Abstract
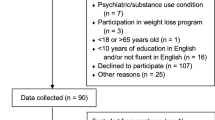
Despite reasonable knowledge of body dysmorphic disorder (BDD), little is known of its cognitive antecedents. In this study, we evaluated executive functioning and decision-making in people at risk of developing BDD using neuropsychological tests. Participants were non-treatment seeking volunteers (18–29 years) recruited from the general community, and split into two groups: those “at risk” of developing BDD (N = 5) and controls (N = 82). Participants undertook the One-Touch Stockings of Cambridge, Cambridge Gamble and Spatial Working Memory tasks and were assessed with the Body Dysmorphic Disorder Questionnaire. Results showed that the at-risk subjects performed significantly worse on a measure of executive function, whereas measures of risk-seeking behavior, quality of decision-making, and spatial working memory were largely intact. The findings suggest that selective cognitive dysfunction may already be present in terms of executive functioning in those at risk of developing BDD, even before psychopathology arises.
Similar content being viewed by others
References
Phillips KA, Wilhelm S, Koran LM, Didie ER, Fallon BA, Feusner J, et al. Body dysmorphic disorder: Some key issues for DSM-V. Depress Anxiety 2010;27:573–91. doi:10.1002/da.20709.
Rief W, Buhlmann U, Wilhelm S, Borkenhagen A, Brähler E. The prevalence of body dysmorphic disorder: A population-based survey. Psychol Med 2006;36:877–85. doi:10.1017/S0033291706007264.
Koran LM, Abujaoude E, Large MD, Serpe RT. The prevalence of body dysmorphic disorder in the United States adult population. CNS Spectr 2008;13:316–22.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5. 5 edition. Washington, D.C: American Psychiatric Publishing; 2013.
Phillips KA. Handbook on Obsessive-Compulsive and Related Disorders. 1 edition. American Psychiatric Publishing; 2015.
Feusner JD, Townsend J, Bystritsky A, Bookheimer S. Visual information processing of faces in body dysmorphic disorder. Arch Gen Psychiatry 2007;64:1417–25. doi:10.1001/archpsyc.64.12.1417.
Feusner JD, Hembacher E, Moller H, Moody TD. Abnormalities of object visual processing in body dysmorphic disorder. Psychol Med 2011;41:2385–97. doi:10.1017/S0033291711000572.
Feusner JD, Moody T, Hembacher E, Townsend J, McKinley M, Moller H, et al. Abnormalities of visual processing and frontostriatal systems in body dysmorphic disorder. Arch Gen Psychiatry 2010;67:197–205. doi:10.1001/archgenpsychiatry.2009.190.
Rauch SL, Phillips KA, Segal E, Makris N, Shin LM, Whalen PJ, et al. A preliminary morphometric magnetic resonance imaging study of regional brain volumes in body dysmorphic disorder. Psychiatry Res 2003;122:13–9.
Atmaca M, Bingol I, Aydin A, Yildirim H, Okur I, Yildirim MA, et al. Brain morphology of patients with body dysmorphic disorder. J Affect Disord 2010;123:258–63. doi:10.1016/j.jad.2009.08.012.
Feusner JD, Townsend J, Bystritsky A, McKinley M, Moller H, Bookheimer S. Regional brain volumes and symptom severity in body dysmorphic disorder. Psychiatry Res 2009;172:161–7. doi:10.1016/j.pscychresns.2008.12.003.
Buchanan BG, Rossell SL, Maller JJ, Toh WL, Brennan S, Castle DJ. Brain connectivity in body dysmorphic disorder compared with controls: A diffusion tensor imaging study. Psychol Med 2013;43:2513–21. doi:10.1017/S0033291713000421.
Feusner JD, Arienzo D, Li W, Zhan L, Gadelkarim J, Thompson PM, et al. White matter microstructure in body dysmorphic disorder and its clinical correlates. Psychiatry Res 2013;211:132–40. doi:10.1016/j.pscychresns.2012.11.001.
