ABSTRACT
Purpose
Previous research has led to the recognition of a cGMP signaling pathway governing drug transport. This study is to investigate whether inhibitors of phosphodiesterase type 5 (PDE5), which increase intracellular cGMP levels, modulate the cytotoxicity and uptake of anti-cancer drugs in cancer cells.
Methods
The experiments were conducted with and without PDE5 inhibitors: dipyridamole, vardenafil, and/or sildenafil. The cytotoxicity of doxorubicin, cisplatin and oxaliplatin was determined in multiple cancer cell lines derived from different tissues. The cellular uptake of structurally diverse compounds was further examined in lung cancer cells with and without various endocytotic inhibitors. The tumor accumulation and the anti-tumor effect of trastuzumab were examined in a lung cancer xenograft mouse model.
Results
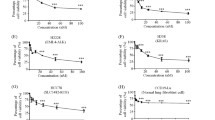
Dipyridamole could modulate the cytotoxicity of doxorubicin, cisplatin, and oxaliplatin in cancer cells. Particularly, PDE5 inhibitors increased cellular uptake of structurally diverse compounds into lung cancer cells both in vitro and in vivo. The effect of vardenafil on drug uptake could be blocked by endocytotic inhibitors. The growth of lung cancer xenograft in nude mice was significantly suppressed by addition of vardenafil to trastuzumab treatment.
Conclusion
PDE5 inhibitors may increase the efficacy of anti-cancer drugs by increasing endocytosis-mediated cellular drug uptake, and thus serve as adjuvant therapy for certain cancers such as lung cancer.








Similar content being viewed by others
REFERENCEs
Packer RJ, Krailo M, Mehta M, Warren K, Allen J, Jakacki R, et al. A Phase I study of concurrent RMP-7 and carboplatin with radiation therapy for children with newly diagnosed brainstem gliomas. Cancer. 2005;104:1968–74.
Packer RJ, Krailo M, Mehta M, Warren K, Allen J, Jakacki R, et al. Phase 1 study of concurrent RMP-7 and carboplatin with radiotherapy for children with newly diagnosed brainstem gliomas. Cancer. 2005;104:1281–7.
Matsukado K, Sugita M, Black KL. Intracarotid low dose bradykinin infusion selectively increases tumor permeability through activation of bradykinin B2 receptors in malignant gliomas. Brain Res. 1998;792:10–5.
Emerich DF, Dean RL, Snodgrass P, Lafreniere D, Agostino M, Wiens T, et al. Bradykinin modulation of tumor vasculature: II. activation of nitric oxide and phospholipase A2/prostaglandin signaling pathways synergistically modifies vascular physiology and morphology to enhance delivery of chemotherapeutic agents to tumors. J Pharmacol Exp Ther. 2001;296:632–41.
Nakano S, Matsukado K, Black KL. Increased brain tumor microvessel permeability after intracarotid bradykinin infusion is mediated by nitric oxide. Cancer Res. 1996;56:4027–31.
Yin D, Wang X, Konda BM, Ong JM, Hu J, Sacapano MR, et al. Increase in brain tumor permeability in glioma-bearing rats with nitric oxide donors. Clin Cancer Res. 2008;14:4002–9.
Black KL, Yin D, Ong JM, Hu J, Konda BM, Wang X, et al. PDE5 inhibitors enhance tumor permeability and efficacy of chemotherapy in a rat brain tumor model. Brain Res. 2008;1230:290–302.
Hu J, Ljubimova JY, Inoue S, Konda B, Patil R, Ding H, et al. Phosphodiesterase type 5 inhibitors increase Herceptin transport and treatment efficacy in mouse metastatic brain tumor models. PLoS One. 2010;5:e10108.
Ningaraj NS, Rao M, Hashizume K, Asotra K, Black KL. Regulation of blood–brain tumor barrier permeability by calcium-activated potassium channels. J Pharmacol Exp Ther. 2002;301:838–51.
Ningaraj NS, Rao MK, Black KL. Adenosine 5′-triphosphate-sensitive potassium channel-mediated blood–brain tumor barrier permeability increase in a rat brain tumor model. Cancer Res. 2003;63:8899–911.
Hu J, Yuan X, Ko MK, Yin D, Sacapano MR, Wang X, et al. Calcium-activated potassium channels mediated blood–brain tumor barrier opening in a rat metastatic brain tumor model. Mol Cancer. 2007;6:22.
