Abstract
Background
The Appalachian region is a large geographic and economic area, representing 7.69% of the United States (US). This region is more rural, whiter, older, and has a higher level of poverty as compared to the rest of the US. Limited research has been done on primary brain and other central nervous system tumors (PBT) epidemiology in this region. In this analysis we characterize incidence, mortality, and survival patterns.
Methods
Data from 2006 to 2015 were obtained from the central brain tumor registry of the US (provided by CDC and NCI). Appalachian counties were categorized using the Appalachia Regional Council scheme. Overall and histology-specific age-adjusted incidence and mortality rates per 100,000 population were generated. 1-, 5-, and 10-year relative survival (RS) was estimated using CDC national program of cancer registry data from 2001 to 2014.
Results
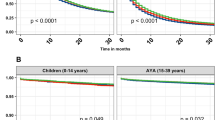
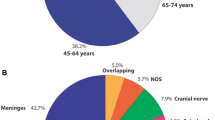
Overall PBT incidence within Appalachia was 22.62 per 100,000, which is not significantly different from the non-Appalachian US (22.77/100,000, p = 0.1189). Malignant incidence was 5% higher in Appalachia (7.55/100,000 vs. 7.23/100,000, p < 0.0001), while non-malignant incidence was 3% lower (15.07/100,000 vs. 15.54/100,000, p < 0.0001). 5-year RS for malignant PBT was lower (31.4% vs. 36.0%), and mortality due to malignant PBT was higher in Appalachia (4.86/100,000 vs. 4.34/100,000, p < 0.0001).
Conclusion
Appalachia has increased malignant and decreased non-malignant PBT incidence, and poorer survival outcomes for malignant PBT compared to the non-Appalachian US.


Similar content being viewed by others
References
Ostrom QT, Gittleman H, Liao P, Vecchione-Koval T, Wolinsky Y, Kruchko C, Barnholtz-Sloan JS (2017) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2010–2014. Neuro Oncol 19:v1–v88
Leece R, Xu J, Ostrom QT, Chen Y, Kruchko C, Barnholtz-Sloan JS (2017) Global incidence of malignant brain and other central nervous system tumors by histology, 2003–2007. Neuro Oncol 19:1553–1564. https://doi.org/10.1093/neuonc/nox091
Ostrom QT, Bauchet L, Davis FG, Deltour I, Fisher JL, Langer CE, Pekmezci M, Schwartzbaum JA, Turner MC, Walsh KM, Wrensch MR, Barnholtz-Sloan JS (2014) The epidemiology of glioma in adults: a “state of the science” review. Neuro Oncol 16:896–913. https://doi.org/10.1093/neuonc/nou087
Amirian ES, Ostrom QT, Liu Y, Barnholtz-Sloan J, Bondy ML (2017) Nervous System. In: Thun M, Linet MS, Cerhan JR, Haiman CA, Schottenfeld D (eds) Cancer epidemiology and prevention, 4 edn. Oxford University Press, New York
Appalachian Regional Commission Counties in Appalachia. https://www.arc.gov/appalachian_region/CountiesinAppalachia.asp
Marshall JL, Thomas L, Lane NM, Arcury TA, Randolph R, Silberman P, Holding W, Villamil L, Sharita T, Lane M, Latus J, Rodgers J, Ivey K (2017) Health disparities in appalachia. Creating a culture of health in appalachia. Appalachian Regional Commission. The University of North Carolina at Chapel Hill, Chapel Hill
Pollard K, Jacobsen LA, Population Reference Bureau (2017) The Appalachian Region: A Data Overview from the 2011–2015 American Community Survey. Population Reference Bureau
McGarvey EL, Leon-Verdin M, Killos LF, Guterbock T, Cohn WF (2011) Health disparities between Appalachian and non-Appalachian counties in Virginia USA. J Community Health 36:348–356. https://doi.org/10.1007/s10900-010-9315-9
Borak J, Salipante-Zaidel C, Slade MD, Fields CA (2012) Mortality disparities in Appalachia: reassessment of major risk factors. J Occup Environ Med 54:146–156. https://doi.org/10.1097/JOM.0b013e318246f395
