Abstract
Objective
Hydrocephalus is usually resolved by diverting cerebrospinal fluid through a surgically implanted intra-ventricular catheter (shunt). The aim of this study was to characterize vancomycin pharmacokinetic (PK) parameters and optimal dosage in shunted patients under vancomycin treatment.
Setting
Intensive Care and Neurosurgical Units. University Hospital.
Methods
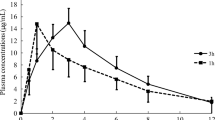
Retrospective data of vancomycin blood concentrations, demographics and biochemical parameters, from a Therapeutic Drug Monitoring (TDM) program, in ventricle-external shunted patients (Group A) and controls (Group B) were collected. In all subjects, several blood samples at steady state conditions were drawn. Individual PK parameters such as drug clearance (CL) and volume of distribution (V) were estimated by using an one-compartmental PK model and later, dosage regimens were individually adjusted by Bayesian analysis. The obtained CL and V mean ± standard deviation were compared between both groups (A versus B). Vancomycin dosage regimens between both groups were also compared.
Main outcome measures
Patients demographics, clinical records, creatinine clearance by Cockcroft-Gault, vancomycin blood levels, vancomycin pK parameters and optimal initial IV vancomycin dosage.
Results
Forty-five patients were included in the study: 15 patients in group A and 30 subjects in group B. Significant differences between CLA and CLB means were observed, while not between VA and VB. In shunted patients, the required vancomycin daily dose to reach target concentrations was significantly higher than the dose needed in the control group (49.25 ± 12.28 mg/kg/day vs. 31.74 ± 6.70 mg/kg/day; P < 0.0005).
Conclusions
Greater vancomycin clearance was found in our shunted patients, thus they required higher vancomycin daily doses compared to the control group. Consequently, vancomycin TDM in shunted patients should be advisable in order to guarantee antibiotic blood concentrations within the recommended therapeutic range.
Similar content being viewed by others
References
Farreras P, Rozman C. Medicina interna, vol II, XIV Ed. Harcourt, S.A., Madrid. ISBN 84-8174-359-3. 2000;1645, 1709–10
Ammirati M, Raimondi AJ. Cerebrospinal fluid shunt infections in children. A study on the relationship between the etiology of hydrocephalus, age at the time of shunt placement and infection rate. Child's Nerv Sys 1987;3:106–9
Bayston R. Hydrocephalus shunt infections. J Antimicrob Chemother 1994; 34(Suppl. A):75–84
Choux M, Genitori L, Lang D, Lena G. Shunt implantation: reducing the incidence of shunt infection. J Neurosurg 1992; 77:875–80
Ellenbogen RG, Goldmann DA, Winston KR. Group B Streptococcal infections of the central nervous system in infants with myelomeningocele. Surg Neurol 1988;29:237–42
Vinchon M, Vallee L, Prin L, Desreumaux P, Dhellemmes P. Cerebro-spinal fluid eosinophilia in shunt infections. Neuropediatrics 1992;23:235–40
Bafeltowska JJ, Buszman E, Mandat KM, Hawranek JK. Therapeutic vancomycin monitoring in children with hydrocephalus during treatment of shunt infections. Surg Neurol 2004 Aug;62(2):142
Bourgeois M, Sainte-Rose C, Cinalli G, Maixner W, Malucci C, Zera M, et al. Epilepsy in children with shunted hydrocephalus. J Neurosurg 1999 Feb;90(2):274–81
Bennett DR, editor. Drug evaluations subscription. Chicago, IL: American Medical Association, Winter 1992
Sheiner LB, Beal SL. Some suggestions for measuring predictive performance. J Pharmacokinet Biopharmaceut 1981; 9:503–12
