Abstract
Purpose
Higher daytime cortisol output has been associated with higher levels of perceived stress and worse mental and physical health outcomes. Hypothalamic–pituitary–adrenal (HPA) axis dysregulation, such as elevated secretion of daytime cortisol, occurs in many mental and physical illnesses. However, the nature of the association between functional health status and daytime cortisol production has not been established.
Methods
Healthy adult volunteers (n = 68, 45 females) provided saliva samples 3, 6, 9 and 12 h after waking, for two consecutive days, in everyday settings. Bivariate correlations between log salivary cortisol concentrations were calculated, and the SF-36 component summary scores were calculated. Latent growth curve modeling was used to model the daytime profile and adjust for covariates (age, sex and waking time).
Results
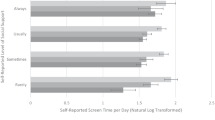
Higher PCS scores were not associated with cortisol three hours after waking (cortisol intercept), or the diurnal decline (cortisol slope). Higher MCS scores were correlated with faster cortisol decline across the day (r = −.31, P < .01) but not with cortisol intercepts. In a latent growth curve model adjusting for age, sex and waking time, the association was no longer statistically significant.
Conclusions
Large scale epidemiological studies involving salivary cortisol would benefit from measuring SF-36 component summary scores. Cortisol intercepts and slopes may be differentially related to the PCS and MCS, although greater statistical power is needed to test this hypothesis more fully. Associations between daytime cortisol and the PCS or MCS could reflect the regulatory competence of bodily systems, common causes or unmeasured confounding factors.


Similar content being viewed by others
References
van Praag, H. M., de Kloet, E. R., & van Os, J. (2004). Stress the brain and depression. Cambridge: Cambridge University Press.
Edwards, S., Evans, P., Hucklebridge, F., & Clow, A. (2001). Association between time of awakening and diurnal cortisol secretory activity. Psychoneuroendocrinology, 26(6), 613–622.
Edwards, S., Clow, A., Evans, P., & Hucklebridge, F. (2001). Exploration of the awakening cortisol response in relation to diurnal cortisol secretory activity. Life Sciences, 68(18), 2093–2103.
Bower, J., Ganz, P., Dickerson, S., Petersen, L., Aziz, N., & Fahey, J. (2005). Diurnal cortisol rhythm and fatigue in breast cancer survivors. Psychoneuroendocrinology, 30(1), 92–100.
Lindeberg, S., Eek, F., Lindbladh, E., Östergren, P. O., Hansen, Å. M., & Karlson, B. (2008). Exhaustion measured by the SF-36 vitality scale is associated with a flattened diurnal cortisol profile. Psychoneuroendocrinology, 33(4), 471–477.
Nicolson, N. A., & Van Diest, R. (2000). Salivary cortisol patterns in vital exhaustion. Journal of Psychosomatic Research, 49(5), 335–342.
Sjoumlgren, E., Leanderson, P., & Kristenson, M. (2006). Diurnal saliva cortisol levels and relations to psychosocial factors in a population sample of middle-aged Swedish men and women. International Journal of Behavioral Medicine, 13(3), 193–200.
McEwan, B. S. (1998). Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York Academy of Sciences, 840(1), 33–44.
McEwen, B. S. (2000). Allostasis and allostatic load: Implications for neuropsychopharmacology. Neuropsychopharmacology, 22(2), 108–124.
Sephton, S. E., Sapolsky, R. M., Kraemer, H. C., & Spiegel, D. (2000). Diurnal cortisol rhythm as a predictor of breast cancer survival. Journal of the National Cancer Institute, 92(12), 994–1000.
Sephton, S., & Spiegel, D. (2003). Circadian disruption in cancer: A neuroendocrine-immune pathway from stress to disease? Brain, Behavior and Immunity, 17(5), 321–328.
Spiegel, D., & Sephton, S. E. (2001). Psychoneuroimmune and endocrine pathways in cancer: Effects of stress and support. Seminars in Clinical Neuropsychiatry, 6(4), 252–265.
Clow, A., Thorn, L., Evans, P., & Hucklebridge, F. (2004). The awakening cortisol response: Methodological issues and significance. Stress, 7(1), 29–37.
Wust, S., Federenko, I., Hellhammer, D., & Kirschbaum, C. (2000). Genetic factors, perceived chronic stress, and the free cortisol response to awakening. Psychoneuroendocrinology, 25(7), 707–720.
Kaye, J. M., & Lightman, S. L. (2005). Psychological stress and endocrine axes. In K. Vedhara & M. Irwin (Eds.), Human psychoneuroimmunology (pp. 25–52). Oxford: Oxford University Press.
Kudielka, B. M., Hellhammer, D. H., & Wüst, S. (2009). Why do we respond so differently? Reviewing determinants of human salivary cortisol responses to challenge. Psychoneuroendocrinology, 34(1), 2–18.
Epel, E. S. (2009). Psychological and metabolic stress: A recipe for accelerated cellular aging? Hormones, 8(1), 7–22.
Ware, J. E., Snow, K. K., Kosisnki, M., & Gandek, B. (1993). SF-36 health survey manual and interpretation guide. Boston, MA: The Health Institute.