Meit M, Heffernan M, Tanenbaum E, Hoffmann T, The Walsh Center for Rural Health Analysis (2007) Final report: appalachian diseases of despair. https://www.arc.gov/assets/research_reports/AppalachianDiseasesofDespairAugust2017.pdf
Lengerich EJ, Tucker TC, Powell RK, Colsher P, Lehman E, Ward AJ, Siedlecki JC, Wyatt SW (2005) Cancer incidence in Kentucky, Pennsylvania, and West Virginia: disparities in Appalachia. J Rural Health 21:39–47
Wilson RJ, Ryerson AB, Singh SD, King JB (2016) Cancer incidence in Appalachia, 2004–2011. Cancer Epidemiology, Biomarkers Prev 25:250–258 https://doi.org/10.1158/1055-9965.Epi-15-0946
Yao N, Alcala HE, Anderson R, Balkrishnan R (2017) Cancer disparities in rural Appalachia: incidence, early detection, and survivorship. J Rural Health 33:375–381. https://doi.org/10.1111/jrh.12213
Paskett ED, Fisher JL, Lengerich EJ, Schoenberg NE, Kennedy SK, Conn ME, Roberto KA, Dwyer SK, Fickle D, Dignan M (2011) Disparities in underserved white populations: the case of cancer-related disparities in Appalachia. Oncologist 16:1072–1081. https://doi.org/10.1634/theoncologist.2011-0145
Fisher JL, Engelhardt HL, Stephens JA, Smith BR, Haydu GG, Indian RW, Paskett ED (2008) Cancer-related disparities among residents of Appalachia Ohio. J Health Disparities Res Pract 2:61–74
Huang B, Luo A, Durbin EB, Lycan E, Tucker T, Chen Q, Horbinski C, Villano JL (2017) Incidence of CNS tumors in Appalachian children. J Neurooncol 132:507–512. https://doi.org/10.1007/s11060-017-2403-2
Aldrich TE, Freitas SJ, Ling L, McKinney P (2008) Brain cancer survival in Kentucky: 1996–2000. J Ky Med Assoc 106:489–493
U.S. Cancer Statistics Working Group (2018) United States Cancer Statistics: 1999–2015 Incidence and Mortality Web-based Report. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute,. http://www.cdc.gov/uscs
Appalachian Regional Commission Subregions in Appalachia. https://www.arc.gov/research/MapsofAppalachia.asp?MAP_ID=31
Surveillance Epidemiology and End Results (SEER) Program (2016) SEER*Stat software version 8.3.2. National Cancer Institute, DCCPS, Surveillance Research Program. http://www.seer.cancer.gov/seerstat
Fay MP, Tiwari RC, Feuer EJ, Zou Z (2006) Estimating average annual percent change for disease rates without assuming constant change. Biometrics 62:847–854. https://doi.org/10.1111/j.1541-0420.2006.00528.x
Surveillance Epidemiology and End Results (SEER) Program SEER*Stat Database: Mortality - All COD, Aggregated With State, Total U.S. (1969–2015) < Katrina/Rita Population Adjustment>, National Cancer Institute, DCCPS, Surveillance Research Program, Surveillance Systems Branch, released April 2018. Underlying mortality data provided by NCHS (http://www.cdc.gov/nchs).
Surveillance Epidemiology and End Results (SEER) Program overview of the SEER program. Natl Cancer Inst http://seer.cancer.gov/about/overview.html
Surveillance Epidemiology and End Results (SEER) Program (2015) Number of Persons by Race and Hispanic Ethnicity for SEER Participants (2010 Census Data). http://seer.cancer.gov/registries/data.html
Surveillance Epidemiology and End Results (SEER) Program (2017) SEER*Stat Database: Incidence - SEER 18 Regs Custom Data (with additional treatment fields), Nov 2016 Sub (2000–2014) < Katrina/Rita Population Adjustment> - Linked To County Attributes - Total U.S., 1969–2015 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, released April 2017, based on the November 2016 submission.
