Abstract
Prevention researchers have advocated primary prevention such as vaccination in alternative venues. However, there have been major questions about both the attendance of, and the ability to, vaccinate high-risk individuals in such settings. The current study seeks to assess the feasibility of vaccinating high-risk men who have sex with men (MSM) at Gay Pride events. The research questions are: Do gay men who are sampled at Gay Pride events engage in more or less risky behavior than gay men sampled at other venues? Do the gay men who receive hepatitis vaccinations at Gay Pride engage in more or less risky behavior than gay men at Gay Pride who do not receive hepatitis vaccination? Of the 3689 MSM that completed the Field Risk Assessment (FRA), 1095/3689 = 29.68% were recruited at either the 2006 or 2007 Long Beach, California Gay Pride events. The remaining, 2594/3689 = 70.32% were recruited at Long Beach gay bars, gay community organizations and institutions, and through street recruitment in various gay enclaves in the Long Beach area. Logistic regression analysis yielded eight factors that were associated with non-attendance of Gay Pride: Age, had sex while high in the last 12 months, had unprotected anal intercourse (UAI) in the last 12 months, had sex for drugs/money in the last 12 months, been diagnosed with a sexually transmitted infection (STI) in the last 12 months, used nitrites (poppers) in the last 12 months, and used methamphetamine in the last 12 months. Identifying as White, Asian, or African American compared to Hispanic was also associated with non-attendance. Bivariate analysis indicated that, of the MSM sampled at Gay Pride, 280/1095 = 25.57% received a hepatitis vaccination there. The MSM sampled at Gay Pride who reported engaging in UAI or having used any stimulant (cocaine, crack-cocaine, or methamphetamine) in the last 12 months were more likely to receive hepatitis vaccination on-site. The results provide evidence for the viability of successfully vaccinating high-risk MSM at Gay Pride events. However, it is vital that no-cost vaccinations are also funded in other community settings such as STI clinics, drug treatment programs, prisons, universities, and other community resource centers in order to reach those additional high-risk MSM who do not attend Gay Pride.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
U.S. rates of the hepatitis A virus (HAV) and hepatitis B virus (HBV) have been steadily dropping since the introduction of the HAV and HBV vaccines in 1995 and 1982 respectively (Bondesson and Saperston 1996). Unfortunately, this decline has excluded men who have sex with men (MSM) (Levine 2003a; MacKellar et al. 2001). According to the Centers for Disease Control and Prevention (CDC; 2006a, 2006b), MSM account for 10% of new HAV cases and 15 to 20% of new HBV cases each year. This is particularly alarming considering that MSM constitute only 8% of the U.S. male population and that less than half of all MSM in the U.S. have received either the HAV or HBV vaccine (Diamond et al. 2003). In one study of hepatitis vaccination in New York City, only 70% of gym-attending gay men reported having been vaccinated for HBV (Siconolfi et al. 2009).
Oral-anal contact or “rimming” places MSM at heightened risk for acquiring HAV which is spread through fecal-oral contact (Jacobsen and Koopman 2004; Mazick et al. 2005). HBV is transmitted among MSM through high-risk sexual behavior such as unprotected anal intercourse (UAI) that results in the sharing of blood or semen (Ostrow et al. 1999; Seage et al. 1997; Szmuness et al. 1975). Drugs that have been shown to impair judgment such as cocaine, crack-cocaine, and methamphetamine, have been linked to higher rates of UAI among MSM (Appleby et al. 2007; Colfax et al. 2005; Fisher et al. 2009; Halkitis et al. 2006; Hirshfield et al. 2004; Semple et al. 2002; Springer et al. 2007). Because engaging in high-risk behaviors places MSM at elevated risk for contracting HAV and HBV, it is paramount that vaccinations are made readily available and promoted among this high-risk group.
Identifying the gaps in both HAV and HBV vaccine coverage among high-risk MSM is essential for targeting the delivery of an effective vaccine. Once the gaps have been identified, the question that follows is: What is the best approach to reach these high-risk MSM for vaccination? Traditionally, the majority of MSM who have received HAV and HBV vaccinations have used a regular source of health care such as a private physician, school, hospital or community health clinic (Alter et al. 1990; MacKellar et al. 2001; McCusker et al. 1990; Rabeneck et al. 1993). Unfortunately, this results in only 1 in 10 MSM at risk for HAV and HBV infection receiving vaccination (MacKellar et al. 2001). MSM are not being educated about the risks associated with HAV and HBV, nor are suggestions for vaccination being made on a regular basis in these health care settings (Diamond et al. 2003; Gunn et al. 2001; Kahn 2002). This is despite a major public service announcement campaign that was aimed at those at high risk of hepatitis including gay men (MacDougall 1998). One possible explanation for the lack of vaccination is that many MSM do not disclose their sexual orientation to their primary care providers and, as a result, the providers are not aware of the elevated risk to their patients (Betts 2002; MacKellar et al. 2001; Martinson et al. 1996).
