Abstract
Purpose
To determine the intestinal disposition mechanisms of paeoniflorin, a bioactive glucoside, and to investigate the mechanisms by which sinomenine increases paeoniflorin bioavailability.
Materials and Methods
A single-pass “four-site” rat intestinal perfusion model and a cultured Caco-2 cell model were employed.
Results
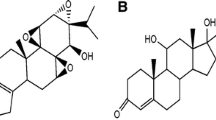
In both model systems, paeoniflorin permeability was poor. In the perfusion model, maximal absorption and metabolism of paeoniflorin occurred in duodenum and jejunum, which were significantly decreased by a glucosidase inhibitor gluconolactone (20 mM). On the other hand, paeoniflorin absorption in terminal ileum increased significantly but its metabolism did not in the presence of sinomenine and cyclosporine A. In the Caco-2 cell model, paeoniflorin was transported 48-fold slower than its aglycone (paeoniflorigenin). Absorptive transport of paeoniflorin was significantly (p < 0.05) increased by sinomenine (38%), verapamil (27%), and cyclosporine A (41%), whereas its secretory transport was significantly (p < 0.01) decreased by sinomenine (50%), verapamil (35%) and cyclosporine A (37%). In contrast, MRP inhibitors MK-571 and leukotriene C4 did not affect transport of paeoniflorin. Lastly, sinomenine was also shown to significantly increase the absorptive transport of digoxin (a prototypical p-glycoprotein substrate) and to significantly decrease its secretory transport.
Conclusions
Poor permeation, p-gp-mediated efflux, and hydrolysis via a glucosidase contributed to the poor bioavailability of paeoniflorin. Sinomenine (an inhibitor of the p-gp-mediated digoxin efflux) increased paeoniflorin's bioavailability via the inhibition of p-gp-mediated paeoniflorin efflux in the intestine.








Similar content being viewed by others
References
J. Yamahara, T. Yamada, H. Kimura, T. Sawada, and H. Fujimura. Biologically active principles of crude drug. II. Anti-allergic principles in “Shoseir-yu-To” anti-inflammatory properties of paeoniflorin and its derivatives. J. Pharmacobio-Dyn. 5:921–929 (1982).
M. Kimura, I. Kimura, and H. Nojima. Depolarizing neuromuscular blocking action induced by electropharmacological coupling in the combined effect of paeoniflorin and glycyrrhizin. Jpn. J. Pharmacol. 37:395–397 (1984).
S. Takeda, T. Isono, Y. Wakui, Y. Matsuzaki, H. Sasaki, and S. Amagaya. Absorption and excretion of paeoniflorin in rats. J. Pharm. Pharmacol. 47:1036–1040 (1995).
S. Takeda, T. Isono, Y. Wakui, Y. Mizuhara, S. Amagaya, M. Maruno, and M. Hattori. In-vivo assessment of extrahepatic metabolism of paeoniflorin in rats: relevance to intestinal floral metabolism. J. Pharm. Pharmacol. 49:35–39 (1997).
Z. Q. Liu, H. Zhou, L. Liu, Z. H. Jiang, Y. F. Wong, Y. Xie, X. Cai, H. X. Xu, and K. C. Chan. The pharmacokinetic fate of paeoniflorin influenced by co-administration of sinomenine in unrestrained conscious rats. J. Ethnopharmaco. 99:61–67 (2005).
L. C. Chen, M. H. Lee, M. H. Chou, M. F. Lin, and L. L. Yang. Pharmacokinetic study of paeoniflorin in mice after oral administration of Paeoniae radix extract. J. Chromatogr. B. 735:33–40 (1999).
L. C. Chen, M. H. Chou, M. F. Lin, and L. L. Yang. Pharmacokinetics of paeoniflorin after oral administration of Shao-yao Gan-cha Tang in mice. Jpn. J. Pharmacol. 88:250–255 (2002).
S. L. Hsiu, Y. T. Lin, K. C. Wen, Y. C. Hou, and P. D. Chao. A deglucosylated metabolite of paeoniflorin of the root of Paeonia lactiflora and its pharmacokinetics in rats. Planta Med. 69:1113–1118 (2003).
M. Hattori, Y. Z. Shu, M. Shimizu, T. Hayashi, N. Morita, X. G. Kobashi, and T. Namba. Metabolism of paeoniflorin and related compounds by human intestinal bacteria. Chem. Pharm. Bull. 33:3838–3846 (1985).
Y. Z. Shu, M. Hattori, T. Akao, K. Kobashi, K. Kagi, K. Fukuyama, T. Tsukihara, and T. Namba. Metabolism of paeoniflorin and related compounds by human intestinal bacteria. II. Structures of 7S-and 7R-paeonimetabolines I and II formed by Bacteroides fragillis and Lactobacillus brevis. Chem. Pharm. Bull. 35:2733– 3726 (1987).
K. Chan, Z. Q. Liu, Z. H. Jiang, H. Zhou, Y. F. Wong, H. X. Xu, and L. Liu. The effects of sinomenine on intestinal absorption of paeoniflorin by everted rat gut sac model. J. Ethnopharmacol. 103:425–432 (2006).