Emerich DF, Snodgrass P, Dean RL, Lafreniere D, Agostino M, Wiens T, et al. Bradykinin modulation of tumor vasculature: I. Activation of B2 receptors increases delivery of chemotherapeutic agents into solid peripheral tumors, enhancing their efficacy. J Pharmacol Exp Ther. 2001;296:623–31.
Inamuraand T, Black KL. Bradykinin selectively opens blood-tumor barrier in experimental brain tumors. J Cereb Blood Flow Metab. 1994;14:862–70.
Black KL, Yin D, Konda BM, Wang X, Hu J, Ko MK, et al. Different effects of KCa and KATP agonists on brain tumor permeability between syngeneic and allogeneic rat models. Brain Res. 2008;1227:198–206.
Corbinand JD, Francis SH. Cyclic GMP phosphodiesterase-5: target of sildenafil. J Biol Chem. 1999;274:13729–32.
Corbin JD, Beasley A, Blount MA, Francis SH. Vardenafil: structural basis for higher potency over sildenafil in inhibiting cGMP-specific phosphodiesterase-5 (PDE5). Neurochem Int. 2004;45:859–63.
Ziegler JW, Ivy DD, Fox JJ, Kinsella JP, Clarke WR, Abman SH. Dipyridamole, a cGMP phosphodiesterase inhibitor, causes pulmonary vasodilation in the ovine fetus. Am J Physiol. 1995;269:H473–9.
Barberi-Heyob M, Griffon G, Merlin JL, Weber B. Sequence-dependent growth-inhibitory effects of the in vitro combination of fluorouracil, cisplatin, and dipyridamole. Cancer Chemother Pharmacol. 1993;33:163–70.
Rodrigues M, Barbosa Jr F, Perussi JR. Dipyridamole increases the cytotoxicity of cisplatin in human larynx cancer cells in vitro. Braz J Med Biol Res. 2004;37:591–9.
Jekunen A, Vick J, Sanga R, Chan TC, Howell SB. Synergism between dipyridamole and cisplatin in human ovarian carcinoma cells in vitro. Cancer Res. 1992;52:3566–71.
Gerlierand D, Thomasset N. Use of MTT colorimetric assay to measure cell activation. J Immunol Methods. 1986;94:57–63.
Nam HY, Kwon SM, Chung H, Lee SY, Kwon SH, Jeon H, et al. Cellular uptake mechanism and intracellular fate of hydrophobically modified glycol chitosan nanoparticles. J Control Release. 2009;135:259–67.
Yumoto R, Nishikawa H, Okamoto M, Katayama H, Nagai J, Takano M. Clathrin-mediated endocytosis of FITC-albumin in alveolar type II epithelial cell line RLE-6TN. Am J Physiol Lung Cell Mol Physiol. 2006;290:L946–55.
Arpino G, Gutierrez C, Weiss H, Rimawi M, Massarweh S, Bharwani L, et al. Treatment of human epidermal growth factor receptor 2-overexpressing breast cancer xenografts with multiagent HER-targeted therapy. J Natl Cancer Inst. 2007;99:694–705.
Michalke B. Platinum speciation used for elucidating activation or inhibition of Pt-containing anti-cancer drugs. J Trace Elem Med Biol. 2010;24:69–77.
Olszewskiand U, Hamilton G. A better platinum-based anticancer drug yet to come? Anticancer Agents Med Chem. 2010;10:293–301.
Kelland L. The resurgence of platinum-based cancer chemotherapy. Nat Rev Cancer. 2007;7:573–84.
Shen DW, Akiyama S, Schoenlein P, Pastan I, Gottesman MM. Characterisation of high-level cisplatin-resistant cell lines established from a human hepatoma cell line and human KB adenocarcinoma cells: cross-resistance and protein changes. Br J Cancer. 1995;71:676–83.
Mercerand J, Helenius A. Virus entry by macropinocytosis. Nat Cell Biol. 2009;11:510–20.
Whitehead CM, Earle KA, Fetter J, Xu S, Hartman T, Chan DC, et al. Exisulind-induced apoptosis in a non-small cell lung cancer orthotopic lung tumor model augments docetaxel treatment and contributes to increased survival. Mol Cancer Ther. 2003;2:479–88.
Chan DC, Earle KA, Zhao TL, Helfrich B, Zeng C, Baron A, et al. Exisulind in combination with docetaxel inhibits growth and metastasis of human lung cancer and prolongs survival in athymic nude rats with orthotopic lung tumors. Clin Cancer Res. 2002;8:904–12.
