Abstract
Purpose
Childhood-onset craniopharyngiomas (CP) are diagnosed due to clinical symptoms (symCP) or incidentally (incCP). We investigated clinical manifestations and outcome in incCPs and symCPs.
Methods
IncCP were discovered in 4 (3 m/1 f) and symCP in 214 (101 m/113 f) CP recruited 2007–2014 in KRANIOPHARYNGEOM 2007. Age, sex, height, body mass index (BMI), tumor volume, degree of resection, pre- and postsurgical hypothalamic involvement/lesions, pituitary function and outcome were compared between both subgroups.
Results
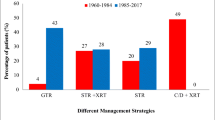
Reasons for imaging in incCP were cerebral palsy, head trauma, nasal obstruction, and tethered-cord syndrome, whereas headache (44%), visual impairment (25%), and growth retardation (17%) lead to imaging in symCP. Tumor volume at diagnosis was smaller in incCP (median 2.39 cm3; range 0.14–4.10 cm3) when compared with symCP (15.86 cm3; 0.002–286.34 cm3). Age, gender, BMI, height, hydrocephalus, tumor location, and hypothalamic involvement at diagnosis of incCP were within the range of these parameters in symCP. Complete resections were achieved more frequently (3/4 patients) in incCP when compared with symCP (20%). Surgical hypothalamic lesions were distributed similar in incCP and symCP. Irradiation was performed only in symCP (33%). No noticeable differences were observed concerning survival rates, endocrine deficiencies, BMI, height, functional capacity and quality of life of the 4 incCP cases when compared with the symCP cohort.
Conclusions
IncCP are rare (1.8%) and characterized by lack of endocrine deficiencies, resulting in normal height and BMI, no hydrocephalus, and smaller tumor volume at diagnosis when compared with symCPs. Outcome of the observed incCP is similar with symCP.
Clinical trial registration number: NCT01272622.





Similar content being viewed by others
References
Martinez-Barbera JP (2015) Molecular and cellular pathogenesis of adamantinomatous craniopharyngioma. Neuropath Appl Neurobiol 41:721–732. https://doi.org/10.1111/nan.12226
Muller HL, Merchant TE, Puget S, Martinez-Barbera JP (2017) New outlook on the diagnosis, treatment and follow-up of childhood-onset craniopharyngioma. Nat Rev Endocrinol 13:299–312. https://doi.org/10.1038/nrendo.2016.217
Goschzik T, Gessi M, Dreschmann V, Gebhardt U, Wang L, Yamaguchi S, Wheeler DA, Lauriola L, Lau CC, Muller HL, Pietsch T (2017) Genomic alterations of adamantinomatous and papillary craniopharyngioma. J Neuropath Exp Neurol 76:126–134. https://doi.org/10.1093/jnen/nlw116
Karavitaki N, Cudlip S, Adams CB, Wass JA (2006) Craniopharyngiomas. Endocr Rev 27:371–397. https://doi.org/10.1210/er.2006-0002
Bogusz A, Muller HL (2018) Childhood-onset craniopharyngioma: latest insights into pathology, diagnostics, treatment and follow-up. Expert Rev Neurother 18(10):793–806. https://doi.org/10.1080/14737175.2018.1528874
Bogusz A, Boekhoff S, Warmuth-Metz M, Calaminus G, Eveslage M, Muller HL (2019) Posterior hypothalamus-sparing surgery improves outcome after childhood craniopharyngioma. Endocr Connect. https://doi.org/10.1530/ec-19-0074
Sterkenburg AS, Hoffmann A, Gebhardt U, Warmuth-Metz M, Daubenbuchel AM, Muller HL (2015) Survival, hypothalamic obesity, and neuropsychological/psychosocial status after childhood-onset craniopharyngioma: newly reported long-term outcomes. Neuro-oncology 17:1029–1038. https://doi.org/10.1093/neuonc/nov044
Muller HL, Bueb K, Bartels U, Roth C, Harz K, Graf N, Korinthenberg R, Bettendorf M, Kuhl J, Gutjahr P, Sorensen N, Calaminus G (2001) Obesity after childhood craniopharyngioma-German multicenter study on pre-operative risk factors and quality of life. Klin Padiatr 213:244–249. https://doi.org/10.1055/s-2001-16855
