Abstract
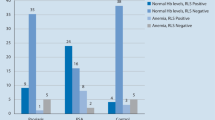
Restless legs syndrome (RLS), a neurological sensory-motor disorder characterized by a compelling urge to move the limbs during the night, is a sleep disturbance that impairs quality of life. Prevalence of RLS and consequences on quality of life were investigated in acromegalic patients. Fifty-six patients (20 men, 55.0 ± 1.6 years), 22 with active acromegaly (group 1) and 34 with controlled disease (group 2), and 95 controls (35 men, 52.9 ± 1.1 years) were evaluated by a structured sleep interview concerning insomnia, circadian sleep disorders and excessive diurnal sleepiness (EDS). The Epworth Sleepiness Scale (ESS) questionnaire was administered to those reporting EDS. Patients were investigated by RLS diagnostic interview and International Restless Leg Syndrome—Rating Scale (IRLS-RS). Quality of life was investigated by AcroQoL questionnaire. RLS was diagnosed in 21% of acromegalics and in 4% of controls (P < 0.002). Prevalence of RLS and mean IRLS-RS was higher in group 1 than in group 2 (P < 0.05). Prevalence of insomnia (P < 0.0002) and of EDS (P < 0.05) and mean ESS score (P < 0.01) were higher in RLS-positive than in RLS-free acromegalics. Video-PSG showed that mean sleep latency (P < 0.01), micro-arousal index (P < 0.05) and wakefulness after sleep onset (P < 0.01) were higher, whereas sleep efficiency (P < 0.01) was lower, in RLS-positive than in RLS-free patients. Global and physical AcroQoL scores were significantly lower in RLS-positive than in RLS-free acromegalics (P < 0.01 and P < 0.001, respectively). Prevalence and severity of RLS is increased in patients with active acromegaly and impacts negatively on their physical performances, dramatically impairing quality of life.

Similar content being viewed by others
References
Rowles SV, Prieto L, Badia X, Shalet SM, Webb SM, Trainer PJ (2005) Quality of Life (QOL) in patients with acromegaly is severely impaired: use of a novel measure of QOL: acromegaly quality of life questionnaire. J Clin Endocrinol Metab 90:3337–3341
Pantanetti P, Sonino N, Arnaldi G, Boscaro M (2002) Self image and quality of life in acromegaly. Pituitary 5:17–19
Webb SM, Badia X, Surinach NL, SpanishAcroQolStudy Group (2006) Validity and clinical applicability of the acromegaly quality of life questionnaire, AcroQoL: a 6-month prospective study. Eur J Endocrinol 155:269–277
Biermasz NR, Pereira AM, Smit JW, Romijn JA, Roelfsema F (2005) Morbidity after long-term remission for acromegaly: persisting joint-related complaints cause reduced quality of life. J Clin Endocrinol Metab 90:2731–2739
Barrière G, Cazalets JR, Bioulac B, Tison F, Ghorayeb I (2005) The restless legs syndrome. Prog Neurobiol 77:139–165
Walters AS, Rye DB (2009) Review of the relationship of restless legs syndrome and periodic limbs movements in sleep to hypertension, heart disease and stroke. Sleep 32:589–597
Walters AS, Rye DB (2010) Evidence continue to mount on the relationship of restless legs syndrome/periodic limb movements in sleep to hypertension, cardiovascular disease and stroke. Sleep 33(3):287
Johns MW (1993) Daytime sleepiness, snoring, and obstructive sleep apnea. The epworth sleepiness scale. Chest 103:30–36
Allen RP, Picchietti D, Hening WA, Trenkwalder C, Walters AS, Montplaisi J, Restless Legs Syndrome Diagnosis and Epidemiology Workshop at the National Institutes of Health; International Restless Legs Syndrome Study Group (2003) Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med 4:101–119
Walters AS, LeBrocq C, Dhar A, Hening W, Rosen R, Allen RP, Trenkwalder C, International Restless Legs Syndrome Study Group (2003) Validation of the international restless legs syndrome study group rating scale for restless legs syndrome. Sleep Med 4:121–132
