Abstract
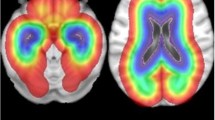
Pediatric high-grade gliomas (pHGGs) occur with strikingly different frequencies in infratentorial and supratentorial regions. Although histologically these malignancies appear similar, they represent distinct diseases. Recent genomic studies have identified histone K27M H3.3/H3.1 mutations in the majority of brainstem pHGGs; these mutations are rarely encountered in pHGGs that arise in the cerebral cortex. Previous research in brainstem pHGGs suggests a restricted permeability of the blood–brain-barrier (BBB). In this work, we use dynamic contrast-enhanced (DCE) MRI to evaluate BBB permeability in a genetic mouse model of pHGG as a function of location (cortex vs. brainstem, n = 8 mice/group) and histone mutation (mutant H3.3K27M vs. wild-type H3.3, n = 8 mice/group). The pHGG models are induced either in the brainstem or the cerebral cortex and are driven by PDGF signaling and p53 loss with either H3.3K27M or wild-type H3.3. T2-weighted MRI was used to determine tumor location/extent followed by 4D DCE-MRI for estimating the rate constant (K trans) for tracer exchange across the barrier. BBB permeability was 67 % higher in cortical pHGGs relative to brainstem pHGGs (t test, p = 0.012) but was not significantly affected by the expression of mutant H3.3K27M versus wild-type H3.3 (t-test, p = 0.78). Although mice became symptomatic at approximately the same time, the mean volume of cortical tumors was 3.6 times higher than the mean volume of brainstem tumors. The difference between the mean volume of gliomas with wild-type and mutant H3.3 was insignificant. Mean K trans was significantly correlated to glioma volume. These results present a possible explanation for the poor response of brainstem pHGGs to systemic therapy. Our findings illustrate a potential role played by the microenvironment in shaping tumor growth and BBB permeability.





Similar content being viewed by others
References
Ostrom QT, Gittleman H, Farah P, Ondracek A, Chen Y, Wolinsky Y, Stroup NE, Kruchko C, Barnholtz-Sloan JS (2013) CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2006–2010. Neuro-Oncology 15:1–56. doi:10.1093/neuonc/not151
Fangusaro J (2012) Pediatric high grade glioma (HGG): a review and update on tumor clinical characteristics and biology. Front Oncol. doi:10.3389/fonc.2012.00105
Cohen KJ, Heideman RL, Zhou T, Holmes EJ, Lavey RS, Bouffet E, Pollack IF (2011) Temozolomide in the treatment of children with newly diagnosed diffuse intrinsic pontine gliomas: a report from the Children’s Oncology Group. Neuro-Oncology 13:410–416. doi:10.1093/neuonc/noq205
Warren K (2012) Diffuse intrinsic pontine glioma: poised for progress. Front Oncol. doi:10.3389/fonc.2012.00205
Sturm D, Witt H, Hovestadt V, Khuong-Quang D-A, Jones David TW, Konermann C, Pfaff E, Tönjes M, Sill M, Bender S, Kool M, Zapatka M, Becker N, Zucknick M, Hielscher T, Liu X-Y, Fontebasso Adam M, Ryzhova M, Albrecht S, Jacob K, Wolter M, Ebinger M, Schuhmann Martin U, van Meter T, Frühwald Michael C, Hauch H, Pekrun A, Radlwimmer B, Niehues T, von Komorowski G, Dürken M, Kulozik Andreas E, Madden J, Donson A, Foreman Nicholas K, Drissi R, Fouladi M, Scheurlen W, von Deimling A, Monoranu C, Roggendorf