Fernandez de Gatta MM, Fruns I, Calvo MV, Lanao JM, Dominguez-Gil A. Influence of pharmacokinetic model on vancomycin peak concentration targets. Ther Drug Monit 1996 Apr;18(2):145–8
Odenholt-Tornqvist I, Löwdin E, Cars C. Postantibiotic sub-MIC effects of vancomycin, roxithromycin, sparfloxacin, and amikacin. Antimicrob Agents Chemother. 1992 sep;36(9):1852–8
Soy D, Badia JR, Torres A. Antibiotic Dosage Regimens in Respiratory Tract Infections in the pharmacokinetic/pharmacodynamic era. Curr Respiratory Med Rev 2006;2:89–97
Healy DP, Polk RE, Garson ML, Rock DT, Comstock TJ, Comparison of steady-state pharmacokinetics of two dosage regimens of vancomycin in normal volunteers. Antimicrob Agents Chemother 1987 Mar;31(3):393–7
Pryka RD, Rodvold KA, Garrison M, Rotschafer JC. Individualizing vancomycin dosage regimes: one- versus two-compartment Bayesian models. Ther Drug Monit 1989; 11:450–4
Albrecht LM, Rybak MJ, Boike SC, Pancorbo S. Comparison of serum sampling methods for determining vancomycin dosage regimes. Ther Drug Monit 1988;10:85–90
Walson PD. Therapeutic drug monitoring in special populations. Clin Chem 1998;44(2):415–9
Evans WE, Schentag JJ, Jusko WJ. Applied pharmacokinetics: principles of therapeutic drug monitoring, 3rd ed. Spokane, Applied Therapeutics, Inc. 1992
Reetze-Bonorden P, Bohler J, Keller E. Drug dosage in patients during continuous renal replacement therapy. Pharmacokinetic and therapeutic considerations. Clin Pharmacokinet 1993 May;24(5):362–79
DelDot ME, Lipman J, Tett SE. Vancomycin pharmacokinetics in critically ill patients receiving continuous venovenous haemodiafiltration. Br J Clin Pharmacol 2004 Sep;58(3):259–68
Rodvold KA, Blum RA, Fischer JH, Zokufa HZ, Rotschafer JC, Crossley KB, et al. Vancomycin pharmacokinetics in patients with various degrees of renal function. Antimicrob Agents Chemother 1988 Jun;32(6):848–52
PachoreK RE, Wood F. Vancomycin half-life in a patient with hepatic and renal dysfunction. Clin Pharm 1991; 10:297–300
Soto J, Alsar MJ, Sacristan JA. Initial dosage of vancomycin in neutropenic hematologic patients. Sangre (Barc) 1992 Jun; 37(3):181–4
Tomás R, Soy D, García-Peláez M, Cardenete J, Quintana E, Mangues MA. High dose requirements of vancomycin in multiple trauma adult patients in intensive care units [Abstract]. Pharm World Sci 2000;22(1):28 [A47]
Pea F, Porreca L, Baraldo M, Furlanut M. High vancomycin dosage regimens required by intensive care unit patients cotreated with drugs to improve haemodynamics following cardiac surgical procedures. J Antimicrob Chemother 2000 Mar;45(3):329–35
Rybak MJ, Albrecht LM, Berman JR, Warbasse LH, Svensson CK. Vancomycin pharmacokinetics in burn patients and intravenous drug abusers. Antimicrob Agents Chemother 1990 May;34(5):792–5
Conil JM, Favarel H, Laguerre J, Brouchet A, Chabanon G, Cazal L, et al. Continuous administration of vancomycin in patients with severe burns. Presse Med 1994 Nov 5; 23(34):1554–8
Acknowledgements
The authors would like to thank Núria Miserachs, Laura Gratacós, Patricia Domínguez and Marina Rovira at the Pharmacy Service of Hospital Clínic de Barcelona for their collaboration in the vancomycin TDM process.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pujal, M., Soy, D., Codina, C. et al. Are higher vancomycin doses needed in venticle-external shunted patients?. Pharm World Sci 28, 215–221 (2006). https://doi.org/10.1007/s11096-006-9037-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-006-9037-3