Abstract
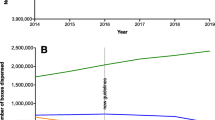
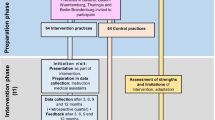
Background Fluoroquinolones are frequently prescribed for non complicated urinary tract infection treatments and have a negative ecological impact. We aimed to substitute them by antibiotics with narrower activity spectrum in order to preserve fluoroquinolone activity in complicated hospital infections. Objective To assess the impact of a multi-modal approach that combines the dispatching of antibiotic prescription guidelines and voluntary attendance at educational sessions on general practitioners’ (GP) antibiotic prescription habits. Setting This study was led in Franche-Comté, a French eastern region, where GPs were given a guideline recommending a restricted use of fluoroquinolones for urinary tract infections. Method Segmented regression analysis of interrupted time series was used to assess changes in antibiotic prescription. Main outcome measure: The antibiotic prescription data of nitrofurantoin, fosfomycin-trometamol and fluoroquinolones for women aged 15–65 years were obtained from the regional agency of health insurance. Results Twenty months after intervention, the number of nitrofurantoin and fosfomycintrometamol prescriptions increased by 36.8% (95% CI: 30.6–42.2) and 28.5% (95% CI: 22.9–35.4), respectively, while that of norfloxacin decreased by 9.1% (95% CI: −15.3 to −3.5). Conclusion This study suggests that the dispatch of the guideline on urinary tract infection had a moderate impact on antibiotic prescriptions.

Similar content being viewed by others
References
Lautenbach E, Fishman NO, Bilker WB, Castiglioni A, Metlay JP, Edelstein PH, et al. Risk factors for fluoroquinolone resistance in nosocomial Escherichia coli and Klebsiella pneumoniae infections. Arch Intern Med. 2002;162(21):2469–77.
Zervos MJ, Hershberger E, Nicolau DP, Ritchie DJ, Blackner LK, Coyle EA, et al. Relationship between fluoroquinolone use and changes in susceptibility to fluoroquinolones of selected pathogens in 10 United States teaching hospitals, 1991–2000. Clin Infect Dis. 2003;37(12):1643–8.
Charbonneau P, Parienti JJ, Thibon P, Ramakers M, Daubin C, du Cheyron D, et al. Fluoroquinolone use and methicillin-resistant Staphylococcus aureus isolation rates in hospitalized patients: a quasi experimental study. Clin Infect Dis. 2006;42(6):778–84.
Muller A, Mauny F, Talon D, Donnan PT, Harbarth S, Bertrand X. Effect of individual- and group-level antibiotic exposure on MRSA isolation: a multilevel analysis. J Antimicrob Chemother. 2006;58(4):878–81.
Stone SP, Cooper BS, Kibbler CC, Cookson BD, Roberts JA, Medley GF, et al. The ORION statement: guidelines for transparent reporting of outbreak reports and intervention studies of nosocomial infection. Lancet Infect Dis. 2007;7(4):282–8.
World Health Organization (WHO). Anatomic therapeutic chemical (ATC) classification index with defined daily doses (DDDs). WHO, Oslo, Norway; 2001.
Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299–309.
Ansari F, Gray K, Nathwani D, Phillips G, Ogston S, Ramsay C, et al. Outcomes of an intervention to improve hospital antibiotic prescribing: interrupted time series with segmented regression analysis. J Antimicrob Chemother. 2003;52(5):842–8.
Mahamat A, MacKenzie FM, Brooker K, Monnet DL, Daures JP, Gould IM. Impact of infection control interventions and antibiotic use on hospital MRSA: a multivariate interrupted time-series analysis. Int J Antimicrob Agents. 2007;30(2):169–76.
Apisarnthanarak A, Pinitchai U, Thongphubeth K, Yuekyen C, Warren DK, Zack JE, et al. Effectiveness of an educational program to reduce ventilator-associated pneumonia in a tertiary care center in Thailand: a 4-year study. Clin Infect Dis. 2007;45(6):704–11.
Matowe L, Ramsay CR, Grimshaw JM, Gilbert FJ, Macleod MJ, Needham G. Effects of mailed dissemination of the Royal College of Radiologists’guidelines on general practitioner referrals for radiography: a time series analysis. Clin Radiol. 2002;57(7):575–8.
J Leroy, I Patry, C Faure, E Ariskina, JP Gaume, T Henon, et al. [Regional audit on fluoroquinolones usage in the hospital and the community: Are these antibiotics over-used?]. Pathol Biol (Paris), 2011;59(5):103–7.
Chomarat M. Resistance of bacteria in urinary tract infections. Int J Antimicrob Agents. 2000;16(4):483–7.
Peterson LR. Squeezing the antibiotic balloon: the impact of antimicrobial classes on emerging resistance. Clin Microbiol Infect. 2005;11(Suppl 5):4–16.
Cals JW, Butler CC, Hopstaken RM, Hood K, Dinant GJ. Effect of point of care testing for C reactive protein and training in communication skills on antibiotic use in lower respiratory tract infections: cluster randomised trial. Bmj. 2009;338:b1374.
Francis NA, Butler CC, Hood K, Simpson S, Wood F, Nuttall J. Effect of using an interactive booklet about childhood respiratory tract infections in primary care consultations on reconsulting and antibiotic prescribing: a cluster randomised controlled trial. Bmj. 2009;339:b2885.
CA McNulty, GM Lasseter, A Charlett, A Lovering, R Howell-Jones, A Macgowan, et al. Does laboratory antibiotic susceptibility reporting influence primary care prescribing in urinary tract infection and other infections? J Antimicrob Chemother. 2011;66(6):1396–1404.
Jiang HJ, Lagasse RS, Ciccone K, Jakubowski MS, Kitain EM. Factors influencing hospital implementation of acute pain management practice guidelines. J Clin Anesth. 2001;13(4):268–76.
Christakis DA, Rivara FP. Pediatricians’awareness of and attitudes about four clinical practice guidelines. Pediatrics. 1998;101(5):825–30.
Costanza ME, Stoddard AM, Zapka JG, Gaw VP, Barth R. Physician compliance with mammography guidelines: barriers and enhancers. J Am Board Fam Pract. 1992;5(2):143–52.
Acknowledgments
We thank all the GPs of Franche-Comte, who enabled the use of their prescription data.
Funding
No specific funding.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Slekovec, C., Leroy, J., Vernaz-Hegi, N. et al. Impact of a region wide antimicrobial stewardship guideline on urinary tract infection prescription patterns. Int J Clin Pharm 34, 325–329 (2012). https://doi.org/10.1007/s11096-012-9606-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-012-9606-6