Public health researchers have advocated hepatitis vaccine service delivery in alternative venues (Des Jarlais et al. 2001; Trubatch et al. 2000); however, there has been a major question about the willingness of high-risk MSM to be vaccinated in such settings. One alternative venue for accessing MSM for vaccination is through local Gay Pride events (Allard et al. 2001). Gay Pride is a locally organized festival that takes place in over 100 cities around the U.S. each year (Kates and Belk 2001). Long Beach, California is one of the cities that holds a Gay Pride event. As stated in the City’s Consolidated Plan, Long Beach is considered to be the most ethnically diverse major city in the United States. The racial /ethnic composition in Long Beach as of the 2000 Census, is as follows: 33% White, 36% Hispanic, 15% African American, 13% Asian, and other racial groups represent the remaining 3% of the population. The percentage of Hispanics has been increasing in recent years. The Long Beach Gay Pride is the second largest in California after San Francisco.
Gay Pride events in other cities have been successfully utilized for sampling MSM populations for research, Human Immunodeficiency Virus (HIV)-prevention education, HIV rapid testing, and other health-promotion efforts (Brennan et al. 2007; Eaton et al. 2007; Gallagher et al. 2007; Kalichman et al. 2004). One advantage to using Gay Pride events is the ability to capture MSM who may not disclose their high-risk behaviors to their health care providers (Levine 2003a). There is a need to understand the factors that would facilitate and optimize hepatitis vaccination programs (Levine 2003b). However, one must first ask the questions: (a) Are those men who go to gay bars and other gay venues, different from those who attend Gay Pride? and (b) Are those high-risk MSM who attend Gay Pride reached by an on-site vaccination effort? The current study will contribute to this understanding by describing the predictors of Gay Pride attendance among MSM and then describing the successful vaccination of high-risk MSM for HAV and HBV at two Gay Pride events.
Methods
Participants
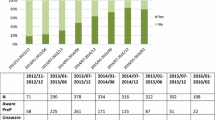
A total of 3689 MSM were recruited for the current study. The eligibility requirement for participation was identifying as male and reporting having had sex with a man in the last 5 years. The majority (n = 2594) of MSM were recruited through gay bars and organizations, and street recruitment in various gay enclaves in the Long Beach, California area. These MSM were administered a brief Field Risk Assessment (FRA) interview at the recruitment site and were then referred to the Center for Behavioral Research and Services (CBRS) in Long Beach for participation in an individual-level sexually transmitted infection (STI)/HIV risk-reduction program. The remaining 1095 MSM were recruited at either the 2006 or 2007 Long Beach Gay Pride events. The Gay Pride participants initially completed the brief FRA and were then referred to the CBRS’ vaccination station for the HAV and HBV vaccinations located on site at Gay Pride. Table 1 demonstrates the age and ethnic distribution of MSM recruited at Gay Pride versus those recruited at locations other than Gay Pride.
Measures
The Field Risk Assessment (FRA), a 36-item structured interview, was used for assessment of the MSM’s demographics as well as their reported drug use and sexual behavior (Kochems et al. 2008).
Vaccination Procedures
Participants at Gay Pride were approached by outreach workers from CBRS and Hep Team Los Angeles and offered the combined HAV/HBV vaccine (TWINRIX®, GlaxoSmithKline). After providing documentation that they were at least 18 years old and signing the informed consent form, the FRA questionnaire was administered by CBRS outreach staff. After completing the FRA, the participant was then shown to the vaccination station. The vaccination station was staffed with one volunteer physician, one volunteer nurse practitioner, and several volunteer registered nurses. There, the nurse (or physician) assessed for any contraindications for the vaccinations, reviewed the informed consent form, and provided the vaccine information sheets as per CDC guidelines; this took approximately 5–15 min. After reconfirming the participant’s intention to obtain the HAV/HBV vaccine, the nurse administered the hepatitis adult vaccines via intramuscular route as stated in the product package insert recommendations.
After injection, the participant was reminded of the need to return for the second dose one month after the first dose and for the third dose, six months after the first. Participants were provided with reminder cards of the recommended vaccine schedule, which they addressed to themselves at the address of their choice. These reminder cards were then retained by the nurse for mailing about one week prior to the time that the participant would be due for the 2nd dose of vaccine. No participant experienced any reactions or adverse events that would constitute a contraindication during the two days of either the 2006 or the 2007 Pride event.