Arienzo D, Leow A, Brown JA, Zhan L, Gadelkarim J, Hovav S, et al. Abnormal brain network organization in body dysmorphic disorder. Neuropsychopharmacol Off Publ Am Coll Neuropsychopharmacol 2013;38:1130–9. doi:10.1038/npp.2013.18.
Hanes KR. Neuropsychological performance in body dysmorphic disorder. J Int Neuropsychol Soc JINS 1998;4:167–71.
Deckersbach T, Savage CR, Phillips KA, Wilhelm S, Buhlmann U, Rauch SL, et al. Characteristics of memory dysfunction in body dysmorphic disorder. J Int Neuropsychol Soc JINS 2000;6:673–81.
Dunai J, Labuschagne I, Castle DJ, Kyrios M, Rossell SL. Executive function in body dysmorphic disorder. Psychol Med 2010;40:1541–8. doi:10.1017/S003329170999198X.
Buhlmann U, Etcoff NL, Wilhelm S. Emotion recognition bias for contempt and anger in body dysmorphic disorder. J Psychiatr Res 2006;40:105–11. doi:10.1016/j.jpsychires.2005.03.006.
Buhlmann U, Wilhelm S, McNally RJ, Tuschen-Caffier B, Baer L, Jenike MA. Interpretive biases for ambiguous information in body dysmorphic disorder. CNS Spectr 2002;7:435–6, 441–3.
Toh WL, Castle DJ, Rossell SL. Attentional biases in body dysmorphic disorder (bdd): Eye-tracking using the emotional Stroop task. Compr Psychiatry 2017;74:151–61. doi:10.1016/j.comppsych.2017.01.014.
Jefferies-Sewell K, Chamberlain SR, Fineberg NA, Laws KR. Cognitive dysfunction in body dysmorphic disorder: New implications for nosological systems and neurobiological models. CNS Spectr 2016:1–10. doi:10.1017/S1092852916000468.
Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol 1959;32:50–5.
Hamilton M. A rating scale for Depression. J Neurol Neurosurg Psychiatry 1960;23:56–62. doi:10.1136/jnnp.23.1.56.
Frisch MB, Cornell J, Villanueva M, Retzlaff PJ. Clinical validation of the quality of life Inventory. A measure of life satisfaction for use in treatment planning and outcome assessment. Psychol Assess 1992;4:92–101. doi:10.1037/1040-3590.4.1.92.
Grant JE, Kim SW, Crow SJ. Prevalence and clinical features of body dysmorphic disorder in adolescent and adult psychiatric inpatients. J Clin Psychiatry 2001;62:517–22.
Toh WL, Castle DJ, Rossell SL. Examining neurocognition in body dysmorphic disorder using the repeatable battery for the assessment of neuropsychological status (RBANS): A comparison with obsessive-compulsive disorder. Psychiatry Res 2015;228:318–24. doi:10.1016/j.psychres.2015.05.094.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Written informed consent was obtained from all study participants. The Institutional Review Board for the University of Chicago approved the study and the consent.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Funding
Dr. Grant has received research grants from NIMH, National Center for Responsible Gaming, the American Foundation for Suicide Prevention, the Trichotillomania Learning Center, Brainsway, Takeda, and Psyadon Pharmaceuticals. He receives yearly compensation from Springer Publishing for acting as Editor-in-Chief of the Journal of Gambling Studies and has received royalties from Oxford University Press, American Psychiatric Publishing, Inc., Norton Press, and McGraw Hill. Mr. Blum and Ms. Redden report no financial relationships with commercial interests.
Rights and permissions
About this article
Cite this article
Blum, A.W., Redden, S.A. & Grant, J.E. Neurocognitive Functioning in Young Adults with Subclinical Body Dysmorphic Disorder. Psychiatr Q 89, 45–52 (2018). https://doi.org/10.1007/s11126-017-9510-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-017-9510-2