ABSTRACT
Purpose
Experimental Blood–Brain Barrier (BBB) permeability models for drug molecules are expensive and time-consuming. As alternative methods, several traditional Quantitative Structure-Activity Relationship (QSAR) models have been developed previously. In this study, we aimed to improve the predictivity of traditional QSAR BBB permeability models by employing relevant public bio-assay data in the modeling process.
Methods
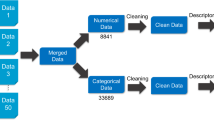
We compiled a BBB permeability database consisting of 439 unique compounds from various resources. The database was split into a modeling set of 341 compounds and a validation set of 98 compounds. Consensus QSAR modeling workflow was employed on the modeling set to develop various QSAR models. A five-fold cross-validation approach was used to validate the developed models, and the resulting models were used to predict the external validation set compounds. Furthermore, we used previously published membrane transporter models to generate relevant transporter profiles for target compounds. The transporter profiles were used as additional biological descriptors to develop hybrid QSAR BBB models.
Results
The consensus QSAR models have R2 = 0.638 for five-fold cross-validation and R2 = 0.504 for external validation. The consensus model developed by pooling chemical and transporter descriptors showed better predictivity (R2 = 0.646 for five-fold cross-validation and R2 = 0.526 for external validation). Moreover, several external bio-assays that correlate with BBB permeability were identified using our automatic profiling tool.
Conclusions
The BBB permeability models developed in this study can be useful for early evaluation of new compounds (e.g., new drug candidates). The combination of chemical and biological descriptors shows a promising direction to improve the current traditional QSAR models.





Similar content being viewed by others
Abbreviations
- 5-HT:
-
5-hydroxytryptamine
- AD:
-
Applicability domain
- ADME:
-
Absorption, distribution, metabolism, and excretion
- AID:
-
PubChem bio-assay identifier
- ALDH1A1:
-
Aldehyde dehydrogenase 1 family, member A1
- AR:
-
Androgen receptor
- ASBT:
-
Apical sodium-dependent bile acid transporter
- BBB:
-
Blood–brain barrier
- BSEP:
-
Bile salt export pump
- CAMP:
-
Cyclic adenosine monophosphate
- CID:
-
PubChem compound identifier
- CNS:
-
Central nervous system
- ER-Alpha:
-
Estrogen receptor alpha
- HITs:
-
Human intestinal transporters
- HTS:
-
High throughput screening
- kNN:
-
k-nearest neighbor
- logBB:
-
Logarithm of brain-plasma concentration ratio at steady-state
- MAE:
-
Mean absolute error
- MCT:
-
Monocarboxylic acid transporters
- MDR:
-
Multidrug resistance
- MDR1:
-
Multidrug resistance protein 1
- MOE:
-
Molecular operating environment software
- MRP1:
-
Multidrug resistance-associated protein 1
- MRP3:
-
Multidrug resistance-associated protein 3
- MRP4:
-
Multidrug resistance-associated protein 4
- MRP5:
-
Multidrug resistance-associated protein 5
- OATPs:
-
Organic anion transporting polypeptides
- PCA:
-
Principle component analysis
- QSAR:
-
Quantitative structure-activity relationship
- RF:
-
Random forest
- SVM:
-
Support vector machine
REFERENCES
Abbott NJ. Blood–brain barrier structure and function and the challenges for CNS drug delivery. J Inherit Metab Dis. 2013;36(3):437–49.
Alavijeh MS, Chishty M, Qaiser MZ, Palmer AM. Drug metabolism and pharmacokinetics, the blood–brain barrier, and central nervous system drug discovery. NeuroRx. 2005;2(4):554–71.
Andersen HR, Nielsen JB, Grandjean P. Toxicologic evidence of developmental neurotoxicity of environmental chemicals. Toxicology. 2000;144(1–3):121–7.
Maggiora GM. On outliers and activity cliffs–why QSAR often disappoints. J Chem Inf Model Am Chem Soc. 2006;46(4):1535.
Bajorath J, Peltason L, Wawer M, Guha R, Lajiness MS, Van Drie JH. Navigating structure-activity landscapes. Drug Discov Today. 2009;14(13–14):698–705.
Zhu H, Zhang J, Kim MT, Boison A, Sedykh A, Moran K. Big data in chemical toxicity research: the use of high-throughput screening assays to identify potential toxicants. Chem Res Toxicol Am Chem Soc. 2014;27(10):1643–51.