Statistical Analysis
Data were entered in Viking Data Entry and Images version 4.2 (Viking Software Solutions 2001). Analysis was then conducted in SAS version 9.1.3 service pack 4 on a Windows 2003 server. To understand the characteristics of those attending Gay Pride, we constructed a logistic regression model predicting Gay Pride attendance. To describe the success of the vaccination efforts, bivariate analyses were used to determine the relationship between participant high-risk behavior and receipt of hepatitis vaccination.
Results
Table 1 presents the bivariate analysis of Gay Pride attendance among the overall sample of MSM. The analysis demonstrates a consistent pattern of sexual risk behavior and drug use behavior being associated with non-attendance at Gay Pride. Methamphetamine, crack-cocaine, nitrites (poppers), and Viagra® were especially prevalent in the analysis.
Table 2 shows the logistic regression model predicting Gay Pride attendance for the overall sample of MSM. The analysis yields a predictive model of eight factors that are associated with non-attendance at Gay Pride. These factors are associated with age, ethnicity, drug use, and high-risk sexual behavior as indicated by negative coefficients and odds ratios of less than one.
Table 3 provides bivariate analyses indicating that, of the MSM sample who were recruited at Gay Pride, 280/1095 = 25.57% (CI .95 = 23.01, 28.26) received a hepatitis vaccination. Interestingly, the MSM who reported engaging in UAI in the last 12 months were significantly more likely to have been vaccinated at Gay Pride. Also, the MSM who reported using illicit stimulants (cocaine, crack-cocaine, or methamphetamine) in the last 12 months were also significantly more likely to have obtained a hepatitis vaccination at Gay Pride. The other variables that were included in Table 1 are also included in Table 3 for comparison purposes. Most of these other variables, including ethnicity and age of participants, were not significantly associated with hepatitis vaccination.
Discussion
This study’s major findings are twofold. First, Gay Pride events were demonstrated to be a useful venue for vaccinating MSM at high-risk for contracting HAV and HBV. That is to say that the MSM who engage in high-risk behavior, those using illicit drugs and engaging in UAI, are more likely to get vaccinated than other attendees at a Gay Pride event. The second finding suggests that while recruitment of high-risk MSM for HAV and HBV vaccination was achieved at several Gay Pride events, many MSM who are at an elevated risk for HAV and HBV, those engaging in even higher rates of UAI, sex while high, illicit drug use, those trading sex for drugs or money, and those diagnosed with an STI in the last 12-months are not attending such events and that additional vaccination venues are needed to adequately target those gay men at higher risk than those who attend Gay Pride events.
The use of methamphetamine, nitrites, and Viagra® has been associated with higher rates of UAI among MSM (Crosby et al. 1996; Dolezal et al. 2000; Fisher et al. 1992; Mansergh et al. 2006; Parsons et al. 2003; Schwarcz et al. 2007; Spindler et al. 2007). Research has shown that MSM who use methamphetamine, nitrites and Viagra® have a significantly higher prevalence of HBV infection (Drumright et al. 2007; Fisher et al. 2009). The current study found that rates of methamphetamine, nitrites, and Viagra® use were higher among those MSM who did not attend Gay Pride indicating that Gay Pride, even though it is a useful and feasible vaccination venue, will not adequately target the gay men at highest risk of hepatitis.
One possible explanation for the riskiest MSM not attending Gay Pride may be directly related to socio-economic status. The 2006 and 2007 Long Beach Gay Pride event cost attendees $20 per day for admittance. Given that many of the persons at greatest risk for infection also have financial difficulties that may or may not be related to their risk behavior, these individuals may have found the admittance fee to be unduly burdensome and an impediment to Gay Pride attendance (Jin et al. 2004; Ostrow et al. 1999). The Gay Pride attendance fee likely prevented some high-risk MSM at lower income levels from attending.
Another possible explanation may be more social in nature. Many MSM do not openly identify as gay or bisexual for various reasons. We speculate that those who do not identify as gay or bisexual may also be less likely to attend events that are described as catering specifically to gay and bisexual participants. Further, some MSM identify as heterosexual, or are inconsistent in their sexual identity, even though they have sex with men and are at higher risk, for HIV and presumably HBV, than those who are consistent in their identity (Washington et al. 2006). These MSM have been reported to be a challenge for HIV prevention programs and may be especially difficult to vaccinate for hepatitis in the type of vaccination program that was offered because they may be less likely to attend a Gay Pride event that so clearly advertises an identity they may not be comfortable embracing (Goldbaum et al. 1998). Even though these MSM may not identify as gay or bisexual, they may be at an elevated risk for HAV and HBV because of possible high rates of sex and drug using behavior (Washington et al. 2006). These men would also benefit greatly from no-cost hepatitis vaccination (Wohl et al. 2002).
