ABSTRACT
Purpose
To determine the impact of skin pretreatment with microneedles (MNs) on ALA- and MAL-induced protoporphyrin IX (PpIX) production, as well as MN impact on pain sensations during light exposure and erythema after PDT.
Methods
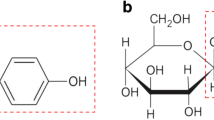
The skin of 14 healthy volunteers was preteated with MNs. Equal amounts of creams containing 2%, 8% and 16% (w/w) ALA and MAL were applied on 1 cm2 areas for 4 h. Additionally, 16% ALA and MAL creams were applied for 24 h. Afterwards, PpIX fluorescence spectra were measured. Sixteen percent ALA and MAL spots were exposed to red light (632 nm, 77 mW/cm2). Time for pain to occur was measured in seconds, and erythemal response was monitored up to 6 h after the end of the light exposure.
Results
Use of MNs increased the PpIX fluorescence after 4 h incubation time with 2% and 8% ALA or MAL, but not with 16% ALA or MAL. Pretreatment with MNs did not increase the pain sensations during light exposure, nor did it influence erythema occurrence.
Conclusions
MNs are a promising tool for improving the efficiency of topical PDT by improving the cutaneous delivery of ALA and MAL, without increase in side effects.





Similar content being viewed by others

REFERENCES
Fien SM, Oseroff AR. Photodynamic therapy for non-melanoma skin cancer. J Natl Compr Canc Netw. 2007;5:531–40.
Braathen LR, Szeimies RM, Basset-Seguin N, et al. Guidelines on the use of photodynamic therapy for nonmelanoma skin cancer: an international consensus. International Society for Photodynamic Therapy in Dermatology, 2005. J Am Acad Dermatol. 2007;56:125–43.
Pizinger K, Cetkovska P, Kacerovska D, Kumpova M. Successful treatment of cutaneous leishmaniasis by photodynamic therapy and cryotherapy. Eur J Dermatol. 2009;19:172–3.
Kamp H, Tietz HJ, Lutz M, et al. Antifungal effect of 5-animolevulinic acid PDT in Trychophyton rubrum. Mycoses. 2005;48:101–7.
Rossi R, Bruscino N, Ricceri F, Grazzini M, Dindelli M, Lotti T. Photodynamic treatment for viral infections of the skin. Ital Dermatol Venereol. 2009;144:79–83.
Lee JW, Kim BJ, Kim MN. Photodynamic therapy: new treatment for recelcitrant Malassezia folliculitis. Lasers Surg Med. 2010;42:192–6.
Yin R, Hao F, Deng J, Yang XC, Yan H. Investigation of optimal ALA concentration applied in topical ALA-PDT for treatment of moderate to severe acne: a pilot study on Chinese people. Br J Dermatol. 2010; doi:10.1111/j.1365-2133.2010.09860.
Gholam P, Denk K, Sehr T, Enk A, Hartmann M. Factors influencing pain intensity during topical photodynamic therapy of complete cosmetic units for actinic keratoses. J Am Acad Dermatol. 2010;63:213–8.
Arits AH, van de Weert MM, Nelemans PJ, Kelleners-Smeets NW. Pain during topical photodynamic therapy: uncomfortable and unpredictable. J Eur Acad Dermatol Venereol 2010; doi:10.1111/j.1468-3083.2010.03670.
Svaasand LO, Wyss P, Wyss MT, Tadir Y, Tromberg BJ, Berns MW. Dosimetry model for photodynamic therapy with topically administered photosensitizers. Lasers Surg Med. 1996;18:139–49.
van den Akker JT, Iani V, Star WM, Sterenborg HJ, Moan J. Topical application of 5-aminolevulinic acid hexyl ester and 5-aminolevulinic acid to normal nude mouse skin: differences in protoporphyrin IX fluorescence kinetics and the role of the stratum corneum. Photochem Photobiol. 2000;72:681–9.
Donnelly RF, McCarron PA, Woolfson AD. Drug delivery of aminolevulinic acid from topical formulations intended for photodynamic therapy. Photochem Photobiol. 2005;81:750–67.
Kasche A, Luderschmidt S, Ring J, Hein R. Photodynamic therapy induces less pain in patients treated with methyl aminolevulinate compared to aminolevulinic acid. J Drugs Dermatol. 2006;5:353–6.
Wiegell SR, Stender IM, Na R, Wulf HC. Pain associated with photodynamic therapy using 5-aminolevulinic acid or 5-aminolevulinic acid methylester on tape-stripped normal skin. Arch Dermatol. 2003;139:1173–7.
Wiegell SR, Wulf HC. Photodynamic therapy of acne vulgaris using 5-aminolevulinic acid versus methyl aminolevulinate. J Am Acad Dermatol. 2006;54:647–51.
Kuijpers DI, Thissen MR, Thissen CA, Neumann MH. Similar effectiveness of methyl aminolevulinate and 5-aminolevulinate in topical photodynamic therapy for nodular basal cell carcinoma. J Drugs Dermatol. 2006;5:642–5.
Donnelly RF, Morrow DIJ, McCarron PA, et al. Microneedle-mediated intradermal delivery of 5-aminolevulinic acid: potential for enhanced topical photodynamic therapy. J Control Release 2008;129:154–62.