Joó F, Rakonczay Z, Wollemann M. cAMP-Mediated regulation of the permeability in the brain capillaries. Experientia. 1975;31(5):582–4.
Sedykh A, Fourches D, Duan J, Hucke O, Garneau M, Zhu H, et al. Human intestinal transporter database: QSAR modeling and virtual profiling of drug uptake, efflux and interactions. Pharm Res. 2013;30(4):996–1007.
Zhang J, Hsieh J-H, Zhu H. Profiling animal toxicants by automatically mining public bioassay data: a big data approach for computational toxicology. Homayouni R, editor. PLoS One Public Libr Sci. 2014 Jan;9(6):e99863.
Muehlbacher M, Spitzer GM, Liedl KR, Kornhuber J. Qualitative prediction of blood–brain barrier permeability on a large and refined dataset. J Comput Aided Mol Des. 2011;25(12):1095–106.
Vilar S, Chakrabarti M, Costanzi S. Prediction of passive blood–brain partitioning: straightforward and effective classification models based on in silico derived physicochemical descriptors. J Mol Graph Model. 2010;28(8):899–903.
Hou TJ, Xu XJ. ADME evaluation in drug discovery. 3. Modeling blood–brain barrier partitioning using simple molecular descriptors. J Chem Inf Comput Sci. 2003;43(6):2137–52.
Abraham MH, Ibrahim A, Zhao Y, Acree WE. A data base for partition of volatile organic compounds and drugs from blood/plasma/serum to brain, and an LFER analysis of the data. J Pharm Sci. 2006;95(10):2091–100.
Mensch J, Jaroskova L, Sanderson W, Melis A, Mackie C, Verreck G, et al. Application of PAMPA-models to predict BBB permeability including efflux ratio, plasma protein binding and physicochemical parameters. Int J Pharm. 2010;395(1–2):182–97.
Ooms F, Weber P, Carrupt P-A, Testa B. A simple model to predict blood–brain barrier permeation from 3D molecular fields. Biochim Biophys Acta Mol Basis Dis. 2002;1587(2–3):118–25.
Breiman L. Random forests. Mach Learn. Kluwer Academic Publishers; 2001 Oct 1;45(1):5–32.
Vapnik V. The nature of statistical learning theory. Springer Science & Business Media; 2000.
Dalgaard P. Introductory Statistics with R. Springer Science & Business Media; 2008.
Zheng W, Tropsha A. Novel variable selection quantitative structure–property relationship approach based on the k-nearest-neighbor principle. J Chem Inf Model Am Chem Soc. 2000;40(1):185–94.
Walker T, Grulke CM, Pozefsky D, Tropsha A. Chembench: a cheminformatics workbench. Bioinformatics. 2010;26(23):3000–1.
Solimeo R, Zhang J, Kim M, Sedykh A, Zhu H. Predicting chemical ocular toxicity using a combinatorial QSAR approach. Chem Res Toxicol Am Chem Soc. 2012;25(12):2763–9.
Zhang L, Zhu H, Oprea TI, Golbraikh A, Tropsha A. QSAR modeling of the blood–brain barrier permeability for diverse organic compounds. Pharm Res. 2008;25(8):1902–14.
Kim MT, Sedykh A, Chakravarti SK, Saiakhov RD, Zhu H. Critical evaluation of human oral bioavailability for pharmaceutical drugs by using various cheminformatics approaches. Pharm Res. 2014;31(4):1002–14.
Tropsha A, Golbraikh A. Predictive QSAR modeling workflow, model applicability domains, and virtual screening. Curr Pharm Des. Bentham Science Publishers; 2007 Dec 1;13(34):3494–504.
Golbraikh A, Shen M, Xiao Z, Xiao Y-D, Lee K-H, Tropsha A. Rational selection of training and test sets for the development of validated QSAR models. J Comput Aided Mol Des. Kluwer Academic Publishers; 2003 Feb 1;17(2–4):241–53.
Walters HC, Craddock AL, Fusegawa H, Willingham MC, Dawson PA. Expression, transport properties, and chromosomal location of organic anion transporter subtype 3. Am J Physiol Gastrointest Liver Physiol. 2000;279(6):G1188–200.
Hagenbuch B, Dawson P. The sodium bile salt cotransport family SLC10. Pflugers Arch. 2004;447(5):566–70.
Kusuhara H, Sugiyama Y. Role of transporters in the tissue-selective distribution and elimination of drugs: transporters in the liver, small intestine, brain and kidney. J Control Release. 2002;78(1–3):43–54.