The current study found that MSM who attended Gay Pride in Long Beach, California were more likely to be Hispanic than White, African American, or Asian. A recent assessment found that, of 11 Gay Pride events in 9 U.S. cities from 2004 to 2006, most of the events were attended primarily by MSM who identified as an ethnic minority (Centers for Disease Control and Prevention 2007). This finding parallels the findings at the Long Beach, California Gay Pride events, given the influx of Hispanics to Southern California (Suro and Singer 2001). Conversely, the respective shortage of Hispanics sampled at venues other than Gay Pride can be partially explained by the fact that our outreach team during this study’s years was made up of men who identified as African American, Asian, and White, with limited Spanish speaking proficiency, and hence the Gay Latino venues proved to be more challenging recruitment sites. It has been well established in the literature that Hispanics are at highest risk for hepatitis A (Hayes-Bautistia et al. 2005; Saab et al. 2005; Wise and Sorvillo 2005). The implication of this finding is that Gay Pride is an excellent opportunity to vaccinate Hispanic gay men for hepatitis A. The fact that we vaccinated for both hepatitis A and hepatitis B also takes into account that there is an association between these two diseases in Los Angeles County (Fisher et al. 2006), and that vaccinating for both instead of just one has been found to be cost effective (Jacobs et al. 2004).
Age was another factor that influenced Gay Pride attendance. MSM recruited at Gay Pride were younger on average than MSM recruited among other venues. This finding is consistent with previous research that has indicated younger MSM were more likely to attend Gay Pride (Friedman et al. 2000; Gallagher et al. 2007). This finding is likely influenced in part by the 21-year-old minimum age requirement for attending the Long Beach bars and clubs where many MSM were recruited. The Long Beach Gay Pride events did not have minimum age requirements and subsequently the outreach team was able to access younger MSM.
The question for prevention researchers now becomes: What is the optimal overall strategy to vaccinate high-risk MSM? Previous research has demonstrated successful hepatitis vaccination of injection drug users at syringe exchange sites (Altice et al. 2005; Des Jarlais et al. 2001). Vaccination services have also been successfully demonstrated at drug rehabilitation programs (Gunn et al. 2005), prisons (Sutton et al. 2005), university health services (Neighbors et al. 1999), STI clinics, and various other community health organizations (Gunn et al. 2007; Sansom et al. 2003; Trubatch et al. 2000). These avenues may be alternative ways of reaching high-risk MSM who do not attend Gay Pride events or openly disclose their sexual behaviors. Several studies also underscore the major role promotional messages in the gay media have played both in raising awareness and facilitating referral of MSM to health care organizations for hepatitis vaccination (Friedman et al. 2000; Warwick et al. 2007).
CBRS vaccinated the maximum number of MSM possible at Gay Pride. However, due to funding constraints, the number of vaccinations provided did not meet the need of all MSM who desired vaccination. Therefore, while 25.57% of the MSM sampled at Gay Pride were vaccinated, the authors suggest that more MSM would have been vaccinated had the resources been available. This is similar to the resource limitation for HIV testing at Gay Pride events that has been pointed out by the CDC (2007). The HAV/HBV combined vaccination that was administered at the 2006 and 2007 Long Beach Gay Pride events was the first of a three-shot series that also includes 30-day and 6-month administrations. Future research should address the rates at which MSM vaccinated at Gay Pride events adhered to their complete vaccination schedule (Rhodes and Diclemente 2003), as the number who received the first of the hepatitis vaccination series does not represent those who completed the series (Des Jarlais et al. 2001; Trubatch et al. 2000).
Limitations
One limitation of the current study is that measurement of adherence to the remainder of the vaccination schedule among those recruited and initially vaccinated at Gay Pride was not possible. A second limitation is the reliance of self-report in public venues when private settings could not be provided. Participants may have under-reported risk behavior during the assessment. The FRA was very limited in the variables it collected because it was designed to be used for initial encounters in the field. It did not collect income, education, and history of previous vaccination.
In light of the results of the current study, the authors advocate that public health efforts take a comprehensive approach to targeting high-risk MSM for HAV and HBV vaccination. Because of the demonstrated success of vaccinating MSM at Gay Pride events, it is crucial that the opportunities afforded by these venues be exploited for public health benefit. However, it is equally important that no-cost vaccinations be funded in various other community venues such as STI clinics, drug treatment programs, prisons, universities, and other community resource centers. With adequate funding for community no-cost vaccination, including the continued efforts of vaccinating at Gay Pride events, the eradication of both HAV and HBV in the U.S. may soon become a reality.