W, Herold-Mende C, Unterberg A, Kramm Christof M, Felsberg J, Hartmann C, Wiestler B, Wick W, Milde T, Witt O, Lindroth Anders M, Schwartzentruber J, Faury D, Fleming A, Zakrzewska M, Liberski Pawel P, Zakrzewski K, Hauser P, Garami M, Klekner A, Bognar L, Morrissy S, Cavalli F, Taylor Michael D, van Sluis P, Koster J, Versteeg R, Volckmann R, Mikkelsen T, Aldape K, Reifenberger G, Collins VP, Majewski J, Korshunov A, Lichter P, Plass C, Jabado N, Pfister Stefan M (2012) Hotspot mutations in H3F3A and IDH1 define distinct epigenetic and biological subgroups of glioblastoma. Cancer Cell 22:425–437
Schwartzentruber J, Korshunov A, Liu X-Y, Jones DTW, Pfaff E, Jacob K, Sturm D, Fontebasso AM, Quang D-AK, Tonjes M, Hovestadt V, Albrecht S, Kool M, Nantel A, Konermann C, Lindroth A, Jager N, Rausch T, Ryzhova M, Korbel JO, Hielscher T, Hauser P, Garami M, Klekner A, Bognar L, Ebinger M, Schuhmann MU, Scheurlen W, Pekrun A, Fruhwald MC, Roggendorf W, Kramm C, Durken M, Atkinson J, Lepage P, Montpetit A, Zakrzewska M, Zakrzewski K, Liberski PP, Dong Z, Siegel P, Kulozik AE, Zapatka M, Guha A, Malkin D, Felsberg J, Reifenberger G, von Deimling A, Ichimura K, Collins VP, Witt H, Milde T, Witt O, Zhang C, Castelo-Branco P, Lichter P, Faury D, Tabori U, Plass C, Majewski J, Pfister SM, Jabado N (2012) Driver mutations in histone H3.3 and chromatin remodelling genes in paediatric glioblastoma. Nature 482:226–231. doi:10.1038/nature10833
Wu G (2012) Somatic histone H3 alterations in pediatric diffuse intrinsic pontine gliomas and non-brainstem glioblastomas. Nat Genet 44:251–253. doi:10.1038/ng.1102
Schiffman JD, Hodgson JG, VandenBerg SR, Flaherty P, Polley M-YC, Yu M, Fisher PG, Rowitch DH, Ford JM, Berger MS, Ji H, Gutmann DH, James CD (2010) Oncogenic BRAF mutation with CDKN2A inactivation is characteristic of a subset of pediatric malignant astrocytomas. Cancer Res 70:512–519. doi:10.1158/0008-5472.can-09-1851
Paugh BS, Broniscer A, Qu C, Miller CP, Zhang J, Tatevossian RG, Olson JM, Geyer JR, Chi SN, da Silva NS, Onar-Thomas A, Baker JN, Gajjar A, Ellison DW, Baker SJ (2011) Genome-wide analyses identify recurrent amplifications of receptor tyrosine kinases and cell-cycle regulatory genes in diffuse intrinsic pontine glioma. J Clin Oncol 29:3999–4006. doi:10.1200/jco.2011.35.5677
Puget S, Philippe C, Bax DA, Job B, Varlet P, Junier M-P, Andreiuolo F, Carvalho D, Reis R, Guerrini-Rousseau L, Roujeau T, Dessen P, Richon C, Lazar V, Le Teuff G, Sainte-Rose C, Geoerger B, Vassal G, Jones C, Grill J (2012) Mesenchymal transition and PDGFRA amplification/mutation are key distinct oncogenic events in pediatric diffuse intrinsic pontine gliomas. PLoS One 7:e30313. doi:10.1371/journal.pone.0030313
Khuong-Quang D-A, Buczkowicz P, Rakopoulos P, Liu X-Y, Fontebasso A, Bouffet E, Bartels U, Albrecht S, Schwartzentruber J, Letourneau L, Bourgey M, Bourque G, Montpetit A, Bourret G, Lepage P, Fleming A, Lichter P, Kool M, Deimling A, Sturm D, Korshunov A, Faury D, Jones D, Majewski J, Pfister S, Jabado N, Hawkins C (2012) K27M mutation in histone H3.3 defines clinically and biologically distinct subgroups of pediatric diffuse intrinsic pontine gliomas. Acta Neuropathol 124:439–447. doi:10.1007/s00401-012-0998-0
