielgruppenorientierter Interventionen zur Reduzierung des Stigmas psychischer Krankheit. Eine systematische Ubersicht [Evaluation of target-group oriented interventions aimed at reducing the stigma surrounding mental illness. A systematic review]. Psychiatrische Praxis, 35, 376–386.
Hayes, S. C., Strosahl, K. D., & Wlison, K. G. (1999). Acceptance and commitment therapy: An experiential approach to behavior change. New York: Guilford Press.
Luoma, J. B., Kohlenberg, B. S., Hayes, S. C., Bunting, K., & Rye, A. K. (2008). Reducing self-stigma in substance abuse through acceptance and commitment therapy: Model, manual development, and pilot outcomes. Addiction Research & Theory, 16, 149–165.
Chan, K. K. S., & Mak, W. W. S. (2012). Shared decision making in the recovery of people with schizophrenia: The role of metacognitive capacities in insight and pragmatic language use. Clinical Psychology Review, 32, 535–544.
Jacobson, N., & Greenley, D. (2001). What is recovery? A conceptual model and explication. Psychiatric Services, 52, 482–485.
Racenstein, J. M., Harrow, M., Reed, R., Martin, E., Herbener, E., & Penn, D. L. (2002). The relationship between positive symptoms and instrumental work functioning in schizophrenia: A 10-year follow-up study. Schizophrenia Research, 56, 95–103.
McCrone, P., Leese, M., Thornicroft, G., Schene, A., Knudsen, H. C., Vazquez-Barquero, J. L., et al. (2001). A comparison of needs of patients with schizophrenia in five European countries: The EPSILON Study. Acta Psychiatrica Scandinavica, 103, 370–379.
Middelboe, T., Mackeprang, T., Hansson, L., Werdelin, G., Karlsson, H., Bjarnason, O., et al. (2001). The Nordic Study on schizophrenic patients living in the community. Subjective needs and perceived help. European Psychiatry, 16, 207–214.
Lasalvia, A., Bonetto, C., Malchiodi, F., Salvi, G., Parabiaghi, A., Tansella, M., et al. (2005). Listening to patients’ needs to improve their subjective quality of life. Psychological Medicine, 35, 1655–1665.
Slade, M., Leese, M., Cahill, S., Thornicroft, G., & Kuipers, E. (2005). Patient-rated mental health needs and quality of life improvement. British Journal of Psychiatry, 187, 256–261.
Doughty, C., & Tse, S. (2010). Can consumer-led mental health services be equally effective? An integrative review of CLMH services in high-income countries. Community Mental Health Journal, 47, 252–266.
Davidson, L., Chinman, M. J., Kloos, B., Weingarten, R., Stayner, D. A., & Tebes, J. K. (2005). Peer support among individuals with severe mental illness: A review of the evidence (pp. 412–450). Boston: Boston University Center for Psychiatric Rehabilitation.
Wood, A. L., & Wahl, O. F. (2006). Evaluating the effectiveness of a consumer-provided mental health recovery education presentation. Psychiatric Rehabilitation Journal, 30, 46–53.
Hsiung, P. C., Pan, A. W., Liu, S. K., Chen, S. C., Peng, S. Y., & Chung, L. (2010). Mastery and stigma in predicting the subjective quality of life of patients with schizophrenia in Taiwan. Journal of Nervous and Mental Disease, 198, 494–500.
Xiang, Y. T., Weng, Y. Z., Leung, C. M., Tang, W. K., & Ungvari, G. S. (2008). Subjective quality of life in outpatients with schizophrenia in Hong Kong and Beijing: Relationship to socio-demographic and clinical factors. Quality of Life Research, 17, 27–36.
Corrigan, P. W., Rafacz, J., & Rüsch, N. (2011). Examining a progressive model of self-stigma and its impact on people with serious mental illness. Psychiatry Research, 189, 339–343.
Acknowledgments
This study is supported by Research Grant 07080161 from the Health and Health Services Research Fund (HHSRF) of Hong Kong. We would like to express our sincere gratitude to the following nongovernmental organizations and mutual support group (in alphabetical order) for facilitating us in recruiting eligible participants from their service users/members: Amity Mutual Support Society; Baptist Oi Kwan Social Service; Christian Family Services; New Life Psychiatric Rehabilitation Association; and the Society of Rehabilitation and Crime Prevention.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chan, K.K.S., Mak, W.W.S. The mediating role of self-stigma and unmet needs on the recovery of people with schizophrenia living in the community. Qual Life Res 23, 2559–2568 (2014). https://doi.org/10.1007/s11136-014-0695-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-014-0695-7