Abstract
Background
Elevated serum alkaline phosphatase has been previously studied as a biomarker for progression of metastatic disease and implicated in adverse skeletal events and worsened survival. The purpose of this study was to determine if serum alkaline phosphatase was a predictor of short-term mortality of patients undergoing surgery for spinal metastatic disease.
Methods
The American College of Surgeons National Surgical Quality Improvement Program was queried for patients undergoing spinal surgery for metastatic disease. Bivariate and multivariable analyses was undertaken to determine the relationship between serum alkaline phosphatase and 30-day mortality.
Results
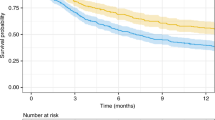
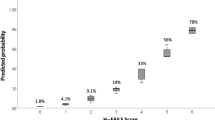
For the 1788 patients undergoing operative intervention for spinal metastatic disease between 2009 and 2016 the 30-day mortality was 8.49% (n = 151). In patients who survived beyond 30-days after surgery, n = 1627 (91.5%) the median [interquartile range] serum alkaline phosphatase levels were 126.4 [75–138], whereas in patients who had 30-day mortality, the serum alkaline phosphatase levels were 179.8 [114–187]. The optimal cut-off for alkaline phosphatase was determined to be 113 IU/L. On multivariable analysis, elevated serum alkaline phosphatase levels were associated with 30-day mortality (OR 1.61, 95% CI 1.12–2.32, p = 0.011).
Conclusion
Elevated preoperative serum alkaline phosphatase is a marker for 30-day mortality in patients undergoing surgery for spinal metastatic disease. Future retrospective and prospective study designs should incorporate assessment of this serum biomarker to better understand the role for serum alkaline phosphatase in improving prognostication in spinal metastatic disease.


Similar content being viewed by others
References
Barzilai O, Laufer I, Yamada Y et al (2017) Integrating evidence-based medicine for treatment of spinal metastases into a decision framework: neurologic, oncologic, mechanicals stability, and systemic disease. J Clin Oncol 35(21):2419–2427
Roodman GD (2004) Mechanisms of bone metastasis. N Engl J Med 350(16):1655–1664
Patchell RA, Tibbs PA, Regine WF et al (2005) Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet 366(9486):643–648
Kang EJ, Lee SY, Kim HJ et al (2016) Prognostic factors and skeletal-related events in patients with small cell lung cancer with bone metastases at the time of diagnosis. Oncology 90(2):103–111
Brown JE, Cook RJ, Lipton A, Costa L, Coleman RE (2010) Prognostic factors for skeletal complications from metastatic bone disease in breast cancer. Breast Cancer Res Treat 123(3):767–779
Von Elm E, Altman DG, Egger M et al (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 4(10):e296
Collins GS, Reitsma JB, Altman DG, Moons KG (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMC Med 13(1):1
McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM (2006) REporting recommendations for tumor MARKer prognostic studies (REMARK). Breast Cancer Res Treat 100(2):229–235
Raval MV, Pawlik TM (2018) Practical guide to surgical data sets: national surgical quality improvement program (NSQIP) and pediatric NSQIP. JAMA Surg. https://doi.org/10.1001/jamasurg.2018.0486
Karhade AV, Larsen AMG, Cote DJ, Dubois HM, Smith TR (2017) National databases for neurosurgical outcomes research: options, strengths, and limitations. Neurosurgery. https://doi.org/10.1093/neuros/nyx408
Hussain AK, Vig KS, Cheung ZB et al (2017) The impact of metastatic spinal tumor location on 30-day perioperative mortality and morbidity after surgical decompression. Spine (Phila Pa 1976) 43:E648–E655
Schoenfeld AJ, Le HV, Marjoua Y et al (2016) Assessing the utility of a clinical prediction score regarding 30-day morbidity and mortality following metastatic spinal surgery: the New England Spinal Metastasis Score (NESMS). Spine J 16(4):482–490
Sarkiss CA, Hersh EH, Ladner TR et al (2018) Risk factors for thirty-day morbidity and mortality in extradural lumbar spine tumor resection. World Neurosurg 114:e1101–e1106
Karhade AV, Vasudeva VS, Dasenbrock HH et al (2016) Thirty-day readmission and reoperation after surgery for spinal tumors: a National Surgical Quality Improvement Program analysis. Neurosurg Focus 41(2):E5
López-Ratón M, Cadarso-Suárez C, Gude-Sampedro F (2014) OptimalCutpoints: an R package for selecting optimal cutpoints in diagnostic tests. J Stat Softw 61:1–36
Stekhoven DJ, Bühlmann P (2011) MissForest—non-parametric missing value imputation for mixed-type data. Bioinformatics 28(1):112–118
Verlaan JJ, Choi D, Versteeg A et al (2016) Characteristics of patients who survived < 3 months or > 2 years after surgery for spinal metastases: can we avoid inappropriate patient selection? J Clin Oncol 34(25):3054–3061
Schoenfeld AJ, Leonard DA, Saadat E, Bono CM, Harris MB, Ferrone ML (2016) Predictors of 30- and 90-day survival following surgical intervention for spinal metastases: a prognostic study conducted at four academic centers. Spine (Phila Pa 1976) 41(8):E503–E509
Achbarou A, Kaiser S, Tremblay G et al (1994) Urokinase overproduction results in increased skeletal metastasis by prostate cancer cells in vivo. Cancer Res 54(9):2372–2377
Berruti A, Dogliotti L, Bitossi R et al (2000) Incidence of skeletal complications in patients with bone metastatic prostate cancer and hormone refractory disease: predictive role of bone resorption and formation markers evaluated at baseline. J Urol 164(4):1248–1253
Tartter PI, Slater G, Gelernt I, Aufses AH Jr (1981) Screening for liver metastases from colorectal cancer with carcinoembryonic antigen and alkaline phosphatase. Ann Surg 193(3):357–360
Kohne CH, Cunningham D, Di Costanzo F et al (2002) Clinical determinants of survival in patients with 5-fluorouracil-based treatment for metastatic colorectal cancer: results of a multivariate analysis of 3825 patients. Ann Oncol 13(2):308–317
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest to disclose.
Ethical approval
The HIPPA-compliant de-identified NSQIP database has been exempted from individual review by our institutional review board.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Karhade, A.V., Thio, Q.C.B.S., Ogink, P.T. et al. Serum alkaline phosphatase and 30-day mortality after surgery for spinal metastatic disease. J Neurooncol 140, 165–171 (2018). https://doi.org/10.1007/s11060-018-2947-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-018-2947-9