Abstract
Purpose
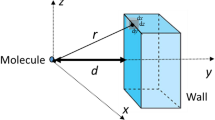
Performance of a transdermal delivery system (TDS) can be affected by exposure to elevated temperature, which can lead to unintended safety issues. This study investigated TDS and skin temperatures and their relationship in vivo, characterized the effective thermal resistance of skin, and identified the in vitro diffusion cell conditions that would correlate with in vivo observations.
Methods
Experiments were performed in humans and in Franz diffusion cells with human cadaver skin to record skin and TDS temperatures at room temperature and with exposure to a heat flux. Skin temperatures were regulated with two methods: a heating lamp in vivo and in vitro, or thermostatic control of the receiver chamber in vitro.
Results
In vivo basal skin temperatures beneath TDS at different anatomical sites were not statistically different. The maximum tolerable skin surface temperature was approximately 42–43°C in vivo. The temperature difference between skin surface and TDS surface increased with increasing temperature, or with increasing TDS thermal resistance in vivo and in vitro.
Conclusions
Based on the effective thermal resistance of skin in vivo and in vitro, the heating lamp method is an adequate in vitro method. However, the in vitro-in vivo correlation of temperature could be affected by the thermal boundary layer in the receiver chamber.






Similar content being viewed by others
Abbreviations
- FDA:
-
U.S. Food and Drug Administration
- HPLC:
-
High performance liquid chromatography
- IVIVC:
-
In vitro-in vivo correlation
- IVPT:
-
In vitro permeation test
- PBS:
-
Phosphate buffered saline
- PID:
-
Proportional integral derivative
- q skin :
-
Heat flux across the skin
- q TDS :
-
Heat flux across the TDS
- R ABL :
-
Aqueous boundary layer thermal resistance
- R s :
-
Skin thermal resistance in vivo
- R sts :
-
Split-thickness skin thermal resistances in vitro
- R TDS :
-
TDS thermal resistance
- RLD:
-
Reference listed drug
- T derm :
-
Temperature of the tissue around blood circulation under the skin
- T receiver :
-
Receiver solution temperature in diffusion cell
- T skin/receiver :
-
Temperature at the skin/receiver interface
- T TDS :
-
TDS surface temperature
- T TDS/skin :
-
Skin surface temperature under TDS
- TDS:
-
Transdermal delivery systems
- TDS-1:
-
1-layer model TDS
- TDS-5:
-
5-layer model TDS
References
Ashburn MA, Ogden LL, Zhang J, Love G, Basta SV. The pharmacokinetics of transdermal fentanyl delivered with and without controlled heat. J Pain. 2003;4(6):291–7.
Barkve TF, Langseth-Manrique K, Bredesen JE, Gjesdal K. Increased uptake of transdermal glyceryl trinitrate during physical exercise and during high ambient temperature. Am Heart J. 1986;112(3):537–41.
Bur A, Joukhadar C, Klein N. Herkner, Mitulovic G, Schmid R, Agneter E, Muller M, Brunner M. Effect of exercise on transdermal nicotine release in healthy habitual smokers. Int J Clin Pharmacol Ther. 2005;43(5):239–43.
Fujimura A, Sasaki M, Harada K, Kumagai Y, Ohashi K, Ebihara A. Influences of bathing and hot weather on the pharmacokinetics of a new transdermal clonidine, M-5041T. J Clin Pharmacol. 1996;36(10):892–6.
Gjesdal K, Klemsdal TO, Rykke EO, Bredesen JE. Transdermal nitrate therapy: bioavailability during exercise increases transiently after the daily change of patch. Br J Clin Pharmacol. 1991;31(5):560–2.
Klemsdal TO, Gjesdal K, Bredesen JE. Heating and cooling of the nitroglycerin patch application area modify the plasma level of nitroglycerin. Eur J Clin Pharmacol. 1992;43(6):625–8.
Klemsdal TO, Gjesdal K, Zahlsen K. Physical exercise increases plasma concentrations of nicotine during treatment with a nicotine patch. Br J Clin Pharmacol. 1995;39(6):677–9.
Moore KT, Sathyan G, Richarz U, Natarajan J, Vandenbossche J. Randomized 5-treatment crossover study to assess the effects of external heat on serum fentanyl concentrations during treatment with transdermal fentanyl systems. J Clin Pharmacol. 2012;52(8):1174–85.
Petersen KK, Rousing ML, Jensen C, Arendt-Nielsen L, Gazerani P. Effect of local controlled heat on transdermal delivery of nicotine. Int J Physiol Pathophysiol Pharmacol. 2011;3(3):236–42.
Shomaker TS, Zhang J, Ashburn MA. A pilot study assessing the impact of heat on the transdermal delivery of testosterone. J Clin Pharmacol. 2001;41(6):677–82.
Prodduturi S, Sadrieh N, Wokovich AM, Doub WH, Westenberger BJ, Buhse L. Transdermal delivery of fentanyl from matrix and reservoir systems: effect of heat and compromised skin. J Pharm Sci. 2010;99(5):2357–66.
