Abstract
Purpose
The extent and variability of unmet care needs over time of people with systemic lupus erythematosus (SLE) has not been previously reported. A prospective study was undertaken to determine the variability over time of such needs.
Method
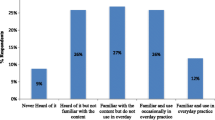
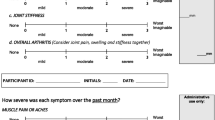
A 97-item SLE needs questionnaire (SLENQ) was completed on two occasions 6 months apart by 233 members of a lupus support association. Levels of unmet need for each individual, and a mean symptom score were calculated.
Results
Overall level of unmet need increased, decreased or stayed the same for 18%, 37%, and 45% of participants respectively. Ninety-four percent of participants at time 1 and 95% of participants at time 2 reported an unmet need for care for at least one item. The prevalence of unmet need for care remained the same for 82 of the 97 items. The mean unmet need score declined significantly between time 1 (0.78) and time 2 (0.69). The mean unmet need scores were significantly correlated with mean symptom score.
Conclusions
The results of the study suggest an unacceptable persistence of care needs not being met. There is an ongoing need to identify mechanisms to enhance care delivery so that the care needs of people with SLE are more effectively addressed.
Similar content being viewed by others
Abbreviations
- SLE:
-
Systemic lupus erythematosus
- SLENQ:
-
Systemic lupus erythematosus needs questionnaire
- QOL:
-
Quality of life
References
Swaak, A. J. G., van den Brink, H. G., Smeenk, R. J. T., Manger, K., Kalden, J. R., Tosi, S., et al. (1999). Systemic lupus erythematosus: clinical features in patients with a disease duration of over 10 years, first evaluation. Rheumatology, 38, 953–958. doi:10.1093/rheumatology/38.10.953.
Haq, I., & Isenberg, D. A. (2002). How does one assess and monitor patients with systemic lupus erythematosus in daily clinical practice? Best Practice & Research. Clinical Rheumatology, 16, 181–194. doi:10.1053/berh.2002.0220.
Klippel, J. (1990). Systemic lupus erythematosus: treatment-related complications superimposed on chronic disease. Journal of the American Medical Association, 263, 1812–1815. doi:10.1001/jama.263.13.1812.
Pierretti, J., Roman, M. J., Devereux, R. B., Lockshin, M. D., Crow, M. K., Paget, S. A., et al. (2007). Systemic lupus erythematosus predicts increased left ventricular mass. Circulation, 116, 419–426. doi:10.1161/CIRCULATIONAHA.106.673319.
Ward, M. M., Marx, A. S., & Barry, N. N. (2002). Psychological distress and changes in the activity of systemic lupus erythematosus. Rheumatology, 41, 184–188. doi:10.1093/rheumatology/41.2.184.
Petri, M., Genoves, M., Engle, E., & Hochberg, M. (1991). Definition, incidence and clinical description of flare in systemic lupus erythematosus. Arthritis and Rheumatism, 34, 937–944. doi:10.1002/art.1780340802.
Petri, M., Buyon, J., & Kim, M. (1999). Classification and definition of major flares in systemic lupus erythematosus clinical trials. Lupus, 8, 685–691. doi:10.1191/096120399680411281.
Abrass, C. K., Nies, K. M., Louie, J. S., Border, W. A., & Glassock, R. J. (1980). Correlation and predictive accuracy of circulating immune complexes with disease activity in patients with systemic lupus erythematosus. Arthritis and Rheumatism, 23, 273–282. doi:10.1002/art.1780230302.
Czar, M., & Engler, M. (1997). Perceived learning needs of patients with coronary artery disease using a questionnaire assessment tool. Heart Lung, 26, 109–117.
Aranda, S., Schofield, P., Weih, L., Yates, P., Milne, D., Faulkner, R., et al. (2005). Mapping the quality of life and unmet needs of urban women with metastatic breast cancer. European Journal of Cancer Care, 14, 211–222.
Rainbird, K. (1999). Measuring the perceived needs of patients with advanced, incurable cancer: towards evidenced based care of the dying. Dissertation, University of Newcastle
Browall, M., Carlsson, M., & Horvath, G. (2004). Information needs of women with recently diagnosed ovarian cancer—a longitudinal study. European Journal of Oncology Nursing: The Official Journal of European Oncology Nursing Society, 8, 200–207.
McCracken, L. M., Semenchuk, E. M., & Goetsch, V. L. (1995). Cross-sectional and longitudinal analyses of coping responses and health status in persons with systemic lupus erythematosus. Behavioral Medicine, 1995(20), 179–187.
Sutcliffe, N., Clarke, A. E., Levinton, C., Frost, C., Gordon, C., & Isenberg, D. A. (1999). Associates of health status in patients with systemic lupus erythematosus. The Journal of Rheumatology, 11(26), 2352–2356.
Moses, N., Wiggers, J., Cockburn, J., & Nicholas, C. (2007). Development and psychometric analysis of the systemic lupus erythematosus needs questionnaire (SLENQ). Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 16, 461–466.