Ware, J. E., Kosinski, M., & Keller, S. K. (1994). SF-36 ® physical and mental health summary scales: A user’s manual. Boston, MA: The Health Institute.
Uhart, M., Chong, R. Y., Oswald, L., Lin, P.-I., & Wand, G. S. (2006). Gender differences in hypothalamic-pituitary-adrenal (HPA) axis reactivity. Psychoneuroendocrinology, 31(5), 642–652.
Edwards, S., Hucklebridge, F., Clow, A., & Evans, P. (2003). Components of the diurnal cortisol cycle in relation to upper respiratory symptoms and perceived stress. Psychosomatic Medicine, 65(2), 320–327.
Jenkinson, C., Layte, R., Wright, L., & Coulter, A. (1996). The U.K. SF-36: An analysis and interpretation manual. A guide to health status measurement with particular reference to the short form 36 health survey. Oxford: Health Services Research Unit, University of Oxford.
Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396.
Kirschbaum, C., & Hellhammer, D. (1994). Salivary cortisol in psychoneuroendocrine research: Recent developments and applications. Psychoneuroendocrinology, 19(4), 313–333.
Jemmott, J. (1987). Social motives and susceptibility to disease: Stalking individual differences in health risks. Journal of Personality, 55(2), 267–298.
Cohen, S., & Williams, G. S. (1993). Perceived stress in a probability sample of the US. In S. Spacapan & S. Oskamp (Eds.), The social psychology of health. Newbury Park, CA: SAGE.
Mikolajczyk, R., Maxwell, A., Naydenova, V., Meier, S., & El Ansari, W. (2008). Depressive symptoms and perceived burdens related to being a student: Survey in three European countries. Clinical Practice and Epidemiology in Mental Health, 4(1), 19.
Allgower, A., Wardle, J., & Steptoe, A. (2001). Depressive symptoms, social support, and personal health behaviors in young men and women. Health Psychology, 20(3), 223–227.
Bollen, K., & Curran, P. (2005). Latent curve models: A structural equation perspective. Hoboken, NJ: Wiley-Interscience.
Hruschka, D., Kohrt, B., & Worthman, C. (2005). Estimating between- and within-individual variation in cortisol levels using multilevel models. Psychoneuroendocrinology, 30(7), 698–714.
Rogosa, D., & Saner, H. (1995). Longitudinal data analysis examples with random coefficient models. Journal of Educational and Behavioral Statistics, 20(2), 149–170.
Curran, P. J. (2003). Have multilevel models been structural equation models all along? Multivariate Behavioral Research, 38(4), 529–569.
Muthén, L. K., & Muthén, B. O. (1998–2007). Mplus user’s guide, 5th Edn. Los Angeles, CA: Muthén & Muthén.
Hu, L., & Bentler, P. M. (1998). Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods, 3(4), 424–453.
Kramer, S. H., & Rosenthal, R. (1999). Effect sizes and significance levels in small-sample research. In R. H. Hoyle (Ed.), Statistical strategies for small sample research (pp. 60–79). Thousand Oaks, CA: SAGE.
Harris, A., Ursin, H., Murison, R., & Eriksen, H. R. (2007). Coffee, stress and cortisol in nursing staff. Psychoneuroendocrinology, 32(4), 322–330.
Kumari, M., Badrick, E., Chandola, T., Adam, E. K., Stafford, M., Marmot, M. G., et al. (2009). Cortisol secretion and fatigue: Associations in a community based cohort. Psychoneuroendocrinology, 34(10), 1476–1485.
Hellhammer, D., Wust, S., & Kudielka, B. (2009). Salivary cortisol as a biomarker in stress research. Psychoneuroendocrinology, 34(2), 163–171.
Vreeburg, S. A., Hoogendijk, W. J. G., van Pelt, J., DeRijk, R. H., Verhagen, J. C. M., van Dyck, R., et al. (2009). Major depressive disorder and hypothalamic-pituitary-adrenal axis activity: Results from a large cohort study. Archives of General Psychiatry, 66(6), 617–626.
Oswald, L. M., Zandi, P., Nestadt, G., Potash, J. B., Kalaydjian, A. E., & Wand, G. S. (2006). Relationship between cortisol responses to stress and personality. Neuropsychopharmacology, 31(7), 1583–1591.
Adam, E. K., & Kumari, M. (2009). Assessing salivary cortisol in large-scale, epidemiological research. Psychoneuroendocrinology, 34(10), 1423–1436.
Maddox, G. L., & Douglass, E. B. (1973). Self-assessment of health: A longitudinal study of elderly subjects. Journal of Health and Social Behavior, 14(1), 87–93.
Acknowledgments
Economic and Social Research Council. The University of Edinburgh Campaign (www.edinburghcampaign.com). We are grateful to Paul Dudgeon, Jeremy Miles and Yu-Kang Tu for their comments on earlier versions of this manuscript
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hagger-Johnson, G.E., Whiteman, M.C., Wawrzyniak, A.J. et al. The SF-36 component summary scales and the daytime diurnal cortisol profile. Qual Life Res 19, 643–651 (2010). https://doi.org/10.1007/s11136-010-9626-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-010-9626-4