Lewis PW, Muller MM, Koletsky MS, Cordero F, Lin S, Banaszynski LA, Garcia BA, Muir TW, Becher OJ, Allis CD (2013) Inhibition of PRC2 activity by a gain-of-function H3 mutation found in pediatric glioblastoma. Science 340:857–861. doi:10.1126/science.1232245
Chan KM, Fang D, Gan H, Hashizume R, Yu C, Schroeder M, Gupta N, Mueller S, James CD, Jenkins R, Sarkaria J, Zhang Z (2013) The histone H3.3K27M mutation in pediatric glioma reprograms H3K27 methylation and gene expression. Genes Dev 27:985–990. doi:10.1101/gad.217778.113
Epstein FJ, Farmer J-P (1993) Brain-stem glioma growth patterns. J Neurosurg 78:408–412. doi:10.3171/jns.1993.78.3.0408
Hipp SJ, Steffen-Smith E, Hammoud D, Shih JH, Bent R, Warren KE (2011) Predicting outcome of children with diffuse intrinsic pontine gliomas using multiparametric imaging. Neuro-Oncology 13:904–909. doi:10.1093/neuonc/nor076
Warren KE (2004) NMR spectroscopy and pediatric brain tumors. Oncologist 9:312–318. doi:10.1634/theoncologist.9-3-312
Sugahara T, Korogi Y, Kochi M, Ikushima I, Hirai T, Okuda T, Shigematsu Y, Liang L, Ge Y, Ushio Y, Takahashi M (1998) Correlation of MR imaging-determined cerebral blood volume maps with histologic and angiographic determination of vascularity of gliomas. Am J Roentgenol 171:1479–1486. doi:10.2214/ajr.171.6.9843274
Law M, Yang S, Wang H, Babb JS, Johnson G, Cha S, Knopp EA, Zagzag D (2003) Glioma grading: sensitivity, specificity, and predictive values of perfusion MR imaging and proton MR spectroscopic imaging compared with conventional MR imaging. Am J Neuroradiol 24:1989–1998
Becher OJ, Hambardzumyan D, Walker TR, Helmy K, Nazarian J, Albrecht S, Hiner RL, Gall S, Huse JT, Jabado N, MacDonald TJ, Holland EC (2010) Preclinical evaluation of radiation and perifosine in a genetically and histologically accurate model of brainstem glioma. Cancer Res 70:2548–2557. doi:10.1158/0008-5472.can-09-2503
Barton KL, Misuraca K, Cordero F, Dobrikova E, Min HD, Gromeier M, Kirsch DG, Becher OJ (2013) PD-0332991, a CDK4/6 Inhibitor, significantly prolongs survival in a genetically engineered mouse model of brainstem glioma. PLoS One 8:e77639. doi:10.1371/journal.pone.0077639
Subashi E, Moding EJ, Cofer GP, MacFall JR, Kirsch DG, Qi Y, Allan Johnson G (2013) A comparison of radial keyhole strategies for high spatial and temporal resolution 4D contrast-enhanced MRI in small animal tumor models. Med Phys. doi:10.1118/1.4774050
Fram EK, Herfkens RJ, Johnson GA, Glover GH, Karis JP, Shimakawa A, Perkins TG, Pelc NJ (1987) Rapid calculation of T1 using variable flip angle gradient refocused imaging. Magn Reson Imaging 5:201–208. doi:10.1016/0730-725X(87)90021-X
Loveless ME, Halliday J, Liess C, Xu L, Dortch RD, Whisenant J, Waterton JC, Gore JC, Yankeelov TE (2012) A quantitative comparison of the influence of individual versus population-derived vascular input functions on dynamic contrast enhanced-MRI in small animals. Magn Reson Med 67:226–236. doi:10.1002/mrm.22988
Heilmann M, Kiessling F, Enderlin M, Schad LR (2006) Determination of pharmacokinetic parameters in DCE MRI: consequence of nonlinearity between contrast agent concentration and signal intensity. Invest Radiol 41:536–543