Hao J, Ghosh P, Li SK, Newman B, Kasting GB, Raney SG. Heat effects on drug delivery across human skin. Expert Opin Drug Deliv. 2016;13(5):755–68.
Franz TJ, Lehman PA, Raney SG. Use of excised human skin to assess the bioequivalence of topical products. Skin Pharmacol Physiol. 2009;22(5):276–86.
Lehman PA, Raney SG, Franz TJ. Percutaneous absorption in man: in vitro-in vivo correlation. Skin Pharmacol Physiol. 2011;24(4):224–30.
Gazerani P, Arendt-Nielsen L. Cutaneous vasomotor reactions in response to controlled heat applied on various body regions of healthy humans: evaluation of time course and application parameters. Int J Physiol Pathophysiol Pharmacol. 2011;3(3):202–9.
Kellogg DL Jr, Liu Y, Kosiba IF, O’Donnell D. Role of nitric oxide in the vascular effects of local warming of the skin in humans. J Appl Physiol (1985). 1999;86(4):1185–90.
Pergola PE, Kellogg DL Jr, Johnson JM, Kosiba WA, Solomon DE. Role of sympathetic nerves in the vascular effects of local temperature in human forearm skin. Am J Phys. 1993;265(3 Pt 2):H785–92.
Miller MA, Kasting G. A measurement of the unstirred aqueous boundary layer in a Franz diffusion cell. Pharm Dev Technol. 2012;17(6):705–11.
Bird RB, Stewart WE, Lightfoot EN. Transport phenomena. New York: Wiley; 1960.
McCabe WL, Smith JC. Unit operations of chemical engineering. New York: McGraw Hill; 1976.
Skelly JP, Shah VP, Maibach HI, Guy RH, Wester RC, Flynn G, Yacobi A. FDA and AAPS report of the workshop on principles and practices of in vitro percutaneous penetration studies: relevance to bioavailability and bioequivalence. Pharm Res. 1987;4(3):265–7.
Aliouat Bellia S, Saidane A, Hamou A, Benzohra M, Saiter JM. Transmission line matrix modelling of thermal injuries to skin. Burns. 2008;34:688–97.
Becker S, Kuznetsov A. Thermal damage reduction associated with in vivo skin electroporation: a numerical investigation justifying aggressive pre-cooling. Int J Heat Mass Transf. 2007;50:105–16.
Agache P, Humbert P. Measuring the skin. New York: Springer; 2004.
Cohen ML. Measurement of the thermal properties of human skin. A review. J Invest Dermatol. 1977;69(3):333–8.
Sandby-Moller J, Poulsen T, Wulf HC. Epidermal thickness at different body sites: relationship to age, gender, pigmentation, blood content, skin type, and smoking habits. Acta Derm Venereol. 2003;83:410–13.
Flynn GL. Physicochemical determinants of skin absorption. In: Gerrity TR, Henry CJ, editors. Principles of route-to-route extrapolation for risk assessment. New York: Elsevier; 1990. p. 93–127.
Li SK, Suh W, Parikh HH, Ghanem A-H, Mehta SC, Peck KD, Higuchi WI. Lag time data for characterizing the pore pathway of intact and chemically pretreated human epidermal membrane. Int J Pharm. 1998;170(1):93–108.
Ibrahim R, Kasting GB. Improved method for determining partition and diffusion coefficients in human dermis. J Pharm Sci. 2010;99(12):4928–39.
Mitragotri S. Temperature dependence of skin permeability to hydrophilic and hydrophobic solutes. J Pharm Sci. 2007;96(7):1832–9.
Scheuplein RJ. Analysis of permeability data for the case of parallel diffusion pathways. Biophys J. 1966;6(1):1–17.
Peck KD, Ghanem AH, Higuchi WI. The effect of temperature upon the permeation of polar and ionic solutes through human epidermal membrane. J Pharm Sci. 1995;84(8):975–82.
ACKNOWLEDGMENTS AND DISCLOSURES
The authors thank Drs. Arjang Talattof and Elena Rantou for helpful discussion and Craig Dixon at ThermTest Inc. for performing the thermal resistance analysis of the nicotine TDS. Funding for this work was made possible, in part, by the FDA through grant U01FD004942. In response to funding opportunity announcement RFA-FD-13-015, separate research projects were awarded in parallel to the University of Cincinnati and the University of Maryland, and each institution was requested by the FDA to perform independent research with the same drug products under comparable study conditions in a manner coordinated by the FDA. The views expressed in this manuscript do not reflect the official policies of the FDA or the U.S. Department of Health and Human Services; nor does any mention of trade names, commercial practices, or organization imply endorsement by the United States Government. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, Q., Murawsky, M., LaCount, T. et al. Characterization of Temperature Profiles in Skin and Transdermal Delivery System When Exposed to Temperature Gradients In Vivo and In Vitro . Pharm Res 34, 1491–1504 (2017). https://doi.org/10.1007/s11095-017-2171-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-017-2171-x