References
Allard, R., Beauchemin, J., Bedard, L., Dion, R., Tremblay, M., & Carsley, J. (2001). Hepatitis A vaccination during an outbreak among gay men in Montreal, Canada, 1995–1997. Journal of Epidemiology and Community Health, 55, 251–256. doi:10.1136/jech.55.4.251.
Alter, M. J., Hadler, S. C., Margolis, H. S., Alexander, W. J., Hu, P. Y., Judson, F. N., et al. (1990). The changing epidemiology of hepatitis B in the United States: Need for alternative vaccination strategies. Journal of the American Medical Association, 263, 1218–1222.
Altice, F., Bruce, R., Walton, M., & Buitrago, M. (2005). Adherence to hepatitis B virus vaccination at syringe exchange sites. Journal of Urban Health, 82, 151–161.
Appleby, P. R., Storholm, E. D., Ayala, A., & Miller, L. C. (2007). Methamphetamine and risky decision making among men who have sex with men. Paper presented at the 19th annual convention of the Association for Psychological Science, Washington, DC.
Betts, K. S. (2002). Protection against STDs, hepatitis, and HIV/AIDS includes talking openly and honestly with sex partners and medical care providers. Journal of the Gay and Lesbian Medical Association, 6, 111–115.
Bondesson, J. D., & Saperston, A. R. (1996). Hepatitis. Emergency Medicine Clinics of North America, 14, 695–718.
Brennan, D. J., Hellerstedt, W. L., Ross, M. W., & Welles, S. L. (2007). History of childhood sexual abuse and HIV risk behaviors in homosexual and bisexual men. American Journal of Public Health, 97, 1107–1112. doi:AJPH.2005.071423 [pii]10.2105/AJPH.2005.071423.
Center for Disease Control and Prevention. (2006a). Hepatitis A prevention for men who have sex with men. Resources for Gay Men's Health Retrieved June 10, 2008, from http://www.cdc.gov/Ncidod/disease/hepatitis/msm/hav_msm_fact.htm.
Center for Disease Control and Prevention. (2006b). Hepatitis B prevention for men who have sex with men. Resources for Gay Men's Health Retrieved June 10, 2008, from http://www.cdc.gov/Ncidod/disease/hepatitis/msm/hbv_msm_fact.htm.
Centers for Disease Control and Prevention. (2007). Rapid HIV testing among racial/ethnic minority men at gay pride events—nine U.S. cities, 2004–2006. Morbidity and Mortality Weekly Report, 56, 602–604.
Colfax, G., Coates, T. J., Husnik, M. J., Huang, Y., Buchbinder, S., Koblin, B., et al. (2005). Longitudinal patterns of methamphetamine, popper (amyl nitrite), and cocaine use and high-risk sexual behavior among a cohort of San Francisco men who have sex with men. Journal of Urban Health, 82, 62–70. doi:jti025 [pii]10.1093/jurban/jti025.
Crosby, G. M., Stall, R. D., Paul, J. P., Barrett, D. C., & Midanik, L. T. (1996). Condom use among gay/bisexual male substance abusers using the timeline follow-back method. Psychology of Addictive Behaviors, 21, 249–257. doi:0306-4603(96)00055-X [pii].
Des Jarlais, D. C., Fisher, D. G., Newman, J. C., Trubatch, B. N., Yancovitz, M., Paone, D., et al. (2001). Providing hepatitis B vaccination to injection drug users: Referral to health clinics vs on-site vaccination at a syringe exchange program. American Journal of Public Health, 91, 1791–1792.
Diamond, C., Thiede, H., Perdue, T., Secura, G. M., Valleroy, L., Mackellar, D., et al. (2003). Viral hepatitis among young men who have sex with men: Prevalence of infection, risk behaviors, and vaccination. Sexually Transmitted Diseases, 30, 425–432.
Dolezal, C., Carballo-Dieguez, A., Nieves-Rosa, L., & Diaz, F. (2000). Substance use and sexual risk behavior: Understanding their association among four ethnic groups of Latino men who have sex with men. Journal of Substance Abuse, 11, 323–336. doi:S0899-3289(00)00030-4 [pii].
Drumright, L. N., Strathdee, S. A., Little, S. J., Araneta, M. R., Slymen, D. J., Malcarne, V. L., et al. (2007). Unprotected anal intercourse and substance use before and after HIV diagnosis among recently HIV-infected men who have sex with men. Sexually Transmitted Diseases, 34, 401–407. doi:10.1097/01.olq.0000245959.18612.a1.
