Abstract
Silent corticotroph staining pituitary adenoma (SCA) represents an uncommon subset of Non-Functioning adenomas (NFAs), hypothesized to be more locally aggressive. In this retrospective multicenter study, we investigate the safety and effectiveness of Stereotactic Radiosurgery (SRS) in patients with SCA compared with other non-SCA NFA’s. Eight centers participating in the International Gamma-Knife Research Foundation (IGKRF) contributed to this study. Outcomes of 50 patients with confirmed SCAs and 307 patients with confirmed non-SCA NFA’s treated with SRS were evaluated. Groups were matched. SCA was characterized by a lack of clinical evidence of Cushing disease, yet with positive immunostaining for corticotroph. Median age was 55.2 years (13.7–87). All patients underwent at least one trans-sphenoidal tumor resection prior to SRS. SRS parameters were comparable as well. Median follow-up 40 months (6-163). Overall tumor control rate (TCR) 91.2% (n = 280). In the SCA group, TCR were 82% (n = 41) versus 94.1% (n = 289) for the control-NFA (p = 0.0065). The SCA group showed a significantly higher incidence of new post-SRS visual deficit (p < 0.0001) assigned to tumor progression and growth, and post-SRS weakness and fatigue (p < 0.0001). In univariate and multivariate analysis, only the status of silent corticotroph staining (p = 0.005, p = 0.009 respectively) and margin dose (p < 0.0005, p = 0.0037 respectively) significantly influenced progression rate. A margin dose of ≥17 Gy was noted to influence the adenoma progression rate in the entire cohort (p = 0.003). Silent corticotroph staining represents an independent factor for adenoma progression and hypopituitarism after SRS. A higher margin dose may convey a greater chance of TCR.


Similar content being viewed by others
References
Dekkers OM, Pereira AM, Romijn JA (2008) Treatment and follow-up of clinically nonfunctioning pituitary macroadenomas. J Clin Endocrinol Metab 93:3717–3726
Melmed S (2006) Medical progress: acromegaly. N Engl J Med 355:2558–2573
Vance ML (2004) Treatment of patients with a pituitary adenoma: one clinician’s experience. Neurosurg Focus 16:E1
Sheehan JP, Xu Z, Lobo MJ (2012) External beam radiation therapy and stereotactic radiosurgery for pituitary adenomas. Neurosurg Clin N Am 23:571–586
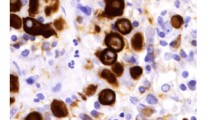
Kovacs K, Horvath E, Bayley TA, Hassaram ST, Ezrin C (1978) Silent corticotroph cell adenoma with lysosomal accumulation and crinophagy. A distinct clinicopathologic entity. Am J Med 64:492–499
Horvath E, Kovacs K, Killinger DW, Smyth HS, Platts ME, Singer W (1980) Silent corticotropic adenomas of the human pituitary gland: a histologic, immunocytologic, and ultrastructural study. Am J Pathol 98:617–638
Xu Z, Ellis S, Lee CC, Starke RM, Schlesinger D, Lee Vance M et al (2014) Silent corticotroph adenomas after stereotactic radiosurgery: a case-control study. Int J Radiat Oncol Biol Phys 90:903–910
Young WF Jr (2000) Clinically nonfunctioning pituitary adenomas. Humana Press, Totowa
Bradley KJ, Wass JA, Turner HE (2003) Non-functioning pituitary adenomas with positive immunoreactivity for ACTH behave more aggressively than ACTH immunonegative tumours but do not recur more frequently. Clin Endocrinol 58:59–64
Cho HY, Cho SW, Kim SW, Shin CS, Park KS, Kim SY (2010) Silent corticotroph adenomas have unique recurrence characteristics compared with other nonfunctioning pituitary adenomas. Clin Endocrinol 72:648–653
Cooper O, Ben-Shlomo A, Bonert V, Bannykh S, Mirocha J, Melmed S (2010) Silent corticogonadotroph adenomas: clinical and cellular characteristics and long-term outcomes. Horm Cancer 1:80–92
Jahangiri A, Wagner JR, Pekmezci M, Hiniker A, Chang EF, Kunwar S et al (2013) A comprehensive long-term retrospective analysis of silent corticotrophic adenomas versus hormone-negative adenomas. Neurosurgery 73:8–17 (discussion 17–18)
Raverot G, Wierinckx A, Jouanneau E, Auger C, Borson-Chazot F, Lachuer J et al (2010) Clinical, hormonal and molecular characterization of pituitary ACTH adenomas without (silent corticotroph adenomas) and with Cushing’s disease. Eur J Endocrinol 163(1):35–43