Muller HL, Gebhardt U, Faldum A, Warmuth-Metz M, Pietsch T, Pohl F, Calaminus G, Sorensen N (2012) Xanthogranuloma, Rathke’s cyst, and childhood craniopharyngioma: results of prospective multinational studies of children and adolescents with rare sellar malformations. J Clin Endocrinol Metab 97:3935–3943. https://doi.org/10.1210/jc.2012-2069
Muller HL, Gebhardt U, Teske C, Faldum A, Zwiener I, Warmuth-Metz M, Pietsch T, Pohl F, Sorensen N, Calaminus G (2011) Post-operative hypothalamic lesions and obesity in childhood craniopharyngioma: results of the multinational prospective trial KRANIOPHARYNGEOM 2000 after 3-year follow-up. Eur J Endocrinol 165:17–24. https://doi.org/10.1530/EJE-11-0158
Fjalldal S, Holmer H, Rylander L, Elfving M, Ekman B, Osterberg K, Erfurth EM (2013) Hypothalamic involvement predicts cognitive performance and psychosocial health in long-term survivors of childhood craniopharyngioma. J Clin Endocrinol Metab 98:3253–3262. https://doi.org/10.1210/jc.2013-2000
Elowe-Gruau E, Beltrand J, Brauner R, Pinto G, Samara-Boustani D, Thalassinos C, Busiah K, Laborde K, Boddaert N, Zerah M, Alapetite C, Grill J, Touraine P, Sainte-Rose C, Polak M, Puget S (2013) Childhood craniopharyngioma: hypothalamus-sparing surgery decreases the risk of obesity. J Clin Endocrinol Metab 98:2376–2382. https://doi.org/10.1210/jc.2012-3928
Puget S, Garnett M, Wray A, Grill J, Habrand JL, Bodaert N, Zerah M, Bezerra M, Renier D, Pierre-Kahn A, Sainte-Rose C (2007) Pediatric craniopharyngiomas: classification and treatment according to the degree of hypothalamic involvement. J Neurosurg 106:3–12. https://doi.org/10.3171/ped.2007.106.1.3
Fjalldal S, Follin C, Gabery S, Sundgren PC, Bjorkman-Burtscher IM, Latt J, Mannfolk P, Nordstrom CH, Rylander L, Ekman B, Cheong R, Palsson A, Petersen A, Erfurth EM (2019) Detailed assessment of hypothalamic damage in craniopharyngioma patients with obesity. Int J Obes 43:533–544. https://doi.org/10.1038/s41366-018-0185-z
Cohen M, Bartels U, Branson H, Kulkarni AV, Hamilton J (2013) Trends in treatment and outcomes of pediatric craniopharyngioma, 1975–2011. Neuro-oncology 15:767–774. https://doi.org/10.1093/neuonc/not026
Müller HL (2015) Craniopharyngioma—pediatric mangement. In: Evans JT, Kenning JT (eds) Craniopharyngiomas comprehensive diagnosis, treatment, and outcome. Academic Press, Oxford, pp 429–458
Hoffmann A, Boekhoff S, Gebhardt U, Sterkenburg AS, Daubenbuchel AM, Eveslage M, Muller HL (2015) History before diagnosis in childhood craniopharyngioma: associations with initial presentation and long-term prognosis. Eur J Endocrinol 173:853–862. https://doi.org/10.1530/EJE-15-0709
Daubenbuchel AM, Hoffmann A, Gebhardt U, Warmuth-Metz M, Sterkenburg AS, Muller HL (2015) Hydrocephalus and hypothalamic involvement in pediatric patients with craniopharyngioma or cysts of Rathke’s pouch: impact on long-term prognosis. Eur J Endocrinol 172:561–569. https://doi.org/10.1530/EJE-14-1029
Muller HL, Emser A, Faldum A, Bruhnken G, Etavard-Gorris N, Gebhardt U, Oeverink R, Kolb R, Sorensen N (2004) Longitudinal study on growth and body mass index before and after diagnosis of childhood craniopharyngioma. J Clin Endocrinol Metab 89:3298–3305. https://doi.org/10.1210/jc.2003-031751
Muller HL, Gebhardt U, Etavard-Gorris N, Korenke E, Warmuth-Metz M, Kolb R, Sorensen N, Calaminus G (2004) Prognosis and sequela in patients with childhood craniopharyngioma—results of HIT-ENDO and update on KRANIOPHARYNGEOM 2000. Klin Padiatr 216:343–348. https://doi.org/10.1055/s-2004-832339
Warmuth-Metz M, Gnekow AK, Muller H, Solymosi L (2004) Differential diagnosis of suprasellar tumors in children. Klin Padiatr 216:323–330. https://doi.org/10.1055/s-2004-832358