Z. Tai, and S. J. Hopkins. Sinomenine: antiarthritic antiinflammatory. Drugs Future 23:45–49 (1998).
L. Liu, J. Riese, K. Resch, and V. Kaever. Impairment of macrophage eicosanoid and nitric oxide production by sinomenine, an alkaloid from Sinomenium acutum. Arzneim.-Forsch. 44(11):1223–1226 (1994).
B. Vieregge, K. Resch, and V. Kaever. Synergistic effects of the alkaloid sinomenine in combination with the immunosuppressive drugs tacrolimus and mycophenolic acid. Planta Med. 44:1223–1226 (1999).
L. Liu, K. Resch, and V. Kaever. Inhibition of lymphocyte proliferation by the anti-rheumatic drug sinomenine. Int. J. Immunopharmacol. 16:685–691 (1996).
M. Hu, J. Chen, D. Tran, Y. Zhu, and G. Lenonardo. The Caco-2 cell monolayers as an intestinal metabolism model: metabolism of dipeptide Phe-Pro. J. Drug Target. 2:79–89 (1994).
M. Hu, J. Chen, Y. Zhu, A. H. Dantzig, R. E. Stratford, and M. T. Kuhfeld. Mechanism and kinetics of transcellular transport of a new β-lactam antibiotic loracarbef across an human intestinal epithelial model system (Caco-2). Pharm. Res.(NY) 11:1405–1413 (1994).
J. Chen, H. Lin, and M. Hu. Metabolism of flavonoids via enteric recycling: role of intestinal disposition. J. Pharmacol. Exp. Ther. 304:1228–1235 (2003).
E. J. Jeong, X. B. Jia, and M. Hu. Disposition of formononetin via enteric recycling: metabolism and excretion in mouse intestinal perfusion and Caco-2 cell model. Mol. Pharmacol. 2:319–328 (2005).
E. J. Jeong, Y. Liu, H. Lin, and M. Hu. In situ single-pass perfused rat intestinal model for absorption and metabolism. In Z. Yan and G. W. Caldwell (eds.), In Methods in Pharmacology and Toxicology: Optimization in Drug Discovery—In Vitro Methods, Human, Totowa, NJ, 2004, pp. 65–76.
M. Hu, K. Ge, L. Roland, J. Chen, P. Tyle, and S. Roy. Determination of absorption characteristics of AG337, a novel thymidylate synthase inhibitor, using a perfused rat intestinal model. J. Pharm. Sci. 87:886–890 (1998).
M. Hu, P. J. Sinko, A. L. J. DeMeere, D. A. Johnson, and G. L. Amidon. Membrane permeability parameters for some amino acids and β-lactam antibiotics: application of the boundary layer approach. J. Theor. Biol. 131:107–114 (1988).
T. Tanaka, S. Takase, and T. Goda. A possible role of a nuclear factor NF-LPH1 in the regional expression of lactase-phlorizin hydrolase along the small intestine. J. Nutr. Sci. Vitaminol. (Tokyo) 43:565–573 (1997).
E. Liang, J. Proudfoot, and M. Yazdanian. Mechanisms of transport and structure–permeability relationship of sulfasalazine and its analogs in Caco-2 cell monolayers. Pharm. Res. 17:1168–1174 (2000).
Y. Liu, Y. Liu, Y. Dai, L. Y. Xun, and M. Hu. Enteric disposition and recycling of flavonoids and ginkgo flavonoids. J. Altern. Complement. Med. 9:631–640 (2003).
Y. Zhang, A. Gupta, H. Wang, L. Zhou, R. R. Vethanayagam, J. D. Unadkat, and Q. Mao. BCRP transports dipyridamole and is inhibited by calcium channel blockers. Pharm. Res. 22:2023–2034 (2005).
G. T. Ho, F. M. Moodie, and J. Satsangi. Multidrug resistance 1 gene (P-glycoprotein 170): an important determinant in gastrointestinal disease? Gut 52:759–766 (2003).
R. Tian, N. Koyabu, H. Takanaga, H. Matsuo, H. Ohtani, and Y. Sawada. Effects of grapefruit juice and orange juice on the intestinal efflux of P-glycoprotein substrates. Pharm. Res. 19:802–809 (2002).
Y. Tanaka, A. L. Slitt, T. M. Leazer, J. M. Maher, and C. D. Klaassen. Tissue distribution and hormonal regulation of the breast cancer resistance protein (Bcrp/Abcg2) in rats and mice. Biochem. Biophys. Res. Commun. 326:181–187 (2005).
B. M. Johnson, P. Zhang, J. D. Schuetz, and K. L. Brouwer. Characterization of transport protein expression in multidrug resistance-associated protein (mrp) 2-deficient rats. Drug Metab. Dispos. 34:556–562 (2006).
Acknowledgments
This work was supported by grants (ZQL, LL, ZHJ) of JCICM-6-02 from the Hong Kong Jockey Club Charities Trust of Hong Kong and of CA-87779 (MH) from the National Institutes of Health, USA. This work was conducted at University of Houston, College of Pharmacy during a research visit by ZQL. The authors wish to thank Drs. Hong Xi Xu and Hua Zhou for their supports and comments to this work.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Liu, Z.Q., Jiang, Z.H., Liu, L. et al. Mechanisms Responsible for Poor Oral Bioavailability of Paeoniflorin: Role of Intestinal Disposition and Interactions with Sinomenine. Pharm Res 23, 2768–2780 (2006). https://doi.org/10.1007/s11095-006-9100-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-006-9100-8