Li K-L, Zhu XP, Waterton J, Jackson A (2000) Improved 3D quantitative mapping of blood volume and endothelial permeability in brain tumors. J Magn Reson Imaging 12:347–357. doi:10.1002/1522-2586(200008)12:2<347:aid-jmri19>3.0.co;2-7
Tofts PS (1997) Modeling tracer kinetics in dynamic Gd-DTPA MR imaging. J Magn Reson Imaging 7:91–101. doi:10.1002/jmri.1880070113
Murase K (2004) Efficient method for calculating kinetic parameters using T1-weighted dynamic contrast-enhanced magnetic resonance imaging. Magn Reson Med 51:858–862. doi:10.1002/mrm.20022
Halvorson KG, Barton KL, Schroeder K, Misuraca KL, Hoeman C, Chung A, Crabtree DM, Cordero FJ, Singh R, Spasojevic I, Berlow N, Pal R, Becher OJ (2015) A high-throughput in vitro drug screen in a genetically engineered mouse model of diffuse intrinsic pontine glioma identifies BMS-754807 as a promising therapeutic agent. PLoS One 10:e0118926. doi:10.1371/journal.pone.0118926
Becher OJ, Holland EC (2006) Genetically engineered models have advantages over xenografts for preclinical studies. Cancer Res 66:3355–3359. doi:10.1158/0008-5472.can-05-3827
Monje M, Mitra SS, Freret ME, Raveh TB, Kim J, Masek M, Attema JL, Li G, Haddix T, Edwards MS, Fisher PG, Weissman IL, Rowitch DH, Vogel H, Wong AJ, Beachy PA (2011) Hedgehog-responsive candidate cell of origin for diffuse intrinsic pontine glioma. Proc Natl Acad Sci USA 108:4453–4458. doi:10.1073/pnas.1101657108
Zhang J, Wu G, Miller C, Tatevossian R, Dalton J, Tang B, Orisme W (2013) Whole-genome sequencing identifies genetic alterations in pediatric low-grade gliomas. Nat Genet 45:602–612. doi:10.1038/ng.2611
Hargrave D, Chuang N, Bouffet E (2008) Conventional MRI cannot predict survival in childhood diffuse intrinsic pontine glioma. J Neurooncol 86:313–319. doi:10.1007/s11060-007-9473-5
Lober R, Cho Y-J, Tang Y, Barnes P, Edwards M, Vogel H, Fisher P, Monje M, Yeom K (2014) Diffusion-weighted MRI derived apparent diffusion coefficient identifies prognostically distinct subgroups of pediatric diffuse intrinsic pontine glioma. J Neurooncol 117:175–182. doi:10.1007/s11060-014-1375-8
McConville P, Hambardzumyan D, Moody JB, Leopold WR, Kreger AR, Woolliscroft MJ, Rehemtulla A, Ross BD, Holland EC (2007) Magnetic resonance imaging determination of tumor grade and early response to temozolomide in a genetically engineered mouse model of glioma. Clin Cancer Res 13:2897–2904. doi:10.1158/1078-0432.ccr-06-3058
Acknowledgments
This work was performed at the Duke Center for In Vivo Microscopy, an NIH/NIBIB National Biomedical Technology Resource Center (P41 EB015897 and 1S10OD010683-01). The authors wish to thank Ms. Sally Zimney for the careful editorial assistance. KGH is supported by NINDS R25 NS065731 (PI John Sampson). OJB is a Rory David Deutsch scholar, is supported by the Damon Runyon Cancer Research Foundation, and K02NS086917.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Ergys Subashi and Francisco J. Cordero have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Subashi, E., Cordero, F.J., Halvorson, K.G. et al. Tumor location, but not H3.3K27M, significantly influences the blood–brain-barrier permeability in a genetic mouse model of pediatric high-grade glioma. J Neurooncol 126, 243–251 (2016). https://doi.org/10.1007/s11060-015-1969-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-015-1969-9