Eaton, L. A., Kalichman, S. C., Cain, D. N., Cherry, C., Stearns, H. L., Amaral, C. M., et al. (2007). Serosorting sexual partners and risk for HIV among men who have sex with men. American Journal of Preventive Medicine, 33, 479–485. doi:S0749-3797(07)00557-0 [pii]10.1016/j.amepre.2007.08.004.
Fisher, D. G., DeLapp, T. D., Roggenbuck, R. L., & Brause, J. (1992). Substance use and perceived AIDS exposure among homosexual men in Alaska. Psychology of Addictive Behaviors, 6, 168–174.
Fisher, D. G., Reynolds, G. L., Jaffe, A., & Perez, M. J. (2006). Hepatitis and human immunodeficiency virus co-infection among injection drug users in Los Angeles County, California. Journal of Addictive Disease, 25, 25–32.
Fisher, D. G., Reynolds, G. L., Ware, M. R., & Napper, L. E. (2009). Methamphetamine and Viagra use: Relationship to sexual risk behaviors. Archives of Sexual Behavior, [Epub ahead of print]. doi:10.1007/s10508-009-9495-5.
Friedman, M. S., Blake, P. A., Koehler, J. E., Hutwagner, L. C., & Toomey, K. E. (2000). Factors influencing a communitywide campaign to administer hepatitis A vaccine to men who have sex with men. American Journal of Public Health, 90, 1942–1946.
Gallagher, K. M., Denning, P. D., Allen, D. R., Nakashima, A. K., & Sullivan, P. S. (2007). Use of rapid behavioral assessments to determine the prevalence of HIV risk behaviors in high-risk populations. Public Health Reports, 122, 56–62.
Goldbaum, G., Perdue, T., Wolitski, R. J., Rietmeijer, C., Hedrich, A., Wood, R., et al. (1998). Differences in risk behavior and sources of AIDS information among gay, bisexual, and straight-identified men who have sex with men. AIDS and Behavior, 2, 13–21.
Gunn, R. A., Murray, P. J., Ackers, M. L., Hardison, W. G., & Margolis, H. S. (2001). Screening for chronic hepatitis B and C virus infections in an urban sexually transmitted disease clinic: Rationale for integrating services. Sexually Transmitted Diseases, 28, 166–170.
Gunn, R. A., Lee, M. A., Callahan, D. B., Gonzales, P., Murray, P. J., & Margolis, H. S. (2005). Integrating hepatitis, STD, and HIV services into a drug rehabilitation program. American Journal of Preventive Medicine, 29, 27–33.
Gunn, R. A., Lee, M. A., Murray, P. J., Gilchick, R. A., & Margolis, H. S. (2007). Hepatitis B vaccination of men who have sex with men attending an urban STD clinic: Impact of an ongoing vaccination program, 1998–2003. Sexually Transmitted Diseases, 34, 663–668.
Halkitis, P. N., Green, K. A., & Carragher, D. J. (2006). Methamphetamine use, sexual behavior, and HIV seroconversion. [Electronic Electronic; Print]. Journal of Gay & Lesbian Psychotherapy, 10, 95–109.
Hayes-Bautistia, D. E., Hsu, P., Perez, A., Sosa, L., & Gamboa, C. (2005). Hepatitis A: The burden among Latino children in California. Salud Publica de Mexico, 47, 396–401.
Hirshfield, S., Remien, R. H., Humberstone, M., Walavalkar, I., & Chiasson, M. A. (2004). Substance use and high-risk sex among men who have sex with men: A national online study in the USA. AIDS Care, 16, 1036–1047. doi:3XH6GN8CCBK2X4PG [pii]10.1080/09540120412331292525.
Jacobs, R. J., Rosenthal, P., & Meyerhoff, A. S. (2004). Cost effectiveness of hepatitis A/B versus hepatitis B vaccination for US prison inmates. Vaccine, 22, 1241–1248.
Jacobsen, K. H., & Koopman, J. S. (2004). Declining hepatitis A seroprevalence: A global review and analysis. Epidemiology and Infection, 132, 1005–1022.
Jin, F., Prestage, G. P., Pell, C. M., Donovan, B., Van de Ven, P. G., Kippax, S. C., et al. (2004). Hepatitis A and B infection and vaccination in a cohort of homosexual men in Sydney. Sexual Health, 1, 227–237.
Kahn, J. (2002). Preventing hepatitis A and hepatitis B virus infections among men who have sex with men. Clinical Infectious Diseases, 35, 1382–1387. doi:CID020656 [pii].
Kalichman, S. C., Gore-Felton, C., Benotsch, E., Cage, M., & Rompa, D. (2004). Trauma symptoms, sexual behaviors, and substance abuse: Correlates of childhood sexual abuse and HIV risks among men who have sex with men. Journal of Child Sexual Abuse, 13, 1–15.