Prader A, Largo RH, Molinari L, Issler C (1989) Physical growth of Swiss children from birth to 20 years of age. First Zurich longitudinal study of growth and development. Helv Paediatr Acta 52:1–125
Rolland-Cachera MF, Cole TJ, Sempe M, Tichet J, Rossignol C, Charraud A (1991) Body mass index variations: centiles from birth to 87 years. Eur J Clin Nutr 45:13–21
Calaminus G, Weinspach S, Teske C, Gobel U (2000) Quality of life in children and adolescents with cancer. First results of an evaluation of 49 patients with the PEDQOL questionnaire. Klin Padiatr 212:211–215. https://doi.org/10.1055/s-2000-9679
Eveslage M, Calaminus G, Warmuth-Metz M, Kortmann RD, Pohl F, Timmermann B, Schuhmann MU, Flitsch J, Faldum A, Muller HL (2019) The postoperative quality of life in children and adolescents with craniopharyngioma. Dtsch Arztebl Int 116:321–328. https://doi.org/10.3238/arztebl.2019.0321
Muller HL, Gebhardt U, Faldum A, Emser A, Etavard-Gorris N, Kolb R, Sorensen N (2005) Functional capacity and body mass index in patients with sellar masses—cross-sectional study on 403 patients diagnosed during childhood and adolescence. Childs Nerv Syst 21:539–545. https://doi.org/10.1007/s00381-005-1166-9
Wolff JE, Daumling E, Dirksen A, Dabrock A, Hartmann M, Jurgens H (1996) Munster Heidelberg abilities scale—a measuring instrument for global comparison of illness sequelae. Klin Padiatr 208:294–298. https://doi.org/10.1055/s-2008-1046486
van Iersel L, Brokke KE, Adan RAH, Bulthuis LCM, van den Akker ELT, van Santen HM (2019) Pathophysiology and individualized treatment of hypothalamic obesity following craniopharyngioma and other suprasellar tumors: a systematic review. Endocr Rev 40:193–235. https://doi.org/10.1210/er.2018-00017
Wijnen M, van den Heuvel-Eibrink MM, Janssen J, Catsman-Berrevoets CE, Michiels EMC, van Veelen-Vincent MC, Dallenga AHG, van den Berge JH, van Rij CM, van der Lely AJ, Neggers S (2017) Very long-term sequelae of craniopharyngioma. Eur J Endocrinol 176:755–767. https://doi.org/10.1530/EJE-17-0044
Muller HL, Reichel J, Boekhoff S, Warmuth-Metz M, Eveslage M, Peng J, Flitsch J (2018) Low concordance between surgical and radiological assessment of degree of resection and treatment-related hypothalamic damage: results of KRANIOPHARYNGEOM 2007. Pituitary 21:371–378. https://doi.org/10.1007/s11102-018-0883-5
Muller HL (2019) Management of endocrine disease: childhood-onset craniopharyngioma: state of the art of care in 2018. Eur J Endocrinol 1:2. https://doi.org/10.1530/eje-18-1021
Karavitaki N, Brufani C, Warner JT, Adams CB, Richards P, Ansorge O, Shine B, Turner HE, Wass JA (2005) Craniopharyngiomas in children and adults: systematic analysis of 121 cases with long-term follow-up. Clin Endocrinol 62:397–409. https://doi.org/10.1111/j.1365-2265.2005.02231.x
Rohrer T, Gassmann K, Buchfelder M, Wenzel D, Fahlbusch R, Dorr HG (2002) Clinical symptoms in 35 children and adolescents with craniopharyngeoma at the time of diagnosis. Klin Padiatr 214:285–290. https://doi.org/10.1055/s-2002-33983
Fahlbusch R, Honegger J, Paulus W, Huk W, Buchfelder M (1999) Surgical treatment of craniopharyngiomas: experience with 168 patients. J Neurosurg 90:237–250. https://doi.org/10.3171/jns.1999.90.2.0237
Tan TS, Patel L, Gopal-Kothandapani JS, Ehtisham S, Ikazoboh EC, Hayward R, Aquilina K, Skae M, Thorp N, Pizer B, Didi M, Mallucci C, Blair JC, Gaze MN, Kamaly-Asl I, Spoudeas H, Clayton PE (2017) The neuroendocrine sequelae of paediatric craniopharyngioma: a 40-year meta-data analysis of 185 cases from three UK centres. Eur J Endocrinol 176(3):359–369. https://doi.org/10.1530/EJE-16-0812
Acknowledgements
The authors want to thank all participating colleagues for recruiting patients in KRANIOPHARYNGEOM 2007, and the patients and their parents for participating in this study.