Webb SM, Prieto L, Badia X, Albareda M, Catalá M, Gaztambide S, Lucas T, Páramo C, Picó A, Lucas A, Halperin I, Obiols G, Astorga R (2002) Acromegaly quality of life questionnaire (ACROQOL) a new health-related quality of life questionnaire for patients with acromegaly: development and psychometric properties. Clin Endocrinol 57:251–258
Allen RP, Walters AS, Montplaisir J, Hening W, Myers A, Bell TJ, Ferini-Strambi L (2005) Restless legs syndrome prevalence and impact: REST general population study. Arch Int Med 165:1286–1292
Machtey I (2001) Epidemiology of restless legs syndrome. Arch Int Med 161:483–484
Sevim S, Dogu O, Camdeviren H, Bugdayci R, Sasmaz T, Kaleagasi H, Aral M, Helvaci I (2003) Unexpectedly low prevalence and unusual characteristics of RLS in Mersin, Turkey. Neurology 61:1562–1569
Bjorvatn B, Leissner L, Ulfberg J, Gyring J, Karlsborg M, Regeur L, Skeidsvoll H, Nordhus IH, Pallesen S (2005) Prevalence, severity and risk factors of restless legs syndrome in the general adult population in two Scandinavian countries. Sleep Med 6:307–331
Möller C, Wetter TC, Köster J, Stiasny-Kolster K (2010) Differential diagnosis of unpleasant sensations in the legs: prevalence of restless legs syndrome in a primary care population. Sleep Med 11(2):161–166
Taylor-Gjevre RM, Gjevre JA, Skomro R, Nair B (2009) Restless legs syndrome in a rheumatoid arthritis patient cohort. J Clin Rheumatol 15(1):12–15
Colao A, Cannavò S, Marzullo P, Pivonello R, Squadrito S, Vallone G, Almoto B, Bichisao E, Trimarchi F, Lombardi G (2003) Twelve months of treatment with octreotide-LAR reduces joint thickness in acromegaly. Eur J Endocrinol 148(1):31–38
Ekbom K (1945) Restless legs: a clinical study. Acta Med Scand 158:1–123
Chabli A, Michaud M, Montplaisir J (2000) Periodic arm movements in patients with the restless legs syndrome. Eur Neurol 44:133–138
Gamaldo C, Benbrook AR, Allen RP, Oguntimein O, Earley CJ (2009) Evaluating daytime alertness in individuals with restless legs syndrome (RLS) compared to sleep restricted controls. Sleep Med 10:134–138
Pearson VE, Allen RP, Dean T, Gamaldo CE, Lesage SR, Earley CJ (2006) Cognitive deficits associated with restless legs syndrome (RLS). Sleep Med 7:25–30
Holdaway IM, Rajasoorya RC, Gamble GD (2004) Factors influencing mortality in acromegaly. J Clin Endocrinol Metab 89:667–674
Clemens S, Rye D, Hochman S (2006) Restless legs syndrome: revisiting the dopamine hypothesis from the spinal cord perspective. Neurology 67(1):125–130
Caylak E (2009) The genetics of sleep disorders in humans: narcolepsy, restless legs syndrome, and obstructive sleep apnea syndrome. Am J Med Gen 149A:2612–2626
Silber MH, Richardson JW (2003) Multiple blood donations associated with iron deficiency in patients with restless legs syndrome. Mayo Clin Proc 78:52–54
Kotagal S, Silber MH (2004) Childhood-onset restless legs syndrome. Ann Neurol 56:803–807
Högl B, Kiechl S, Willeit J, Saletu M, Frauscher B, Seppi K, Müller J, Rungger G, Gasperi A, Wenning G, Poewe W (2005) Restless legs syndrome: a community-based study of prevalence, severity, and risk factors. Neurology 64:1920–1924
Trenkwalder C, Hening WA, Montagna P, Oertel WH, Allen RP, Walters AS, Costa J, Stiasny-Kolster K, Sampaio C (2008) Treatment of restless legs syndrome: an evidence-based review and implications for clinical practice. Mov Disord 23:2267–2302
Acknowledgments
We thank Prof. Susan M. Webb for kindly providing AcroQoL questionnaires in Italian.
Author information
Authors and Affiliations
Corresponding author
Additional information
S. Cannavò and R. Condurso contributed equally to the study.
Rights and permissions
About this article
Cite this article
Cannavò, S., Condurso, R., Ragonese, M. et al. Increased prevalence of restless legs syndrome in patients with acromegaly and effects on quality of life assessed by Acro-QoL. Pituitary 14, 328–334 (2011). https://doi.org/10.1007/s11102-011-0298-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-011-0298-z