ABSTRACT
Purpose
To prepare acylated exenatide analogues and investigate their biological properties for guiding the development of PLGA formulations of exenatide.
Methods
The acylated exenatide analogues were prepared by reaction with glycolic acid (GA), one constitutional unit of PLGA, and characterized by HPLC-MS/MS and Circular Dichroism (CD). The pharmacokinetic properties and anti-diabetic activities were studied in SD rats and db/db mice, respectively.
Results
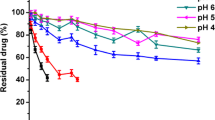
Structural characterizations of the acylated products showed that one to four glycolic acids (GAs) were connected to the primary amine groups of exenatide, and there was a conversion of α-helix to β-sheet to some extent. Pharmacokinetic studies in SD rats revealed that acylated exenatides had a similar Tmax with that of the prototype drug, whereas the Cmax and the AUC values of the adducts were significantly decreased. Biological activity tests demonstrated that exenatide and acylated exenatide analogues had similar in vivo antidiabetic activities in terms of controlling blood glucose concentration, HbA1c level, body weight and food intake.
Conclusions
These findings suggest that GA conjugated exenatide had no influence on the peptide efficacy, therefore it’s not necessary to inhibit exenatide acylation in PLGA formulations during the peptide release process.






Similar content being viewed by others
Abbreviations
- CD:
-
Circular dichroism
- CDI:
-
N, N′-carbonyldiimidazole
- DMSO:
-
Dimethyl sulfoxide
- GA:
-
Glycolic acid
- LCA:
-
Lithocholic acid
- LUA:
-
Lauric acid
- PLGA:
-
Poly(lactide-co-glycolide)
- SD:
-
Sprague–Dawley
- T2DM:
-
Type 2 diabetes mellitus
References
Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–53.
Jaime A, Davidson MD. Advances in therapy for type 2 diabetes: GLP-1 receptor agonists and DPP-4 inhibitors. Cleve Clin J Med. 2009;76:S28–78.
Lovshin JA, Drucker DJ. Incretin-based therapies for type 2 diabetes mellitus. Nat Rev Endocrinol. 2009;5:262–9.
Kulasa KM. The current status of exenatide once weekly. Clin Med Insights Ther. 2011;3:221–32.
Drucker DJ, Nauck MA. The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet. 2006;368:1696–705.
Drucker DJ, Buse JB, Taylor K, Kendall DM, Trautmann M, Zhuang D, et al. Exenatide once weekly versus twice daily for the treatment of type 2 diabetes: a randomised, open-label, non-inferiority study. Lancet. 2008;372:1240–50.
Kwak HH, Shim WS, Hwang S, Son MK, Kim YJ, Kim TH, et al. Pharmacokinetics and efficacy of a biweekly dosage formulation of exenatide in zucker diabetic fatty (ZDF) rats. Pharm Res. 2009;26:2504–12.
Lucke A, Kiermaier J, Göpferich A. Peptide acylation in poly(ahydroxy esters). Pharm Res. 2002;19:175–81.
Murty SB, Thanoo BC, Wei Q, DeLuca PP. Impurity formation studies with peptide-loaded polymeric microspheres Part I. In vivo evaluation. Int J Pharm. 2005;297:50–61.
Lucke A, Kiermaier J, Göpferich A. Acylation of peptides by lactic acid solutions. Eur J Pharm Biopharm. 2003;55:27–33.
Ahn JH, Park EJ, Lee HS, Lee KC, Na DH. Reversible blocking of amino groups of octreotide for the inhibition of formation of acylated peptide impurities in poly(lactide-co-glycolide) delivery systems. AAPS PharmSciTech. 2011;12:1220–6.
Houchin ML, Neuenswander SA, Topp EM. Effect of excipients on PLGA film degradation and the stability of an incorporated peptide. J Control Release. 2007;117:413–20.
Park E, Tak TH, Na DH, Lee KC. Effect of PEGylation on stability of peptide in poly(lactide-co-glycolide) microspheres. Arch Pharm Res. 2010;33:1111–6.
Na DH, DeLuca PP. PEGylation of octreotide: I. Separation of positional isomers and stability against acylation by poly(D, L-lactide-co-glycolide). Pharm Res. 2005;22:736–42.
Ghassemi AH, van Steenbergen MJ, Barendregt A, Talsma H, Kok RJ, van Nostrum CF, et al. Controlled release of octreotide and assessment of peptide acylation from poly(D, L-lactide-co-hydroxymethyl glycolide) compared to PLGA microspheres. Pharm Res. 2012;29:110–20.
Sophocleous AM, Zhang Y, Schwendeman SP. A new class of inhibitors of peptide sorption and acylation in PLGA. J Control Release. 2009;137:179–84.
Zhang Y, Sophocleous AM, Schwendeman SP. Inhibition of peptide acylation in PLGA microspheres with water-soluble divalent cationic salts. Pharm Res. 2009;26:1986–94.
