Abstract
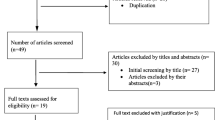
Background Residents in long-term care facilities take many medications concomitantly, including antibacterials, which increases the risk of drug–drug interactions. Objectives The aims of the study were to investigate the prevalence of severe potential interactions between antibacterials and other medications in Slovenian long-term care facilities and to compare the performance of two different drug–drug interaction checkers in these settings. Setting Residents in long-term care facilities in Slovenia. Method A point-prevalence study was conducted from April 2016 to June 2016. Residents’ characteristics, antibacterial treatment, and concomitant medications were obtained from their medical charts. Potential drug–drug interactions were determined using Lexicomp Online™ 3.0.2 and the online Drugs.com Drug Interactions Checker. The study only included potential drug–drug interactions categorized as type MA (major interactions) by the Drugs.com checker and as type X (should be avoided) by Lexicomp Online™. The study calculated the differences in the number of type X and MA potential drug–drug interactions between different antibacterial classes and between the two drug–drug interactions checkers. Main outcome measure Number of medications per patient, number of potential drug–drug interactions with antibacterial, and differences between two drug–drug interactions checkers. Results Eighty (68.4%) of Slovenian general long-term care facilities with 13,032 residents responded to the invitation. 317 (2.4%) of the residents received antibacterial treatment and 212 residents were included in the analysis. On average, they received 10.9 medications (SD = 3.9). Antibacterials were involved in 24.1% type MA potential drug–drug interactions and 26.4% type X potential drug–drug interactions. A significant difference in the total number of potential drug–drug interaction between the two checkers was found for all antibacterials, co-trimoxazole and fluoroquinolones (p < 0.005). Type X and MA potential drug–drug interactions were more common with fluoroquinolones than with beta-lactams or co-trimoxazole (p < 0.005). Conclusion Potential interactions between antibacterials, especially fluoroquinolones and other drugs, were common in long-term care facility residents treated with antibacterials. Differences in the number of potential drug–drug interactions between the two checkers indicate that if available the use of several sources of information is recommended in clinical practice. The results call for a collaborative approach to address the risks of drug–drug interactions.
Similar content being viewed by others
References
Andrew MK, Purcell CA, Marshall EG. Polypharmacy and use of potentially inappropriate medications in long-term care facilities: does coordinated primary care make a difference? Int J Pharm Pract. 2017;1:11. https://doi.org/10.1111/ijpp.12397.
Janssens B, Petrovic M, Jacquet W. Medication use and its potential impact on the oral health status of LTCF residents in flanders (Belgium). J Am Med Dir Assoc. 2017;18:809.e1–8.
Hajjar ER, Cafiero AC, Hanlon JT. Polypharmacy in elderly patients. Am J Geriatr Pharmacother. 2007;5:345–51.
Gallagher PF, Barry PJ, Ryan C, Hartigan I, O’Mahony D. Inappropriate prescribing in an acutely ill population of elderly patients as determined by Beers’ Criteria. Age Ageing. 2008;37:96–101.
Dechanont S, Maphanta S, Butthum B, Kongkaew C. Hospital admissions/visits associated with drug–drug interactions: a systematic review and meta-analysis. Pharmacoepidemiol Drug Saf. 2014;23:489–97.
Buul LW, van Steen JT, van der Veenhuizen RB, Achterberg WP, Schellevis FG, Essink RT, et al. Antibiotic use and resistance in long term care facilities. J Am Med Dir Assoc. 2012;13:568.e1–13.
Fleming A, Browne J, Byrne S. The effect of interventions to reduce potentially inappropriate antibiotic prescribing in long-term care facilities: a systematic review of randomised controlled trials. Drugs Aging. 2013;30:401–8.
Stuart RL, Wilson J, Bellaard-Smith E, Brown R, Wright L, Vandergraaf S, et al. Antibiotic use and misuse in residential aged care facilities. Intern Med J. 2012;42:1145–9.
Drinka PJ, Crnich CJ, Nace DA. An antibiotic prescription induces resistance at the individual level more than the group level. J Am Med Dir Assoc. 2013;14:707–8.
Malani AN, Brennan BM, Collins CD, Finks J, Pogue JM, Kaye KS. Antimicrobial stewardship practices in michigan long-term care facilities. Infect Control Hosp Epidemiol. 2016;37:236–7.