Noone AM, Lund JL, Mariotto A, Cronin K, McNeel T, Deapen D, Warren JL (2016) Comparison of SEER treatment data with medicare claims. Med Care 54:e55–e64. https://doi.org/10.1097/mlr.0000000000000073
R Core Team (2018) R: A language and environment for statistical computing. R Foundation for Statistical Computing. http://www.R-project.org/
Program JR, Version 4.2.0.2 - June 2015; Statistical methodology and applications branch, surveillance research program, National Cancer Institute
Ostrom QT, Cote DJ, Ascha M, Kruchko C, Barnholtz-Sloan JS (2018) Adult Glioma Incidence and Survival by Race or Ethnicity in the United States from 2000 to 2014. JAMA Oncol https://doi.org/10.1001/jamaoncol.2018.1789
Porter AB, Lachance DH, Johnson DR (2015) Socioeconomic status and glioblastoma risk: a population-based analysis. Cancer Causes Control: CCC 26:179–185. https://doi.org/10.1007/s10552-014-0496-x
Khanolkar AR, Ljung R, Talback M, Brooke HL, Carlsson S, Mathiesen T, Feychting M (2016) Socioeconomic position and the risk of brain tumour: a Swedish national population-based cohort study. J Epidemiol Community Health. https://doi.org/10.1136/jech-2015-207002
Plascak JJ, Fisher JL (2013) Area-based socioeconomic position and adult glioma: a hierarchical analysis of surveillance epidemiology and end results data. PLoS ONE 8:e60910. https://doi.org/10.1371/journal.pone.0060910
Wigertz A, Lonn S, Hall P, Feychting M (2010) Non-participant characteristics and the association between socioeconomic factors and brain tumour risk. J Epidemiol Community Health 64:736–743. https://doi.org/10.1136/jech.2008.085845
Deb S, Pendharkar AV, Schoen MK, Altekruse S, Ratliff J, Desai A (2017) The effect of socioeconomic status on gross total resection, radiation therapy and overall survival in patients with gliomas. J Neuro-Oncol 132:447–453. https://doi.org/10.1007/s11060-017-2391-2
Nilsson J, Holgersson G, Jaras J, Bergstrom S, Bergqvist M (2018) The role of income in brain tumor patients: a descriptive register-based study: no correlation between patients’ income and development of brain cancer. Med Oncol 35:52. https://doi.org/10.1007/s12032-018-1108-5
Megwalu UC (2017) Impact of county-Level socioeconomic status on oropharyngeal cancer survival in the United States. Otolaryngol–Head Neck Surg 156:665–670. https://doi.org/10.1177/0194599817691462
Underwood JM, Richards TB, Henley SJ, Momin B, Houston K, Rolle I, Holmes C, Stewart SL (2015) Decreasing trend in tobacco-related cancer incidence, United States 2005–2009. J Community Health 40:414–418. https://doi.org/10.1007/s10900-014-9951-6
Woolley SM, Meacham SL, Balmert LC, Talbott EO, Buchanich JM (2015) Comparison of mortality disparities in central Appalachian coal- and non-coal-mining counties. J Occup Environ Med 57:687–694. https://doi.org/10.1097/jom.0000000000000435
Krometis LA, Gohlke J, Kolivras K, Satterwhite E, Marmagas SW, Marr LC (2017) Environmental health disparities in the central Appalachian region of the United States. Rev Environ Health 32:253–266. https://doi.org/10.1515/reveh-2017-0012
Ferdosi H, Lamm SH, Afari-Dwamena NA, Dissen E, Chen R, Li J, Feinleib M (2018) Small-for-gestational age prevalence risk factors in central Appalachian states with mountain-top mining. Int J Occup Med Environ Health 31:11–23. https://doi.org/10.13075/ijomeh.1896.01042
Spector LG, Puumala SE, Carozza SE, Chow EJ, Fox EE, Horel S, Johnson KJ, McLaughlin CC, Reynolds P, Von Behren J, Mueller BA (2009) Cancer risk among children with very low birth weight. Pediatrics 124:96–104. https://doi.org/10.1542/peds.2008-3069