Funding
This study was funded by a grant (HLM; DKS2014.13) of the German Childhood Cancer Foundation, Bonn, Germany.
Author information
Authors and Affiliations
Contributions
SB researched the data and wrote the manuscript. BB did neuroradiological assessment of all imaging. BB is the neuroradiologist, who performs reference-assessment of imaging in all patients recruited in KRANIOPHARYNGEOM 2007. She prepared the imaging data and their presentation and reviewed/edited the manuscript. ME supervised statistical analyses and reviewed/edited the manuscript. PS contributed to the analytical plan and discussion and reviewed/edited the manuscript. HLM initiated and conducted the multicenter trials HIT-Endo and KRANIOPHARYNGEOM 2000/2007, contributed to the analytical plan and discussion and reviewed/edited the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
HLM has received reimbursement of participation fees for scientific meetings and continuing medical education events from the following companies: Ferring, Lilly, Pfizer, Sandoz/Hexal, Novo Nordisk, Ipsen, and Merck Serono. He has received reimbursement of travel expenses from Ipsen and lecture honoraria from Pfizer. The other authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in our study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study KRANIOPHARYNGEOM 2007 (Clinical trial registration number: NCT01272622) was approved by the local standing-committee on ethical practice of the Medizinische Fakultät, Julius-Maximilians-Universität Würzburg, Germany (approval: 94/06), and written parental and/or patient consent was obtained in all cases.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
11102_2019_983_MOESM1_ESM.pdf
Supplementary material 1 Supplemental Figure 1 Parental-assessed health-related quality of life (QoL) as measured by the Pediatric Quality of Life (PEDQOL) [24] questionnaire in patients diagnosed and recruited with incidentaloma craniopharyngioma (incCP) and symptomatic craniopharyngioma (symCP) in the trial KRANIOPHARYNGEOM 2007 between 2007 and 2014. Parental assessments by PEDQOL at the time points 3, 12, and 36 months after CP diagnosis are depicted for the PEDQOL domains autonomy (Suppl. Fig. 1A), emotional stability (Suppl. Fig. 1B), body image (Suppl. Fig. 1C), cognition (Suppl. Fig. 1D), physical function (Suppl. Fig. 1E), social function (friends) (Suppl. Fig. 1F), and social function (family) (Suppl. Fig. 1G). PEDQOL provides negative ratings, i.e. a high score is equivalent to more negative self or parental QoL assessment. Individual PEDQOL scores for incCP are depicted as circle for case 1, triangle for case 3, and square for case 4. PEDQOL scores for sympCP are shown as boxplots. The horizontal line in the middle of the box depicts the median. The top and bottom edges of the box respectively mark the 25th and 75th percentiles. Whiskers indicate the range of values that fall within 1.5 box-lengths. (PDF 363 kb)
Rights and permissions
About this article
Cite this article
Boekhoff, S., Bison, B., Eveslage, M. et al. Craniopharyngiomas presenting as incidentalomas: results of KRANIOPHARYNGEOM 2007. Pituitary 22, 532–541 (2019). https://doi.org/10.1007/s11102-019-00983-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-019-00983-7