Beovic B, Plesnicar BK, Potocan M, Zmitek A, Winkler V, Celan SS, et al. Antibiotic prescribing in psychiatric hospitals and interactions between antibiotics and psychotropic drugs: a prospective observational study. Infect Control Hosp Epidemiol. 2016;37:233–5.
Hines LE, Murphy JE. Potentially harmful drug–drug interactions in the elderly: a review. Am J Geriatr Pharmacother. 2011;9:364–77.
The Association of Social Institutions in Slovenia. (2016) Highlights from analyzes. http://www.ssz-slo.si/wp-content/uploads/Poudarki-iz-komulativnega-stati%C4%8Dnega-poro%C4%8Dila-za-leto-2016.pdf. Accessed 10 Oct 2017.
European Centre for Disease Prevention and Control (ECDC) Point prevalence survey of healthcare-associated infections and antimicrobial use in European long-term care facilities. April–May 2013. Stockholm: ECDC. 2014. https://ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/healthcare-associated-infections-point-prevalence-survey-long-term-care-facilities-2013.pdf. Accessed 10 Oct 2017.
Stepan D, Ušaj L, Petek Šter M, Smolinger Galun M, Smole H, Beović B. Antimicrobial prescribing in long-term care facilities: a nationwide point-prevalence study, Slovenia 2016. Euro Surveill. 2018;1:11. https://doi.org/10.2807/1560-7917.ES.2018.23.46.1800100.
Lexicomp-Clinical Drug Information. 2018. https://online.lexi.com/lco/action/home. Accessed 10 Oct 2017.
Drug Interactions Checker. 2018. https://www.drugs.com/drug_interactions.html. Accessed 10 Oct 2017.
Søraas IA, Staurset HB, Slørdal L, Spigset O. Drug–drug interactions in nursing home patients. Tidsskr Nor Laegeforen. 2014;134:1041–6.
Björkman IK, Fastbom J, Schmidt IK, Bernsten CB, Pharmaceutical Care of the Elderly in Europe Research (PEER) Group. Drug–drug interactions in the elderly. Ann Pharmacother. 2002;36:1675–81.
Alves-Conceição V, Silva DTD, Santana VL, Santos EGD, Santos LMC, Lyra DP Jr. Evaluation of pharmacotherapy complexity in residents of long-term care facilities: a cross-sectional descriptive study. BMC Pharmacol Toxicol. 2017;18:59.
Muhič N, Mrhar A, Brvar M. Comparative analysis of three drug–drug interaction screening systems against probable clinically relevant drug–drug interactions: a prospective cohort study. Eur J Clin Pharmacol. 2017;73:875–82.
Bonkat G, Bartoletti RR, Bruyère F, Cai T, Geerlings SE, Köves B, et al. Urological infections. Eur Assoc Urol. 2019. https://uroweb.org/guideline/urological-infections/#1. Accessed 15 May 2019.
Lim WS, Baudouin SV, George RC, Hill AT, Jamieson C, Le Jeune I, et al. BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax. 2009;64(Suppl 3):iii1–55.
European Medicines Agency. Disabling and potentially permanent side effects lead to suspension or restrictions of quinolone and fluoroquinolone antibiotics. European Medicines Agency. 2019. https://www.ema.europa.eu/en/medicines/human/referrals/quinolone-fluoroquinolone-containing-medicinal-products. Accessed 15 May 2019.
Holt S, Schimedel S, Thürmann AP. Potentially inappropriate medications in the elderly: the PRISCUS list. Dtsch Arztebl Int. 2010;107:543–51.
Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (screening tool of older person’s prescriptions) and START (screening tool to alert doctors to right treatment) consensus validation. Int J Clin Pharmacol Ther. 2008;46:72–83.
Gorup EC, Šter MP. Number of medications or number of diseases: what influences underprescribing? Eur J Clin Pharmacol. 2017;73:1673–9.
Gorup EC, Šter MP, Klančič D. Polypharmacy and inappropriate drug prescribing in elderly nursing home residents. Zdrav vestn. 2009;78:231–40.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Štuhec, M., Potočin, I., Stepan, D. et al. Potential drug interactions with antibacterials in long-term care facilities analyzed by two interaction checkers. Int J Clin Pharm 41, 932–938 (2019). https://doi.org/10.1007/s11096-019-00855-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-019-00855-x