Loftsson T, Konradsdottir F, Masson M. Influence of aqueous diffusion layer on passive drug diffusion from aqueous cyclodextrin solutions through biological membranes. Pharmazie. 2006;61:83–9.
Schinkeland AH, Jonker JW. Mammalian drug efflux transporters of the ATP binding cassette (ABC) family: an overview. Adv Drug Deliv Rev. 2003;55:3–29.
Danieland H, Kottra G. The proton oligopeptide cotransporter family SLC15 in physiology and pharmacology. Pflugers Arch. 2004;447:610–8.
Hagenbuchand B, Meier PJ. Organic anion transporting polypeptides of the OATP/SLC21 family: phylogenetic classification as OATP/SLCO superfamily, new nomenclature and molecular/functional properties. Pflugers Arch. 2004;447:653–65.
Koepselland H, Endou H. The SLC22 drug transporter family. Pflugers Arch. 2004;447:666–76.
Parkar NS, Akpa BS, Nitsche LC, Wedgewood LE, Place AT, Sverdlov MS, et al. Vesicle formation and endocytosis: function, machinery, mechanisms, and modeling. Antioxid Redox Signal. 2009;11:1301–12.
Beltingand M, Wittrup A. Developments in macromolecular drug delivery. Methods Mol Biol. 2009;480:1–10.
Zhang Q, Hong M, Duan P, Pan Z, Ma J, You G. Organic anion transporter OAT1 undergoes constitutive and protein kinase C-regulated trafficking through a dynamin- and clathrin-dependent pathway. J Biol Chem. 2008;283:32570–9.
Jiang W, Prokopenko O, Wong L, Inouye M, Mirochnitchenko O. IRIP, a new ischemia/reperfusion-inducible protein that participates in the regulation of transporter activity. Mol Cell Biol. 2005;25:6496–508.
Kroiss M, Leyerer M, Gorboulev V, Kuhlkamp T, Kipp H, Koepsell H. Transporter regulator RS1 (RSC1A1) coats the trans-Golgi network and migrates into the nucleus. Am J Physiol Renal Physiol. 2006;291:F1201–12.
Filatova A, Leyerer M, Gorboulev V, Chintalapati C, Reinders Y, Muller TD, et al. Novel shuttling domain in a regulator (RSC1A1) of transporter SGLT1 steers cell cycle-dependent nuclear location. Traffic. 2009;10:1599–618.
Korn T, Kuhlkamp T, Track C, Schatz I, Baumgarten K, Gorboulev V, et al. The plasma membrane-associated protein RS1 decreases transcription of the transporter SGLT1 in confluent LLC-PK1 cells. J Biol Chem. 2001;276:45330–40.
Zhuand B, Strada SJ. The novel functions of cGMP-specific phosphodiesterase 5 and its inhibitors in carcinoma cells and pulmonary/cardiovascular vessels. Curr Top Med Chem. 2007;7:437–54.
Thompson WJ, Piazza GA, Li H, Liu L, Fetter J, Zhu B, et al. Exisulind induction of apoptosis involves guanosine 3′,5′-cyclic monophosphate phosphodiesterase inhibition, protein kinase G activation, and attenuated beta-catenin. Cancer Res. 2000;60:3338–42.
Eguchi K, Nakanishi S, Takagi H, Taoufiq Z, Takahashi T. Maturation of a PKG-dependent retrograde mechanism for exoendocytic coupling of synaptic vesicles. Neuron. 2012;74:517–29.
Scrima M, De Marco C, De Vita F, Fabiani F, Franco R, Pirozzi G, et al. The nonreceptor-type tyrosine phosphatase PTPN13 is a tumor suppressor gene in non-small cell lung cancer. Am J Pathol. 2012;180:1202–14.
ACKNOWLEDGMENTS AND DISCLOSURES
The present study was supported by the National Institute of General Medical Sciences of the US National Institutes of Health (NIH) under Award R01GM099742, and by the US Food and Drug Administration (FDA) under Award U01FD004320. Qing Li received research support from National Natural Science Foundation (NNSF) of China (81001445). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH, FDA and NNSF.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, Q., Shu, Y. Pharmacological Modulation of Cytotoxicity and Cellular Uptake of Anti-cancer Drugs by PDE5 Inhibitors in Lung Cancer Cells. Pharm Res 31, 86–96 (2014). https://doi.org/10.1007/s11095-013-1134-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-013-1134-0