Kates, S. M., & Belk, R. W. (2001). The meaning of lesbian and Gay Pride day. Journal of Contemporary Ethnography, 30, 392–429.
Kochems, L. M., Mechling, J. P., Nguyen, J. L., Reynolds, G. L., Cloud, M. A., Reutzel, P. M., et al. (2008). Gay Respect with methamphetamine-use assessments: HIV intervention for well-informed gay and other MSM in Long Beach, CA. Paper presented at the 136th Annual Meeting of the American Public Health Association, San Diego, CA.
Levine, H. S. (2003a). Hepatitis A and B vaccination among men who have sex with men. Paper presented at the 37th National Immunization Conference, Chicago, IL. (March)
Levine, H. S. (2003b). Vaccinating men who have sex with men against hepatitis A and hepatitis B: 10 lessons learned from community-based vaccination efforts in the US. Paper presented at the 131st Annual Meeting of the American Public Health Association, Washington, DC. (November)
MacDougall, D. S. (1998). Culture-sensitive campaign targets hepatitis awareness. Journal of the International Association of Physicians in AIDS Care, 4, 38–40.
MacKellar, D. A., Valleroy, L. A., Secura, G. M., McFarland, W., Shehan, D., Ford, W., et al. (2001). Two decades after vaccine license: Hepatitis B immunization and infection among young men who have sex with men. American Journal of Public Health, 91, 965–971.
Mansergh, G., Shouse, R. L., Marks, G., Guzman, R., Rader, M., Buchbinder, S., et al. (2006). Methamphetamine and sildenafil (Viagra) use are linked to unprotected receptive and insertive anal sex, respectively, in a sample of men who have sex with men. Sexually Transmitted Infections, 82, 131–134. doi:82/2/131 [pii]10.1136/sti.2005.017129.
Martinson, J. C., Fisher, D. G., & DeLapp, T. D. (1996). Client disclosure of lesbianism: A challenge for health care providers. Journal of Gay & Lesbian Social Services, 4, 81–94.
Mazick, A., Howitz, M., Rex, S., Jensen, I. P., Weis, N., Katzenstein, T. L., et al. (2005). Hepatitis A outbreak among MSM linked to casual sex and gay saunas in Copenhagen, Denmark. Eurosurveillance, 10, 111–114. doi:536 [pii].
McCusker, J., Hill, E. M., & Mayer, K. H. (1990). Awareness and use of hepatitis B vaccine among homosexual male clients of a Boston community health center. Public Health Reports, 105, 59–64.
Neighbors, K., Oraka, C., Shih, L., & Lurie, P. (1999). Awareness and utilization of the hepatitis B vaccine among young men in the Ann Arbor area who have sex with men. Journal of American College Health, 47, 173–178.
Ostrow, D. G., Vanable, P. A., McKirnan, D. J., & Brown, L. (1999). Hepatitis and HIV risk among drug-using men who have sex with men: Demonstration of Hart's law of inverse access and application to HIV. Journal of the Gay and Lesbian Medical Association, 3, 127–136.
Parsons, J. T., Halkitis, P. N., Wolitski, R. J., & Gomez, C. A. (2003). Correlates of sexual risk behaviors among HIV-positive men who have sex with men. AIDS Education and Prevention, 15, 383–400.
Rabeneck, L., Risser, J. M. H., Murray, H. G. B., McCabe, B. K., Lacke, C. E., & Lucco, L. J. (1993). Failure of providers to vaccinate HIV-infected men against hepatitis B: A missed opportunity. American Journal of Gastroenterology, 88, 2015–2018.
Rhodes, S. D., & Diclemente, R. J. (2003). Psychosocial predictors of hepatitis B vaccination among young African-American gay men in the deep South. Sexually Transmitted Diseases, 30, 449–454.
Saab, S., Lee, C., Shpaner, A., & Ibrahim, A. B. (2005). Seroepidemiology of hepatitis A in patients with chronic liver disease. Journal of Viral Hepatitis, 12, 101–105. doi:10.1111/j.1365-2893.2005.00551.x.
Sansom, S., Rudy, E., Strine, T., & Douglas, W. (2003). Hepatitis A and B vaccination in a sexually transmitted disease clinic for men who have sex with men. Sexually Transmitted Diseases, 30, 685–688. doi:10.1097/01.OLQ.0000079524.04451.4C00007435-200309000-00003 [pii].