Roncaroli F, Scheithauer BW, Young WF, Horvath E, Kovacs K, Kros JM et al (2003) Silent corticotroph carcinoma of the adenohypophysis: a report of five cases. Am J Surg Pathol 27(4):477–486
Scheithauer BW, Jaap AJ, Horvath E, Kovacs K, Lloyd RV, Meyer FB et al (2000) Clinically silent corticotroph tumors of the pituitary gland. Neurosurgery 47:723–729 (discussion 729–730)
Webb KM, Laurent JJ, Okonkwo DO, Lopes MB, Vance ML, Laws ER Jr (2003) Clinical characteristics of silent corticotrophic adenomas and creation of an internet-accessible database to facilitate their multi-institutional study. Neurosurgery 53:1076–1084 (discussion 1084–1085)
Alahmadi H, Lee D, Wilson JR, Hayhurst C, Mete O, Gentili F et al (2012) Clinical features of silent corticotroph adenomas. Acta Neurochir 154:1493–1498
Chen L, White WL, Spetzler RF, Xu B (2011) A prospective study of nonfunctioning pituitary adenomas: presentation, management, and clinical outcome. J Neurooncol 102:129–138
Ioachimescu AG, Eiland L, Chhabra VS, Mastrogianakis GM, Schniederjan MJ, Brat D et al (2012) Silent corticotroph adenomas: Emory University cohort and comparison with ACTH negative nonfunctioning pituitary adenomas. Neurosurgery 71:296–303 (discussion 304)
Sheehan JP, Starke RM, Mathieu D, Young B, Sneed PK, Chiang VL et al (2013) Gamma Knife radiosurgery for the management of nonfunctioning pituitary adenomas: a multicenter study. J Neurosurg 119:446–456
Snell JW, Sheehan J, Stroila M, Steiner L (2006) Assessment of imaging studies used with radiosurgery: a volumetric algorithm and an estimation of its error. Technical note. J Neurosurg 104:157–162
Murad MH, Fernandez-Balsells MM, Barwise A, Gallegos-Orozco JF, Paul A, Lane MA et al (2010) Outcomes of surgical treatment for nonfunctioning pituitary adenomas: a systematic review and meta-analysis. Clin Endocrinol 73(6):777–791
Gopalan R, Schlesinger D, Vance ML, Laws E, Sheehan J (2011) Long-term outcomes after Gamma Knife radiosurgery for patients with a nonfunctioning pituitary adenoma. Neurosurgery 69:284–293
Pollock BE, Cochran J, Natt N, Brown PD, Erickson D, Link MJ et al (2008) Gamma knife radiosurgery for patients with nonfunctioning pituitary adenomas: results from a 15-year experience. Int J Radiat Oncol Biol Phys 70:1325–1329
Cohen-Inbar O, Ramesh A, Xu Z, Vance ML, Schlesinger D, Sheehan JP (2016) Gamma knife radiosurgery in patients with persistent acromegaly or Cushing’s disease: long-term risk of hypopituitarism. Clin Endocrinol 84:524–531
Xu Z, Lee Vance M, Schlesinger D, Sheehan JP (2013) Hypopituitarism after stereotactic radiosurgery for pituitary adenomas. Neurosurgery 72:630–637
Ding D, Starke RM, Sheehan JP (2014) Treatment paradigms for pituitary adenomas: defining the roles of radiosurgery and radiation therapy. J Neurooncol 117:445–457
Hoybye C, Rahn T (2009) Adjuvant Gamma Knife radiosurgery in non-functioning pituitary adenomas; low risk of long-term complications in selected patients. Pituitary 12:211–216
Izawa M, Hayashi M, Nakaya K, Satoh H, Ochiai T, Hori T et al (2000) Gamma Knife radiosurgery for pituitary adenomas. J Neurosurg 93:19–22
Jagannathan J, Sheehan JP, Pouratian N, Laws ER, Steiner L, Vance ML (2007) Gamma Knife surgery for Cushing’s disease. J Neurosurg 106:980–987
Starke RM, Williams BJ, Jane JA Jr, Sheehan JP (2012) Gamma Knife surgery for patients with nonfunctioning pituitary macroadenomas: predictors of tumor control, neurological deficits, and hypopituitarism. J Neurosurg 117:129–135
Funding
This study was completely independently founded. We state that no personal or institutional financial interest exists for drugs, materials, or devices described in our submission.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Dr. Inga S. Grills has stock ownership and serve on the Board of Directors in a company called Greater Michigan Gamma Knife. In addition, Dr. Lunsford is a shareholder and consultant for Elekta AB.
Rights and permissions
About this article
Cite this article
Cohen-Inbar, O., Xu, Z., Lee, Cc. et al. Prognostic significance of corticotroph staining in radiosurgery for non-functioning pituitary adenomas: a multicenter study. J Neurooncol 135, 67–74 (2017). https://doi.org/10.1007/s11060-017-2520-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-017-2520-y