Donnelly RF, Cassidy CM, Loughlin RG, et al. Delivery of methylene blue and meso-tetra (N-methyl-4-pyridyl) porphine tetra tosylate from cross-linked poly(vinyl alcohol) hydrogels: a potential means of photodynamic therapy of infected wounds. J Photochem Photobiol B. 2009;96:223–31.
Chabri F, Bouris K, Jones T, et al. Microfabricated silicon microneedles for nonviral cutaneous gene delivery. Br J Dermatol. 2004;150:869–77.
Donnelly RF, Singh TR., Tunney MM, et al. Microneedle arrays allow lower microbial penetration than hypodermic needles in vitro. Pharm Res. 2009;26:2513–22.
Haq MI, Smith E, John DN, et al. Clinical administration of microneedles: skin puncture, pain and sensation. Biomed Microdevices. 2009;11:35–47.
Bal SM, Caussin J, Pavel S, Bouwstra JA. In vivo assessment of safety of microneedle arrays in human skin. Eur J Pharm Sci. 2008;35:193–202.
Fluhr JW, Kuss O, Diepgen T, et al. Testing for irritation with a multifactorial approach: comparison of eight non-invasive measuring techniques on five different irritation types. Br J Dermatol. 2001;145:696–703.
Egekvist H, Bjerring P, Arendt-Nielsen L. Pain and mechanical injury of human skin following needle insertions. Eur J Pain. 1999;3:41–9.
Bond JR, Barry BW. Hairless mouse skin is limited as a model for assessing the effects of penetration enhancers in human skin. J Invest Dermatol. 1988;90:810–3.
Lee JW, Yoo KH, Kim BJ, Kim MN. Photodynamic therapy with methyl 5-aminolevulinate acid combined with microneedle treatment in patients with extensive alopecia areata. Clin Exp Dermatol. 2010;35:548–9.
Touma DJ, Gilchrest BA. Topical photodynamic therapy: a new tool in cosmetic dermatology. Semin Cutan Med Surg. 2003;22:124–30.
Donnelly RF, Majithiya R, Thakur RRS, et al. Design, optimization and characterisation of polymeric microneedle arrays prepared by a novel laser-based micromoulding technique. Pharm Res. 2009; doi:10.1007/s11095-010-0169-8.
Moriyama EM, Kim A, Bogaards A, Lilge L, Wilson BCA. Ratiometric fluorescence imaging system for surgical guidance. Adv Opt Tech. 2008;2008:1–10.
Clarys P, Alewaeters K, Lambrecht R, Barel AO. Skin color measurements: comparison between three instruments: the ChromameterA, the DermaSpectrometerA and the MexameterA. Skin Res Technol. 2000;6:230–8.
Prausnitz MR, Luderschmidt S. Transdermal drug delivery. Nat Biotechnol. 2008;26:1261–8.
Brown MB, Traynor MJ, Martin GP, Akomeah FK. Transdermal drug delivery systems: skin perturbation devices. Methods Mol Biol. 2008;437:119–39.
Singh S, Singh J. Transdermal drug delivery by passive diffusion and iontophoresis: a review. Med Res Rev. 1993;13:569–621.
Moser K, Kriwet K, Naik A, Kalia YN, Guy RH. Passive skin penetration enhancement and its quantification in vitro. Eur J Pharm Biopharm. 2001;52:103–12.
Corsini E, Galli CL. Epidermal cytokines in experimental contact dermatitis. Toxicology. 2000;142:203–11.
Busch TM, Hahn SM, Evans SM, Koch CJ. Depletion of tumor oxygenation during photodynamic therapy: detection by the hypoxia marker EF3 [2-(2-nitroimidazol-1[H]-yl)-N-(3, 3, 3-trifluoropropyl)acetamide]. Cancer Res. 2000;60:2636–42.
Busch TM. Local physiological changes during photodynamic therapy. Lasers Surg Med. 2006;38:494–9.
Kaushik S, Hord AH, Denson DD, et al. Lack of pain associated with microfabricated microneedles. Anesth Analg. 2001;92:502–4.
Henry S, McAllister DV, Allen MG, Prausnitz MR. Microfabricated microneedles: a novel approach to transdermal drug delivery. J Pharm Sci. 1998;87:922–5.
McCarron PA, Donnelly RF, Andrews AD, Woolfson AD. Stability of 5-aminolevulinic acid in novel non-aqueous gel and patch-type systems intended for topical application. J Pharm Sci. 2005;94:1756–71.
ACKNOWLEDGEMENTS
The volunteer aspect of this work was supported by the Norwegian Cancer Society (Det Norske Kreftforening). The microneedles aspect of this work was supported by BBSRC grant number BB/E020534/1 and Invest Northern Ireland Proof of Concept grant number POC21A.
CONFLICT OF INTEREST
The manuscript contains original data which are not published or intended to publish elsewhere. We state no conflicts of interests or of financial nature or others.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mikolajewska, P., Donnelly, R.F., Garland, M.J. et al. Microneedle Pre-treatment of Human Skin Improves 5-Aminolevulininc Acid (ALA)- and 5-Aminolevulinic Acid Methyl Ester (MAL)-Induced PpIX Production for Topical Photodynamic Therapy Without Increase in Pain or Erythema. Pharm Res 27, 2213–2220 (2010). https://doi.org/10.1007/s11095-010-0227-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-010-0227-2