Schwarcz, S., Scheer, S., McFarland, W., Katz, M., Valleroy, L., Chen, S., et al. (2007). Prevalence of HIV infection and predictors of high-transmission sexual risk behaviors among men who have sex with men. American Journal of Public Health, 97, 1067–1075. doi:AJPH.2005.072249[pii]10.2105/AJPH.2005.072249.
Seage, G. R., 3rd, Mayer, K. H., Lenderking, W. R., Wold, C., Gross, M., Goldstein, R., et al. (1997). HIV and hepatitis B infection and risk behavior in young gay and bisexual men. Public Health Reports, 112, 158–167.
Semple, S. J., Patterson, T. L., & Grant, I. (2002). Motivations associated with methamphetamine use among HIV + men who have sex with men. Journal of Substance Abuse Treatment, 22, 149–156. doi:S0740547202002234 [pii].
Siconolfi, D. E., Halkitis, P. N., & Rogers, M. E. (2009). Hepatitis vaccination and infection among gay, bisexual, and other men who have sex with men who attend gyms in New York City. American Journal of Men’s Health, 3, 141–149.
Spindler, H. H., Scheer, S., Chen, S. Y., Klausner, J. D., Katz, M. H., Valleroy, L. A., et al. (2007). Viagra, methamphetamine, and HIV risk: Results from a probability sample of MSM, San Francisco. Sexually Transmitted Diseases, 34, 586–591. doi:10.1097/01.olq.0000258339.17325.93.
Springer, A. E., Peters, R. J., Shegog, R., White, D. L., & Kelder, S. H. (2007). Methamphetamine use and sexual risk behaviors in U.S. high school students: Findings from a national risk behavior survey. Prevention Science, 8, 103–113. doi:10.1007/s11121-007-0065-6.
Suro, R., & Singer, A. (2001). Latino growth in metropolitan America: Changing patterns, new locations Survey Series (p. 17). Washington, DC: Center on Urban & Metropolitan Policy.
Sutton, A. J., Gay, N. J., Edmunds, W. J., Andrews, N. J., Hope, V. D., & Gill, O. N. (2005). Modelling the characteristics of the male injecting drug user population in England and Wales. International Journal of Drug Policy, 16, 176–182.
Szmuness, W., Much, I., Prince, A. M., Hoofnagle, J. H., Cherubin, C. E., Harley, E. J., et al. (1975). On the role of sexual behavior in the spread of hepatitis B infection. Annals of Internal Medicine, 83, 489–495.
Trubatch, B. N., Fisher, D. G., Cagle, H. H., & Fenaughty, A. M. (2000). Vaccination strategies for targeted and difficult-to-access groups. American Journal of Public Health, 90, 447.
Viking Software Solutions. (2001). Viking Data Entry+Images (Version 4.2). Tulsa, OK: Phoenix Software International, Inc.
Warwick, Z., Dean, G., & Carter, P. (2007). B safe, B sorted: Results of a hepatitis B vaccination outreach programme. International Journal of STD & AIDS, 18, 335–337.
Washington, T. A., Galai, N., Cohn, S., Celentano, D. D., Vlahov, D., & Strathdee, S. A. (2006). The relationship between self-reported sexual orientation and behavior in a sample of middle-aged male injection drug users. Archives of Sexual Behavior, 35, 67–74.
Wise, M. E., & Sorvillo, F. (2005). Hepatitis A-related mortality in California, 1989–2000: Analysis of multiple cause-coded death data. American Journal of Public Health, 95, 900–905. doi:10.2105/AJPH.2003.035485.
Wohl, A. R., Johnson, D. F., Lu, S., Jordan, W., Beall, G., Currier, J., et al. (2002). HIV risk behaviors among African American men in Los Angeles County who self-identify as heterosexual. Journal of Acquired Immune Deficiency Syndromes, 31, 354–360.
Acknowledgments
The authors would like to acknowledge the assistance of Harold Levine, Linda Radke and the Hep Team Los Angeles with the vaccination effort. The authors would also like to acknowledge the assistance of Jon Mechling, Paul Reutzel, Mike Cloud, John Nuygen, Jacob Tuten, Brent Fremming, Eileen Garcia, Yusuke Kuroki, Michael Ware, and Michele Sguerri in data collection. This research was funded in part by contracts H700939 and H700938 from the Office of AIDS Programs and Policy, County of Los Angeles, CA. Further support was provided by National Research Service Award 1F32DA022902 from the National Institute on Drug Abuse awarded to Dr. Napper.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Storholm, E.D., Fisher, D.G., Reynolds, G.L. et al. Hepatitis Vaccination of Men Who Have Sex with Men at Gay Pride Events. Prev Sci 11, 219–227 (2010). https://doi.org/10.1007/s11121-009-0164-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11121-009-0164-7