Gerloff T. The sister of P-glycoprotein represents the canalicular bile salt export pump of mammalian liver. J Biol Chem. 1998;273(16):10046–50.
Tsuji A, Tamai I. Carrier-mediated or specialized transport of drugs across the blood–brain barrier. Adv Drug Deliv Rev. 1999;36(2–3):277–90.
Demeule M, Shedid D, Beaulieu E, Del Maestro RF, Moghrabi A, Ghosn PB, et al. Expression of multidrug-resistance P-glycoprotein (MDR1) in human brain tumors. Int J Cancer. 2001;93(1):62–6.
Huai-Yun H, Secrest DT, Mark KS, Carney D, Brandquist C, Elmquist WF, et al. Expression of multidrug resistance-associated protein (MRP) in brain microvessel endothelial cells. Biochem Biophys Res Commun. 1998;243(3):816–20.
Roberts LM, Black DS, Raman C, Woodford K, Zhou M, Haggerty JE, et al. Subcellular localization of transporters along the rat blood–brain barrier and blood-cerebral-spinal fluid barrier by in vivo biotinylation. Neuroscience. 2008;155(2):423–38.
Mayer U, Wagenaar E, Beijnen JH, Smit JW, Meijer DKF, Asperen J, et al. Substantial excretion of digoxin via the intestinal mucosa and prevention of long-term digoxin accumulation in the brain by the mdrla P-glycoprotein. Br J Pharmacol. 1996;119(5):1038–44.
Zhu H, Martin TM, Ye L, Sedykh A, Young DM, Tropsha A. Quantitative structure-activity relationship modeling of rat acute toxicity by oral exposure. Chem Res Toxicol Am Chem Soc. 2009;22(12):1913–21.
Zhu H, Tropsha A, Fourches D, Varnek A, Papa E, Gramatica P, et al. Combinatorial QSAR modeling of chemical toxicants tested against Tetrahymena pyriformis. J Chem Inf Model. 2008;48(4):766–84.
Sedykh A, Zhu H, Tang H, Zhang L, Richard A, Rusyn I, et al. Use of in vitro HTS-derived concentration-response data as biological descriptors improves the accuracy of QSAR models of in vivo toxicity. Environ Health Perspect. 2011;119(3):364–70.
Zhu H, Rusyn I, Richard A, Tropsha A. Use of cell viability assay data improves the prediction accuracy of conventional quantitative structure-activity relationship models of animal carcinogenicity. Environ Health Perspect. 2008;116(4):506–13.
Hammarlund-Udenaes M, Fridén M, Syvänen S, Gupta A. On the rate and extent of drug delivery to the brain. Pharm Res. 2008;25(8):1737–50.
Ohtsuki S, Tomi M, Hata T, Nagai Y, Hori S, Mori S, et al. Dominant expression of androgen receptors and their functional regulation of organic anion transporter 3 in rat brain capillary endothelial cells; comparison of gene expression between the blood–brain and -retinal barriers. J Cell Physiol. 2005;204(3):896–900.
Sharma HS, Dey PK. Impairment of blood–brain barrier (BBB) in rat by immobilization stress: role of serotonin (5-HT). Indian J Physiol Pharmacol. 1981;25(2):111–22.
Banks W, Kastin A, Komaki G, Arimura A. Passage of pituitary adenylate cyclase activating polypeptide1-27 and pituitary adenylate cyclase activating polypeptide1-38 across the blood- brain barrier. J Pharmacol Exp Ther. 1993;267(2):690–6.
Cai C, Omwancha J, Hsieh C-L, Shemshedini L. Androgen induces expression of the multidrug resistance protein gene MRP4 in prostate cancer cells. Prostate Cancer Prostatic Dis. 2007;10(1):39–45.
ACKNOWLEDGMENTS AND DISCLOSURES
Research reported in this publication was supported, in part, by the National Institute of Environmental Health Sciences of the National Institutes of Health under Award Number R15ES023148 and the Colgate-Palmolive Grant for Alternative Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Figure S1
(DOCX 1647 kb)
Table SI
(XLSX 11 kb)
Table SII
(XLSX 30 kb)
Table SIII
(XLSX 24 kb)
Rights and permissions
About this article
Cite this article
Wang, W., Kim, M.T., Sedykh, A. et al. Developing Enhanced Blood–Brain Barrier Permeability Models: Integrating External Bio-Assay Data in QSAR Modeling. Pharm Res 32, 3055–3065 (2015). https://doi.org/10.1007/s11095-015-1687-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-015-1687-1