Abstract
Purpose
The purpose of the study is to assess the quality-of-life scores and possible association with measures of ovarian reserve in female cancer survivors compared to healthy controls of similar age.
Methods
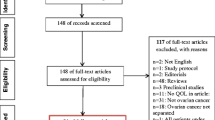
In this prospective cohort study, fifty-nine cancer survivors aged 16–39 years and 66 healthy, similarly aged unexposed women were recruited at the University of Pennsylvania. The primary outcome measures are the generic and cancer-specific domain scores on the Quality of Life in Adult Cancer Survivors (QLACS) instrument, early follicular phase serum hormones, follicle-stimulating hormone (FSH), luteinizing hormone (LH), estradiol (E2), inhibin B (INH), anti-Mullerian hormone (AMH), and ovarian ultrasound measurements [ovarian volume and antral follicle count (AFC)].
Results
Cancer survivors had significantly higher total and cancer-specific domain scores compared to unexposed participants. Serum AMH, INH, ovarian volume, and AFC were lower while serum FSH was higher in cancer survivors. Although survivors exhibited diminished ovarian reserve, these markers were not independently associated with total QLACS score. Cancer survivors with irregular menstrual function were found to have lower quality-of-life (QOL) scores than those with regular cycles.
Conclusions
We found that QOL appears to be significantly impaired in cancer survivors compared to controls, even when remote from initial cancer diagnosis. In addition, our study suggests that reproductive aging contributes to QOL in the setting of irregular menses and likely profound impairment of ovarian function.
Similar content being viewed by others
References
Zeltzer, L. K., Recklitis, C., Buchbinder, D., Zebrack, B., Casillas, J., Tsao, J. C., et al. (2009). Psychological status in childhood cancer survivors: A report from the Childhood Cancer Survivor Study. Journal of Clinical Oncology, 27, 2396–2404.
Schover, L. R. (2000). Psychosocial issues associated with cancer in pregnancy. Seminars in Oncology, 27, 699–703.
Howard-Anderson, J., Ganz, P. A., Bower, J. E., & Stanton, A. L. (2012). Quality of life, fertility concerns, and behavioral health outcomes in younger breast cancer survivors: A systematic review. Journal of the National Cancer Institute, 104, 386–405.
Janson, C., Leisenring, W., Cox, C., Termuhlen, A. M., Mertens, A. C., Whitton, J. A., et al. (2009). Predictors of marriage and divorce in adult survivors of childhood cancers: A report from the Childhood Cancer Survivor Study. Cancer Epidemiology Biomarkers Prevent, 18, 2626–2635.
Frobisher, C., Lancashire, E. R., Winter, D. L., Jenkinson, H. C., & Hawkins, M. M. (2007). British Childhood Cancer Survivor Study. Long-term population-based marriage rates among adult survivors of childhood cancer in Britain. International Journal of Cancer, 121, 846–855.
Gracia, C. R., Sammel, M. D., Freeman, E., Prewitt, M., Carlson, C., Ray, A., Vance, A., & Ginsberg, J. P. (2012). Impact of cancer therapies on ovarian reserve. Fertility and sterility, 97, 134,40.e1.
Mann, E., Singer, D., Pitkin, J., Panay, N., & Hunter, M. S. (2012). Psychosocial adjustment in women with premature menopause: A cross-sectional survey. Climacteric, 15(5), 481–489.
Green, D. M., Kawashima, T., Stovall, M., Leisenring, W., Sklar, C. A., Mertens, A. C., et al. (2009). Fertility of female survivors of childhood cancer: A report from the childhood cancer survivor study. Journal of Clinical Oncology, 27, 2677–2685.
Avis, N. E., Ip, E., & Foley, K. L. (2006). Evaluation of the Quality of Life in Adult Cancer Survivors (QLACS) scale for long-term cancer survivors in a sample of breast cancer survivors. Health Qual Life Outcomes, 4, 92.