Shiels MS, Engels EA, Linet MS, Clarke CA, Li J, Hall HI, Hartge P, Morton LM (2013) The epidemic of non-Hodgkin lymphoma in the United States: disentangling the effect of HIV, 1992–2009. Cancer Epidemiol Biomark Prev 22:1069–1078. https://doi.org/10.1158/1055-9965.epi-13-0040
Moorman JP, Krolikowski MR, Mathis SM, Pack RP (2018) HIV/HCV Co-infection: burden of disease and care strategies in Appalachia. Curr HIV/AIDS Rep. https://doi.org/10.1007/s11904-018-0404-1
Hall HI, Li J, McKenna MT (2005) HIV in predominantly rural areas of the United States. J Rural Health 21:245–253
Macleod LC, Cannon SS, Ko O, Schade GR, Wright JL, Lin DW, Holt SK, Gore JL, Dash A (2018) Disparities in access and regionalization of care in testicular cancer. Clin Genitourin Cancer 16:e785–e793. https://doi.org/10.1016/j.clgc.2018.02.014
Bos D, Poels MM, Adams HH, Akoudad S, Cremers LG, Zonneveld HI, Hoogendam YY, Verhaaren BF, Verlinden VJ, Verbruggen JG, Peymani A, Hofman A, Krestin GP, Vincent AJ, Feelders RA, Koudstaal PJ, van der Lugt A, Ikram MA, Vernooij MW (2016) Prevalence, clinical management, and natural course of incidental findings on brain mr images: the population-based rotterdam scan study. Radiology 281:507–515. https://doi.org/10.1148/radiol.2016160218
Ezzat S, Asa SL, Couldwell WT, Barr CE, Dodge WE, Vance ML, McCutcheon IE (2004) The prevalence of pituitary adenomas: a systematic review. Cancer 101:613–619. https://doi.org/10.1002/cncr.20412
Morris Z, Whiteley WN, Longstreth WT Jr, Weber F, Lee YC, Tsushima Y, Alphs H, Ladd SC, Warlow C, Wardlaw JM, Al-Shahi Salman R (2009) Incidental findings on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ 339:b3016. https://doi.org/10.1136/bmj.b3016
Bruner JM, Louis DN, McLendon R, Rosenblum MK, Archambault WT, Most S, Tihan T (2017) The utility of expert diagnosis in surgical neuropathology: analysis of consultations reviewed at 5 national comprehensive cancer network institutions. J Neuropathol Exp Neurol 76:189–194. https://doi.org/10.1093/jnen/nlw122
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131:803–820. https://doi.org/10.1007/s00401-016-1545-1
Acknowledgements
This work was previously presented at the 2018 annual meeting of the Society for Neuro-Oncology.
Funding
QTO is supported by a Research Training Grant from the Cancer Prevention and Research Institute of Texas (CPRIT; RP160097T). Funding for CBTRUS was provided by the Centers for Disease Control and Prevention (CDC) under Contract No. 2016-M-9030, the American Brain Tumor Association, The Sontag Foundation, Novocure, Abbvie, the Musella Foundation, and the National Cancer Institute (NCI) under contract No. HHSN261201800176P, as well as private and in kind donations. Contents are solely the responsibility of the authors and do not necessarily reflect the official views of the CDC or the NCI.
Author information
Authors and Affiliations
Contributions
Conceptualization: QTO. Formal analysis: QTO. Data curation: QTO, HG. Writing—original draft: QTO. Writing - review and editing: QTO, HG, CK, JSB. Funding acquisition: CK, JSB.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the Institutional Review Board at University Hospitals Cleveland Medical Center.
Informed consent
This was a retrospective study using de-identified national cancer registries. Thus, formal consent was not required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ostrom, Q.T., Gittleman, H., Kruchko, C. et al. Primary brain and other central nervous system tumors in Appalachia: regional differences in incidence, mortality, and survival. J Neurooncol 142, 27–38 (2019). https://doi.org/10.1007/s11060-018-03073-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-018-03073-z