Moses, N., Wiggers, J., Cockburn, J., & Nicholas, C. (2005). Prevalence and correlates of perceived unmet needs of people with systemic lupus erythematosus. Patient Education and Counseling, 57, 30–38.
Stein, H., Walters, K., Dillon, A., & Schulzer., M. (1980). Systemic lupus erythematosus—a medical and social profile. The Journal of Rheumatology, 13, 570–576.
Wallace, D. (1995). The lupus book. New York: Oxford University Press.
Hays, R. D., Brodsky, M., Johnston, M. F., Spritzer, K. L., & Hui, K. (2005). Evaluating The statistical significance of health-related quality-of-life change in individual Patients. Evaluation & the Health Professions, 28, 160–171.
Costenbader, K. H., Brome, D., Blanch, D., Gall, V., Karlson, E., & Liang, M. H. (2007). Factors determining participation in prevention trials among systemic lupus erythematosus: a qualitative study. Arthritis and Rheumatism, 57, 49–55.
Yelin, E., Trupin, L., Katz, P., Criswell, L., Yazdany, J., Gillis, J., et al. (2007). Work dynamics among persons with systemic lupus erythematosus. Arthritis and Rheumatism, 57, 56–63.
Bauman, A., Barnes, C., Schrieber, L., Dunsmore, J., & Brooks, P. (1989). The unmet needs of patients with systemic lupus erythematosus: planning for patient education. Patient Education and Counseling, 14, 235–42.
Panopalis, P., Petri, M., Manzi, S., Isenberg, D. A., Gordon, C., Senecal, J. L., et al. (2005). The systemic lupus erythematosus tri-nation study: longitudinal changes in physical and mental well-being. Rheumatology, 44, 751–755.
Kuriya, B., Gladman, D., Ibanez, D., & Urowitz, M. (2008). Quality of life over time in patients with systemic lupus erythematosus. Arthritis and Rheumatism, 59, 181–185.
Leong, K. P., Kong, K. O., Thong, B. Y. H., Thong, E. T., Koh, E. T., Lian, T. Y., et al. (2005). Development and preliminary validation of a systemic lupus erythematosus-specific quality-of-life instrument (SLEQOL). Rheumatology, 44, 1267–1276.
Holden, J. D. (2001). Hawthorne effects and research into professional practice. Journal of Evaluation in Clinical Practice, 7, 65–70.
Hasan, T., Pertovaara, M., Yli-Kerttula, U., Lukkaala, T., & Korpela, M. (2004). Seasonal variation of disease activity of systemic lupus erythematosus in Finland: a 1 year follow up study. Annals of the Rheumatic Diseases, 63, 1498–1500.
Maeshima, E., Liang, X. M., Otani, H., Mune, M., & Yukawa, S. (2002). Effect of environmental changes on oxidative deoxyribonucleic acid (DNA) damage in systemic lupus erythematosus. Archives of Environmental Health, 57, 425–428.
Voss, A. B., Green, A., & Junker, P. (1999). Systemic lupus erythematosus in the county of Fynen. (Danish). An epidemiological study. Ugeskrift for Laeger, 161, 3837–3840.
Uramoto, K. M., Michet, C. J., Jr, Thumboo, J., Sunku, J., O’Fallon, W. M., & Gabriel, S. E. (1999). Trends in the incidence and mortality of systemic lupus erythematosus. Arthritis and Rheumatism, 42, 46–50.
Anstey, N. M., Bastian, I., Dunkley, H., & Currie, B. J. (1993). Systemic lupus erythematosus in Australian Aborigines: high prevalence, morbidity and mortality. Australian and New Zealand Journal of Medicine, 23, 646–651.
Australian Bureau of Statistics. (2002). 2001 Census community profile: New South Wales. Canberra: ABS.
Hopkinson, N., Doherty, M., & Powell, R. J. (1994). Clinical features and race specific incidence/prevalence rates of systemic lupus erythematosus in a geographically complete cohort of patients. Annals of the Rheumatic Diseases, 53, 675–680.
Fitzgerald, J. D., & Grossman, J. M. (1999). Validity and reliability of retrospective assessment of disease activity and flare in observational cohorts of lupus patients. Lupus, 8, 638–644.
Gustafson, D. (1991). Expanding on the role of patient as consumer. QRB, October, pp. 324–325
Acknowledgments
The authors wish to thank the members and staff of the Lupus Association of NSW for their ongoing and generous assistance during the many phases of this project. This paper was prepared with infrastructure support from the Hunter Medical Research Institute.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was conducted with ethics approval from the University of Newcastle Hunter Research Ethics Committee (HREC: H6820499) and the Hunter Area Health Service–Hunter Area Human Ethics Committee (HAHREC: 9904213.17), and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki.
Rights and permissions
About this article
Cite this article
Moses, N., Wiggers, J. & Nicholas, C. Persistence of unmet need for care among people with systemic lupus erythematosus: a longitudinal study. Qual Life Res 17, 867–876 (2008). https://doi.org/10.1007/s11136-008-9361-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-008-9361-2