Avis, N. E., Smith, K. W., McGraw, S., Smith, R. G., Petronis, V. M., & Carver, C. S. (2005). Assessing quality of life in adult cancer survivors (QLACS). Quality of Life Research, 14, 1007–1023.
Pearce, N. J., Sanson-Fisher, R., & Campbell, H. S. (2008). Measuring quality of life in cancer survivors: A methodological review of existing scales. Psychooncology, 17, 629–640.
Schover, L. R. (2009). Patient attitudes toward fertility preservation. Pediatric Blood & Cancer, 53, 281–284.
Schover, L. R., Brey, K., Lichtin, A., Lipshultz, L. I., & Jeha, S. (2002). Knowledge and experience regarding cancer, infertility, and sperm banking in younger male survivors. Journal of Clinical Oncology, 20, 1880–1889.
Schover, L. R., Rybicki, L. A., Martin, B. A., & Bringelsen, K. A. (1999). Having children after cancer. A pilot survey of survivors’ attitudes and experiences. Cancer, 86, 697–709.
Letourneau, J. M., Ebbel, E. E., Katz, P. P., Katz, A., Ai, W. Z., Chien, A. J., et al. (2012). Pretreatment fertility counseling and fertility preservation improve quality of life in reproductive age women with cancer. Cancer, 118, 1710–1717.
Partridge, A. H., Gelber, S., Peppercorn, J., Sampson, E., Knudsen, K., Laufer, M., et al. (2004). Web-based survey of fertility issues in young women with breast cancer. Journal of Clinical Oncology, 22, 4174–4183.
Ferrell, B. R., Grant, M. M., Funk, B. M., Otis-Green, S. A., & Garcia, N. J. (1998). Quality of life in breast cancer survivors: Implications for developing support services. Oncology Nursing Forum, 25, 887–895.
Carver, C. S., Smith, R. G., Petronis, V. M., & Antoni, M. H. (2006). Quality of life among long-term survivors of breast cancer: Different types of antecedents predict different classes of outcomes. Psychooncology, 15, 749–758.
Freeman, E. W., Sammel, M. D., Lin, H., Liu, Z., & Gracia, C. R. (2011). Duration of menopausal hot flushes and associated risk factors. Obstetrics and Gynecology, 117, 1095–1104.
Carpenter, J. S., Andrykowski, M. A., Cordova, M., Cunningham, L., Studts, J., McGrath, P., et al. (1998). Hot flashes in postmenopausal women treated for breast carcinoma: Prevalence, severity, correlates, management, and relation to quality of life. Cancer, 82, 1682–1691.
Zebrack, B. J., Foley, S., Wittmann, D., & Leonard, M. (2010). Sexual functioning in young adult survivors of childhood cancer. Psychooncology, 19, 814–822.
van Dijk, E. M., van Dulmen-den Broeder, E., Kaspers, G. J., van Dam, E. W., Braam, K. I., & Huisman, J. (2008). Psychosexual functioning of childhood cancer survivors. Psychooncology, 17, 506–511.
Grant, M. D., Piotrowski, Z. H., & Chappell, R. (1995). Self-reported health and survival in the Longitudinal Study of Aging, 1984–1986. Journal of Clinical Epidemiology, 48, 375–387.
Ferrell, B. R., Dow, K. H., & Grant, M. (1995). Measurement of the quality of life in cancer survivors. Quality of Life Research, 4, 523–531.
Acknowledgments
Supported by NIH T32 HD007440 and NIH 5K12HD001271-12 (LAK); Doris Duke Clinical Research Fellowship (KED); NIH K01 L1-CA-133839-03 and 1R01HD062797 (CRG, MDS).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kondapalli, L.A., Dillon, K.E., Sammel, M.D. et al. Quality of life in female cancer survivors: is it related to ovarian reserve?. Qual Life Res 23, 585–592 (2014). https://doi.org/10.1007/s11136-013-0473-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-013-0473-y