Zhang Y, Schwendeman SP. Minimizing acylation of peptides in PLGA microspheres. J Control Release. 2012;162:119–26.
Na DH, Lee JE, Jang SW, Lee KC. Formation of acylated growth hormone-releasing peptide-6 by poly(lactide-co-glycolide) and its biological activity. AAPS PharmSciTech. 2007;8:E1–5.
Kidwai SA, Ansari AA, Salahuddin A. Effect of succinylation (3-carboxy- propionylation) on the conformation and immunological activity of ovalbumin. Biochem J. 1976;155:171–80.
Qasim MA, Salahuddin A. Changes in conformation and immunological activity of ovalbumin during its modification with different acid anhydrides. Biochim Biophys Acta. 1978;536:50–63.
Murase S, Yumoto N, Petukhov MG, Yoshikawa S. Acylation of the alpha-amino group in neuropeptide Y(12–36) increases binding affinity for the Y2 receptor. J Biochem Tokyo. 1996;119:37–41.
Schwendeman SP, Costantino HR, Gupta RK, Tobio M, Chang AC, Alonso MJ, et al. Strategies for stabilising tetanus toxoid towards the development of a single-dose tetanus vaccine. Dev Biol Stand. 1996;87:293–306.
Liang RC, Li X, Shi YN, Wang AP, Sun KX, Liu WH, et al. Effect of water on exenatide acylation in poly(lactide-co-glycolide) microspheres. Int J Pharm. 2013;454:344–53.
Liang RC, Zhang RY, Li X, Wang AP, Chen DQ, Sun KX, et al. Stability of Exenatide in poly(D, L-lactide-co-glycolide) solutions: a simplified investigation on the peptide degradation by the polymer. Eur J Pharm Sci. 2013;50:502–10.
Hudson FM, Andersen NH. Exenatide: NMR/CD evaluation of the medium dependence of conformation and aggregation state. Pept Sci. 2004;76:298–308.
Doyle BL, Pollo MJ, Pekar AH, Roy ML, Thomas BA, Brader ML. Biophysical signatures of noncovalent aggregates formed by a glucagonlike peptide-1 analog: a prototypical example of biopharmaceutical aggregation. J Pharm Sci. 2005;94:2749–63.
Riedel MJ, Lee CWK, Kieffer TJ. Engineered glucagon-like peptide-1-producing hepatocytes lower plasma glucose levels in mice. Am J Physiol Endocrinol Metab. 2009;296:E936–44.
Willard FS, Sloop KW. Physiology and emerging biochemistry of the glucagon-like peptide-1 receptor. Exp Diabetes Res. 2012;2012:12. doi:10.1155/2012/470851.
Chae SY, Choi YG, Son S, Jung SY, Lee DS, Lee KC. The fatty acid conjugated exendin-4 analogs for type 2 antidiabetic therapeutics. J Control Release. 2010;144:10–6.
Chae SY, Jin CH, Shin JH, Son S, Kim TH, Lee S, et al. Biochemical, pharmaceutical and therapeutic properties of long-acting lithocholic acid derivatized exendin-4 analogs. J Control Release. 2010;142:206–13.
Hoare SRJ. Mechanisms of peptide and nonpeptide ligand binding to Class B G-protein-coupled receptors. DDT. 2005;10:417–27.
López de Maturana R, Donnelly D. The glucagon-like peptide-1 receptor binding site for the N-terminus of GLP-1 requires polarity at Asp198 rather than negative charge. FEBS Lett. 2002;530:244–8.
Murty SB, Na DH, Thanoo BC, DeLuca PP. Impurity formation studies with peptide-loaded polymeric microspheres Part II. In vitro evaluation. Int J Pharm. 2005;297:62–72.
Houchin ML, Topp EM. Chemical degradation of peptides and proteins in PLGA: a review of reactions and mechanisms. J Pharm Sci. 2008;97:2395–404.
Giteau A, Venier-Julienne MC, Aubert-Pouessel A, Benoit JP. How to achieve sustained and complete protein release from PLGA-based microparticles? Int J Pharm. 2008;350:14–26.
Van de Weert M, Hennink WE, Jiskoot W. Protein instability in poly(lactic-co-glycolic acid) microparticles. Pharm Res. 2000;17:1159–67.
Acknowledgments and Disclosures
The authors would like to express thanks to Dr. Dan Donnelly (Programme Leader for Pharmacology, School of Biomedical Sciences, Faculty of Biological Sciences, University of Leeds) for his assistance and supply of the helical wheel of exenatide for adaption in this work.
This study was supported by grants from the National Basic Research Program of China (No. 2012CB724003), the National Key Technology Research and Development Program of China (No. 2012BAK25B03) and the National Science and Technology Major Project of the Ministry of Science and Technology of China (No. 2013ZX09402201).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liang, R., Li, X., Zhang, R. et al. Acylation of Exenatide by Glycolic Acid and its Anti-Diabetic Activities in db/db Mice. Pharm Res 31, 1958–1966 (2014). https://doi.org/10.1007/s11095-014-1298-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-014-1298-2